Diversity in Classical Hematology Research
More infoAccording to the World Health Organization, trauma from external causes remains the major cause of death and disability among people aged from 5 to 29 years old.1 In order to reestablish hemodynamic stability and adequate hemostasis of these patients, without the dilutional effects of infusing large volumes of crystalloids, the concept of hemostatic resuscitation was developed.2
The purpose of this report is to discuss a case in which hemostatic resuscitation was performed quickly, resulting in a good macro-hemodynamic response of the patient at the first prehospital transfusion service in Latin America.
Case reportA 49-year-old female patient and her son suffered a motorcycle-light pole collision in Bragança Paulista, a city in the inner part of the state of São Paulo, in the southeastern region of Brazil. The patient was on the back of the motorcycle and five minutes after the crash, when the Prehospital Emergency Care arrived at the scene, she was next to the light pole, on a left lateral decubitus. The driver was stable and had no important physical injuries, while the reported patient presented heavy sweating, clammy skin, lightheadedness and an absent radial pulse. The safety of the prehospital care providers was ensured and the Prehospital Trauma Life Support (PHTLS™) XABCDE protocol was performed.
On physical examination, there were no signs of external bleeding. She had pervious airways and spinal motion restriction with a semi rigid cervical collar and a scoop stretcher was performed. Her oxygen saturation was 90% (in ambient air) and at examination there were vesicular breath sounds with fine crackles and fractures of several ribs in the left thoraco-abdominal transition. The patient had pale skin, sweating and cold extremities, capillary refill time was longer than two seconds, heart rate of 150 bpm and the patient's blood pressure was inaudible due to hypotension. On abdominal examination there was left hypochondrium pain but no signs of peritonitis. On pelvic examination there was no sign of instability. The patient was Glasgow Coma Scale (GCS) 14 and did not present any focal neurological signs nor upper limbs fracture, but there were signs of a closed left femur fracture. In relation to preexisting conditions, she had a past medical history of hypertension and no known allergies.
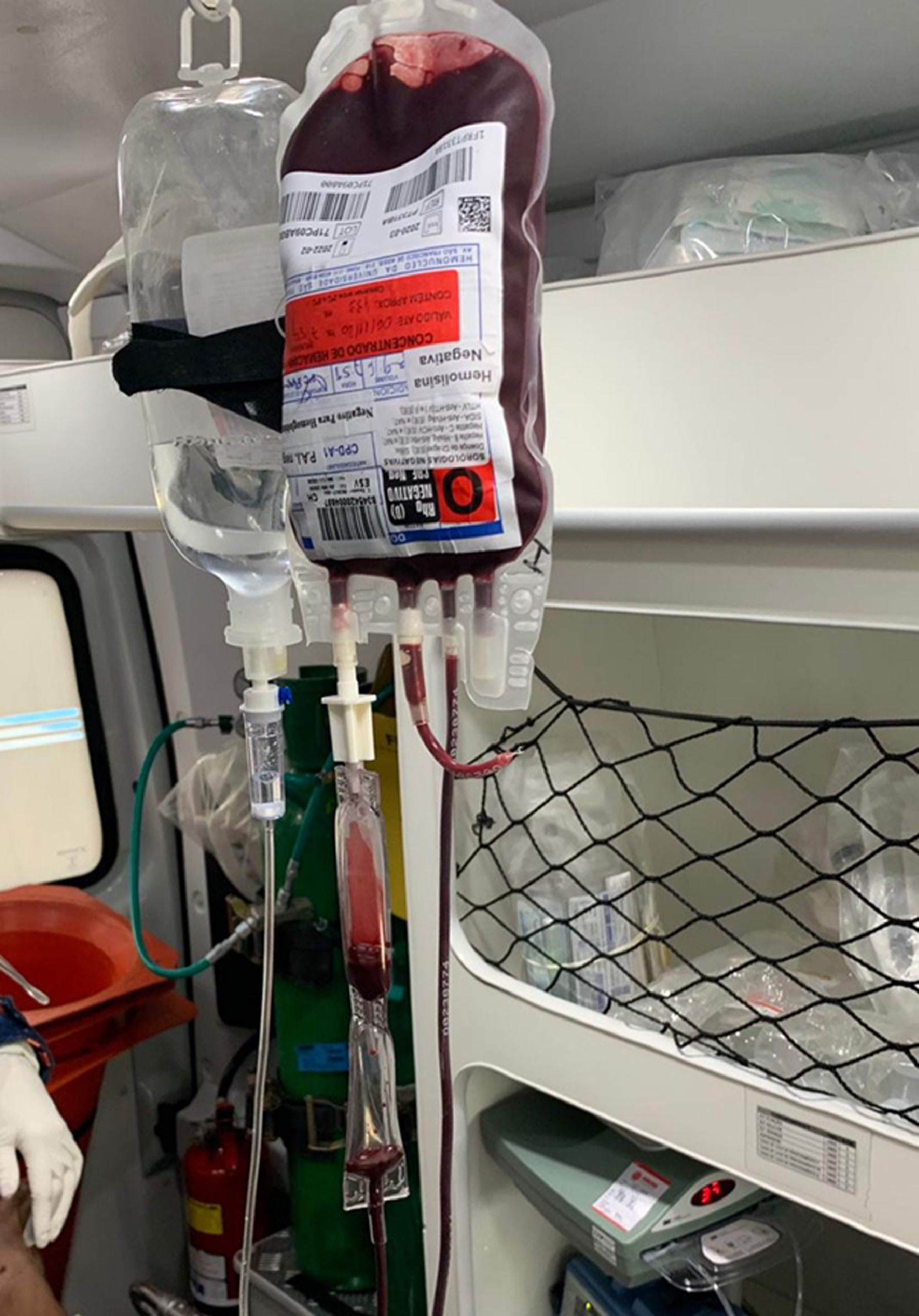
E-FAST was performed during transportation, which demonstrated intra-abdominal free fluid and the presence of a left hemothorax. 100% oxygen was offered with a non rebreather mask and two peripheral venous catheters were placed. 1 g tranexamic acid, 3 g calcium gluconate and fluid resuscitation with 1000 ml crystalloids were administered. The patient met criteria for blood transfusion at the prehospital environment due to hemodynamic instability, 3 out of 4 score on the ABC criteria for trauma and shock index above 1.0. Pre-transfusion blood samples were collected and one heated red blood cell concentrate, ABO ‘O’ and RhD negative, was transfused at the mobile land unit (Figure 1). The transfusion started 10 minutes after the arrival of the mobile unit at the trauma scene and, 16 minutes later, the warmed infusion was completed.
