Hemorrhagic shock is the main cause of death in the prehospital environment, which highlights the need to standardize measures aiming at bleeding control and volume replacement in this environment. In Brazil, the first prehospital packed red blood cell transfusion service started in September 2020, in Bragança Paulista, state of São Paulo.
ObjectivesDescribe the trends and characteristics of patients who received prehospital transfusions prior to hospital treatment during the first year of operation.
MethodsA retrospective data review was made of all patients who received transfusions from the mobile intensive care unit in Bragança Paulista over one year.
ResultsIn this period, 19 patients were transfused. Since activation, the average response time was 20 min. The mean shock indexes before and after blood transfusion were 2.16 and 1.1, respectively. During the course of the 1st year of prehospital transfusions, no blood was wasted and there were no adverse effects.
ConclusionIntroduction of the prehospital packed red blood cell transfusion service was successful, with significant improvement in hemodynamic parameters.
Trauma due to external causes accounted for 8 % of the world mortality rate in 2017, and remains to this day the leading cause of disability and death among people aged five to 29 years.1 Moreover, responsible for up to 91 % of the mortality, hemorrhagic shock is the main cause of death in the out-of-hospital environment.2 It is, therefore, necessary to offer fast and effective medical assistance, since people who are critically injured can progress to death in about thirty minutes due to severe bleeding.3 It is essential to establish bleeding control and volume replacement in mobile units in the prehospital environment.
Volume replacement using crystalloids is one of the main procedures performed in prehospital care. However, according to studies carried out by Griggs,4 this technique is associated with higher immediate mortality (within six hours) due to blood loss, and late mortality (within 28 h) due to complications such as multiple organ failure and dilutional coagulopathy, when compared to blood transfusions. Thus, based on military experiments, prehospital services around the world have optimized their care by implementing blood transfusion therapy in their mobile units in order to have more effective hemodynamic control and lower complication rates.5–8
In Brazil, the first prehospital blood transfusion service started in September 2020 in a mobile intensive care unit (SAMU - 192) in Bragança Paulista, a provincial city of the state of São Paulo. This unit covers a total of 11 cities spread over 3219 km2 and a population of approximately 480,600 inhabitants. This was also the first Latin American service to create guidelines and parameters for the use of and to adhere to this procedure.9,10
However, despite the increasing use of blood transfusions in mobile units, further observational studies and research are still needed in order to assess the real effectiveness of this practice in the short and long terms.
ObjectivesThe purpose of this retrospective review is to describe the trends and characteristics of patients who received prehospital transfusions of packed red blood cells (PRBCs) prior to hospital treatment, in order to discuss and to stimulate the possibility of extrapolating this approach to other scenarios. This would include the development of specific protocols for early and safe transfusions all over the world, aiming at reducing deaths in the prehospital setting.
Materials and methodsThis study is a retrospective data review of all patients who received blood products from the mobile intensive care unit (SAMU 192) in Bragança Paulista attending primary missions between 09/14/2020 and 09/14/2021. The information was collected through a review of the patients’ medical records and a review of the scarce literature available on prehospital transfusion outside military settings.
All patients studied received blood transfusions in the prehospital setting because they met the criteria according to the score developed by the service (supplementary Figure 1). The criteria to indicate transfusions were based on different scores used around the world due to the significant concern in avoiding unnecessary transfusions in the prehospital environment. Briefly, adult trauma patients, or those with upper or lower gastrointestinal bleeding, or with obstetrical bleeding, who had at least 2 of 4 ABC Score criteria for trauma, presence of signs of hemodynamic instability, shock index > 1, or pulse pressure < 45 were transfused. A trained physician in emergency care evaluated the ABC score and decided the need for transfusion.
The service in question has the availability, in the ambulance, of two units of PRBCs, ABO “O” and RhD negative that are negative for the presence of Hb S. Both units are reserved for a single patient use. A partnership has been developed between the regional mobile emergency service and the regional blood bank, with the development of protocols for storage, transport, and transfusion of PRBCs in the ambulances. Subsequently, a specific training process was carried out of both the mobile response and blood bank teams. Eleven cities, spread over 3219 km2 are covered by the regional mobile emergency service, a public health system that cares for 480.600 inhabitants. The regional blood bank is found at the São Francisco University Hospital, the main university hospital in the region.
ResultsIn the period from 09/14/2020 to 09/14/2021, a total of 58,379 emergency calls were registered by all mobile response teams. Of these, 1603 responses were attended by the Alfa ambulance, which has a trained physician in emergency care and specific material for the blood transfusion procedure. Of the attendances made by the ambulance, 19 patients (1.9 %) complied with the transfusion criteria developed by the service.
