Lung transplantation (LT) is a therapeutic option for patients with non-neoplastic, severe, and irreversible chronic respiratory disease, if all available therapeutic resources have been exhausted. LT continues to grow as a field, with more than 4500 transplants performed worldwide in 2019 at over 260 lung transplant centers.1 Chronic obstructive pulmonary disease (COPD) represents the 30.1% of the total lung transplants performed according to the International Society for Heart and Lung Transplantation (ISHLT).2
Recently, the ISHLT update of the selection of lung transplant candidates includes thrombophilia as a high-risk factor or substantially increased risk of complications.3
It is well known that a prothrombotic state exists after transplantation, and many studies have shown that there is an increased risk of thromboembolic disease.4,5 However, there is very little evidence of lung transplantation outcomes in patients with known thrombophilia. As far as our search has reached, only one case of lung transplantation has been reported in a 19-year-old woman with cystic fibrosis with a heterozygous mutation of the prothrombin gene G20210A, who died 6 months after transplantation, apparently due to an overdose of oxycodone, but no pulmonary artery thromboembolism was evidenced in the postmortem study.6
Case report53-year-old male, old smoker of 50 pack-years 7 years ago, with diagnosis of COPD BODE 7 points, with normal levels of alpha-1 antitrypsin, in functional class 4 of the MRC-m, with chronic global respiratory failure, who was referred for lung transplantation.
In addition, he has a family history of chronic thromboembolic disease: his mother has a protein C deficiency, and a sister with protein C deficiency who died at 28 years of age with acute pulmonary embolism, and another brother with protein C deficiency with pulmonary thromboembolism at age 30.
He had a history of an episode of acute arterial ischemia in the lower right limb in 2003, treated with intravenous prostanoids and subsequently acetylsalicylic acid, and an acute pulmonary embolism in 2010 secondary to a deep vein thrombosis in the right popliteal territory, requiring admission in intensive care. Treatment with acenocoumarol was started. Nine months after the acute embolism, the diagnosis of chronic pulmonary embolism in the right upper lobe was confirmed.
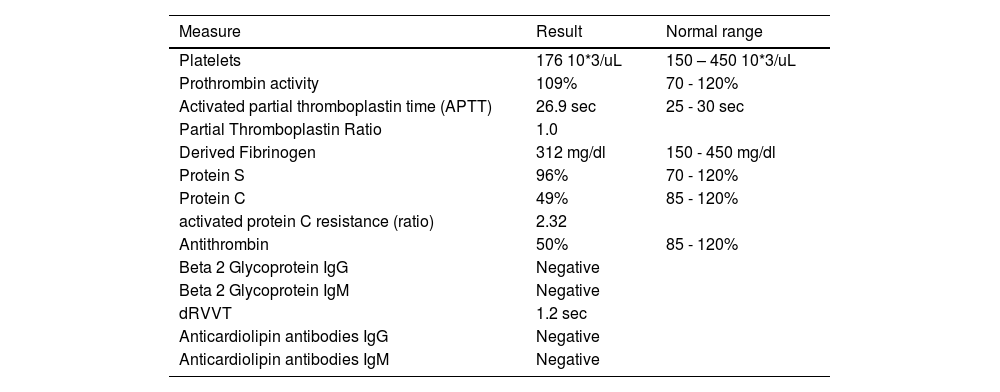
The patient was referred to our hospital in August 2013 as a candidate for a lung transplant. Although he had been studied in the referring hospital, a coagulation study was repeated in our hospital during the pretransplant study. To carry out this study, acenocoumarol was switched to enoxaparin for 4 weeks prior to the hematology study. The complete study is shown in Table 1. The patient did not have other comorbidities such as liver abnormalities or renal failure that could alter these results. With these results of protein C and antithrombin deficiency, his personal and family history, and after being evaluated by a hematologist, the diagnosis of combined thrombophilia was established.
Hypercoagulability study before lung transplant
dRVVT: dilute Russell's viper venom time; sec: seconds.
When he was evaluated for lung transplant, a full evaluation was done. His ventilation/perfusion scintigraphy showed signs of chronic pulmonary embolism in the right upper lobe and left lower lobe, findings that were confirmed by CT scan of the pulmonary arteries. His coronary arteries were normal on coronary angiography, and right heart catheterization demonstrated pulmonary hypertension with pulmonary artery pressures of 45/20/28 mmHg, wedge pressure of 11 mmHg, right atrial pressure of 9 mmHg, and cardiac output of 6.45 liters/minute. In addition, the patient had a severe obstructive ventilatory syndrome, with a ratio of 22.27, an FEV1 of 600 ml (17%) and a FVC of 2700 ml (61%), with global respiratory failure (PaO2 = 52 mmHg and PaCO2 = 47 mmHg) and walked 273 meters in the 6-minute walk test with oxygen added at 5 litres/minute, making two stops and showing desaturation from 97% initial to 77% final.
So, he had a mixed secondary pulmonary hypertension due to respiratory disease (group 3) and chronic thromboembolism (group 4), and he wasn´t considered for surgical treatment of the thrombi or angioplasty balloon due to respiratory comorbidity (COPD).
He had no other contraindications, so he was finally considered for lung transplantation, and he was included in the waiting list in December 2020, and he remained on acenocoumarol treatment until the time of transplantation with an INR (International normalized ratio) between 2.5-3.5.
In February 2021, a double lung transplant was performed. At the moment when he arrived at the hospital for transplantation, his INR was 3.27 and his prothrombin activity was 23%. He received treatment with 10 mg of vitamin K and 20 IU/kg of Octaplex® (human prothrombin complex), achieving adequate reversal of anticoagulation, going to an INR of 1.28 and prothrombin activity of 68% in only 1 h.
A double lung transplant was performed, with basiliximab induction, without significant surgical or anesthetic complications. He was extubated in the first 24 h without problems. Immediately after the transplant, anticoagulation with sodium heparin in continuous infusion was maintained. Heparin doses were adjusted according to Hematology recommendations. After 72 h, without bleeding complications and without problems of thrombosis he was switched to low molecular weight heparin with enoxaparin at a dose of 1 mg/kg every 12 h. In the absence of renal failure, obesity, or complications, the effect of enoxaparin with anti-Xa was not monitored. He was discharged from the ICU after 4 days. After performing a control transbronchial biopsy in the 3rd week after transplantation according to our hospital protocol, treatment with acenocoumarol was started again. He was discharged home 24 days after the transplant.
During the follow-up, he had problems achieving INR stability between 2.5 - 3.5, probably due to interactions with other drugs, so he switched to warfarin, achieving an adequate INR level. Direct-acting anticoagulants were ruled out due to known thrombophilia. At the present time, 11 months after transplantation, he has not had bleeding complications or thrombosis, with an excellent functional class, without relevant complications of any other type.
DiscussionEven though according to the latest recommendations of the ISHLT, patients with thrombophilia are considered at high risk of complications, our case suggests that an adequate selection of the patient, without other significant comorbidities, and with a meticulous management and in collaboration with specialists in hematology, can lead to a successful lung transplant. Because of that, although more experience is needed in performing lung transplants in patients with thrombophilia, some selected cases could be considered as candidates for this treatment option.