The patient was transported by ground to the São Francisco University Hospital (HUSF), a tertiary referral hospital in Bragança Paulista, in approximately 20 minutes. Upon arrival at the trauma center, the patient's blood pressure was 100 × 60 mmHg and heart rate of 120 bpm, demonstrating a good macro hemodynamic response after fluid and blood resuscitation. Thoracostomy was performed at the ER and the chest tube drainage did not characterize a massive hemothorax, so there was no need for a thoracotomy. An exploratory laparotomy was performed to examine the source of the abdominal bleeding and a splenic rupture was found. The surgical team proceeded to a splenectomy (Figure 2).
DiscussionTrauma is the main cause of death and disability in people from 1 to 44 years, both in Brazil and in other Latin American countries.3,4 In 2017, the Global Burden of Diseases (GBD) estimated that death by trauma represented 8% of the global mortality, with a rate of 57,9 deaths per 100.000 inhabitants,5 being bleeding and hemorrhagic shock the cause of 30 to 40% of those preventable deaths,6 resulting in approximately 75 million years of life lost.7 Therefore, hemorrhagic control and shock stabilization are essential for the prevention of those deaths.
Given the necessity for volume replacement in shock treatment, crystalloid administration has been done aggressively in the last 50 years. However, recent studies show that this excessive use was proven harmful, favoring the worsening of bleeding and death.6 Contrariwise, new researches evidenced the potential benefits of the transfusion of PRBCs, plasma and whole blood at a prehospital environment, bringing better outcomes such as enhanced chances of survival and less need for future transfusions.8,9 This strategy is aligned with the Patient Blood Management approach.
The transfusion of packed red blood cells (PRBCs) was made for the first time during the Vietnam War, in which the military received blood during transit to hospitals in protected areas.10 After that, the first blood transfusion at prehospital care in civilians was registered in 1985 in the United States of America. Since then, the procedure has been implemented in ambulances and helicopters of several emergency care systems around the world.11,12 In Brazil, prehospital blood transfusion was established in September 2020, at a mobile intensive care unit (SAMU 192) in Bragança Paulista, a city in the inner part of the state of São Paulo, being the first in Latin America to offer this kind of procedure.4
As far as we know, this is the first case report in Latin America related to immediate transfusion of PRBCs in prehospital care, being of extreme importance the analysis of the results obtained in the unit as a way of helping and inciting other services to adhere to the strategy. At this first moment, it was decided to provide only RBC concentrates because this blood centre does not produce and distribute units of whole blood, which would require a restructuring not yet available, considering the production and storage logistics. The perspective is that this service can be expanded to use plasma or whole blood units, according to the future availability of the blood bank.