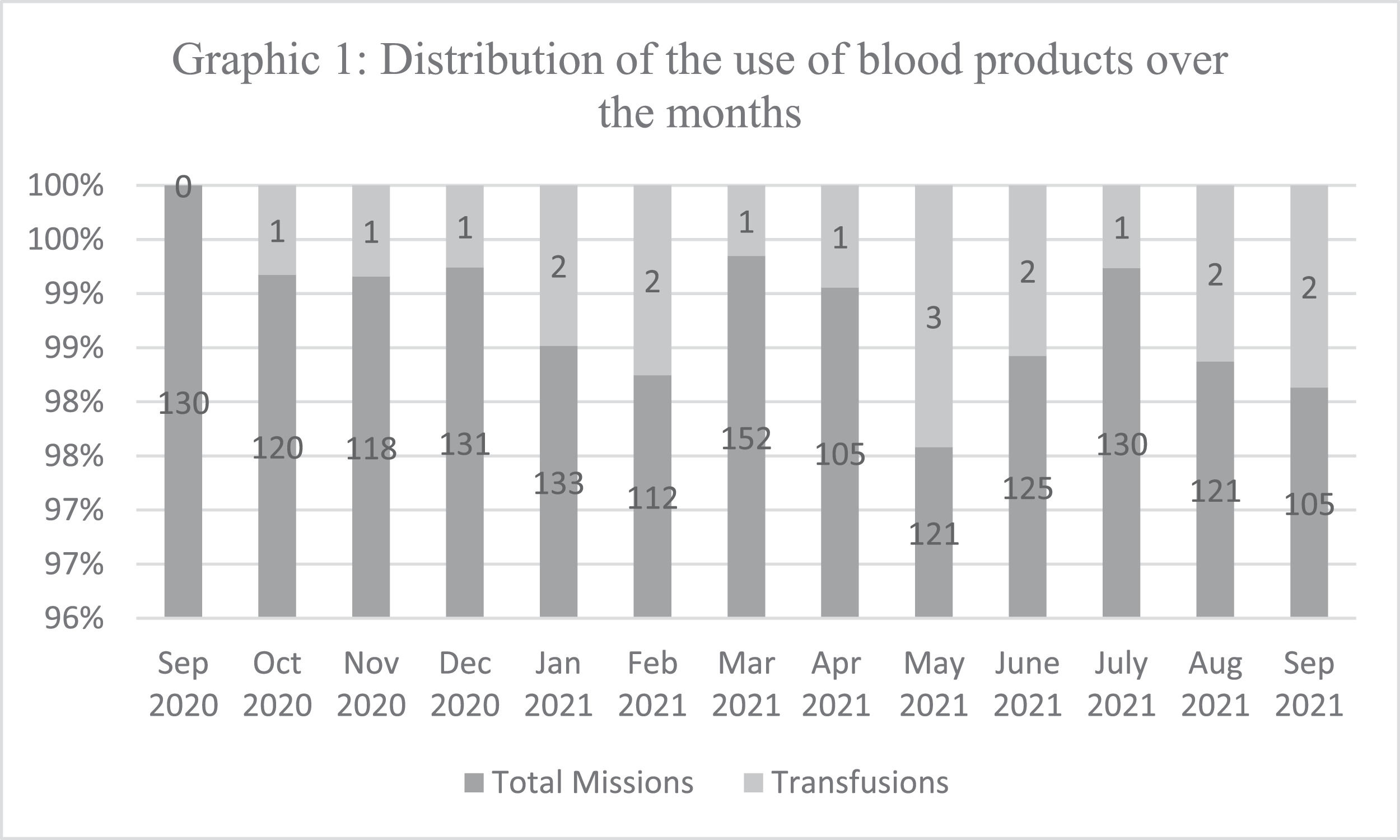
When analyzing the distribution of the use of blood products over the months (Figure 1), there was a 50 % increase of transfusion rates when comparing the periods from September 2020 to March 2021 and from March 2021 to September 2021. Among the transfused patients, 73.68 % (n = 14) were trauma victims, 21.05 % (n = 4) had upper digestive hemorrhages and 5.26 % (n = 1) had obstetrical bleeding. The mean age of the patients was 43.1 years, ranging from 20 to 88 years old. The gender ratio was 15 male to 4 female patients.