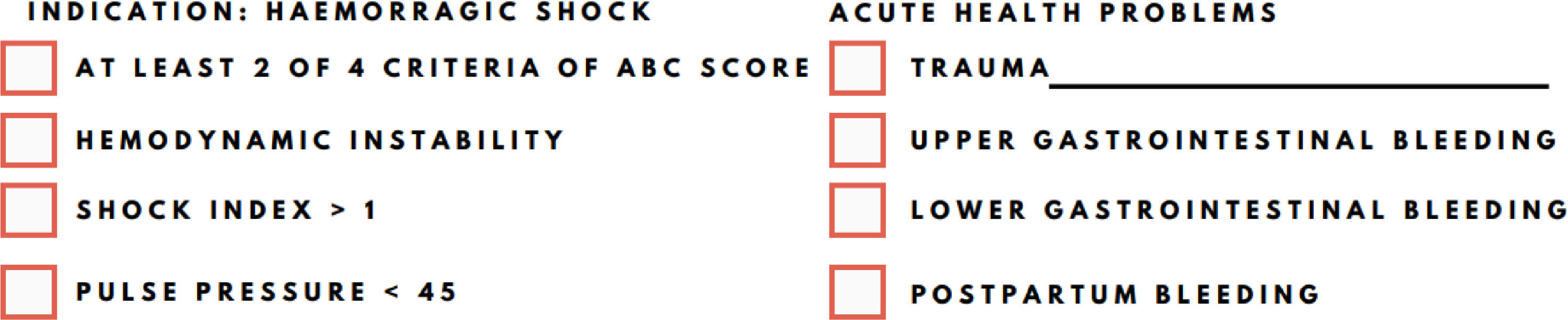
Currently, there is no international agreement about the criteria used for the indication of blood transfusion in a prehospital environment.13 In this context, the criteria used in the service to perform the transfusion was developed by the unit itself, shown in Figure 3, in summary: traumatized adult patients (traumatic cardiorespiratory arrest, firearm injury, stab wound, piercing-cutting wound, polytrauma), or with upper or lower gastrointestinal bleeding or those with puerperal bleeding and hemorrhagic shock, who meet at least 2 out of 4 ABC Score criteria for trauma, presence of signs of hemodynamic instability, shock index > 1 or pulse pressure < 45.4
On the reported case, the patient suffered a blunt mechanical trauma from a motorcycle accident. On the scene, she had a heart rate of 150 bpm, inaudible systolic pressure, therefore, close to zero, and positive E-FAST for free fluid in the abdominal cavity, characterizing 3 of 4 ABC Score criteria.13 Furthermore, the patient had hemodynamic instability signs, such as pale skin, heavy sweating, cold extremities and capillary refill time longer than 2 seconds. Moreover, as blood pressure was very low, the shock index was bigger than 1. Therefore, the transfusion was justified by the presence of trauma and a 3 out of 4 score on the criteria established by the service protocol.
After the transfusion of PRBCs, the patient transitioned from a hemorrhagic shock state, with a very low systolic pressure, to a normotensive one, with a rate of 100 × 60 mmHg. Furthermore, her heart rate dropped significantly, going from 150 to 120 bpm, coming close to normal. Thus, the results analysis demonstrated a good macro hemodynamic response after fluid and blood resuscitation, reverting the critical initial state the patient was found in.
At the hospital, after submission to an exploratory laparotomy to find the primary cause of bleeding, a splenic rupture was found, proven to be one of the main causes of uncontrollable internal bleeding.14 In fact, a study showed that, in the presence of grade III or higher injury, blood transfusion is required in 100% of cases,14 corroborating even more with the importance of the procedure and less need of future transfusions.
ConclusionThis case report describes a patient who underwent prehospital transfusion of PRBCs performed by the mobile intensive care unit (SAMU 192) in Bragança Paulista, southeastern Brazil, after blunt mechanical trauma with splenic involvement and consequent hypovolemic shock. The patient evolved with a good response to treatment, followed by stabilization of vital signs. However, despite the success accomplished, the literature still presents great divergence in relation to the real benefits of the technique in a prehospital environment, showing the need of new studies and trials, in addition to the development of standardized procedures to be followed.
Study approvalThis case report was approved by SAMU 192 Regional Bragança Ethics Committee.
FundingThe charges will be paid by Biothermal Logistics Solutions, a South American Pelican Biothermal representative.
The authors would like to thank Mr. Claudio Moreno Andrade and Mr. Fabio Tadeu Teixeira Martins for their generous support and encouragement during the implementation of the project.