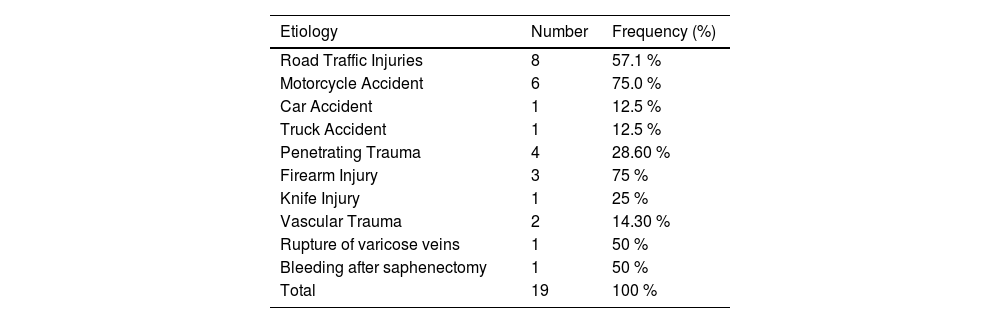
The etiologies of the patients who received PRBCs are described in Table 1. Fourteen patients (57.1 %; n = 8) were victims of road traffic accidents, of which 75 % (n = 6) suffered motorcycle accidents, 12.5 % (n = 1) car accidents, and 12.5 % (n = 1) truck accidents. In addition, 28.6 % (n = 4) of the trauma patients suffered penetrating traumas, of which 75 % (n = 3) suffered a firearm injury and 25 % (n = 1) suffered a stab wound. Of the remaining trauma victims, 14.3 % (n = 2) suffered vascular trauma, one suffered a varicose vein rupture in the left lower limb and one a postoperative hemorrhage from a saphenectomy.
Frequency of etiologies.
| Etiology | Number | Frequency (%) |
|---|---|---|
| Road Traffic Injuries | 8 | 57.1 % |
| Motorcycle Accident | 6 | 75.0 % |
| Car Accident | 1 | 12.5 % |
| Truck Accident | 1 | 12.5 % |
| Penetrating Trauma | 4 | 28.60 % |
| Firearm Injury | 3 | 75 % |
| Knife Injury | 1 | 25 % |
| Vascular Trauma | 2 | 14.30 % |
| Rupture of varicose veins | 1 | 50 % |
| Bleeding after saphenectomy | 1 | 50 % |
| Total | 19 | 100 % |
Since activation, the mean response time was 20 min (range: 2–58 min). Physicians were on the scene with patients for an average of 43 min (range: 10–111 min). The mean travel time from the accident scene to the reference service was 25 min (range: 12–54 min) and the total mission time from activation until the patient's death or arrival at hospital was on average 84 min (range: 20–176 min). Seventeen (89.5 %) of the transfused patients arrived alive at the hospital with only two patients (10.5 %) suffering cardiac arrest.
The vital signs and the shock index of the patients were evaluated before and after the blood transfusion. The mean systolic blood pressure (SBP) on arrival at the accident scene was 52.6 mmHg (range: 0–110), and the mean heart rate (HR) prior to the procedure was 114 beats per minute (range: 0–160). Thus, the mean initial shock index (HR/SBP) was 2.16. After transfusion of PRBCs, the mean systolic blood pressure was 85.2 mmHg (range: 0–120), and the mean heart rate was 93.7 beats per minute (range: 0–150). Thus, the mean final shock index was 1.1.
During the first year, 11 patients (58 %) received one PRBC unit while eight patients (42 %) received two PRBC units. On average, patients received 1360 mL of crystalloids in the prehospital setting. After care (prehospital and hospital), of the 17 transfused patients who arrived alive at the hospital, seven (41 %) were discharged after admission to the intensive care unit (ICU). This implies that, of all the transfused patients (n = 19), more than one-third (36.8 %) were discharged after PRBC transfusions.
Throughout the 1st year of prehospital transfusions, no blood units were discarded due to the expiration date or any other cause (no blood waste). In addition, no adverse effects were reported after the procedure.
DiscussionNineteen cases were recorded in the first year after the introduction of prehospital blood transfusions. This incidence is in line with the world literature when compared to the study by Shand et al.11 who reported 22 cases within the first year. Furthermore, on comparing the periods from September 2020 to March 2021 and from March 2021 to September 2021, there was a 50 % increase in blood transfusion rates. Thus, it can be inferred that the lower rates observed in the first period are related to the restrictions imposed by the COVID-19 pandemic in Brazil, which was responsible for a decrease in traumatic accidents.12 Moreover, with a recent protocol and improved equipment in this service, the increase of the experience of the team with the procedure and the inclusion criteria there is a tendency for the care rates to rise progressively over the next few years.
Traumatic accidents were the main cause for the need of PRBC transfusions in prehospital care, with road traffic injuries being predominant. Hence, corroborating the results found, the retrospective study carried out by Lyon et al.,13 after analyzing 147 patients, concluded that 73 % were related to road traffic collisions and trauma was the reason for 97 % of transfusions. Among non-traumatic events, gastrointestinal bleeding was responsible for the highest transfusion rate. In addition, according to Ichiyanagui Rodríguez, the ratio of upper to lower gastrointestinal bleeding is 83:17, which explains the absence of cases of lower gastrointestinal bleeding in this study.14 Only one case was due to obstetrical hemorrhage.
Efficiency in the transport associated with effective prehospital interventions improves outcomes of patients who suffer hemorrhagic shocks.15 However, the Bragança Paulista mobile care service covers an area of 3219 km2, directly reflecting on the time required for support teams to arrive at the accident scene. The result of this is that the mean time to arrive was 20 min (range: 2–58). The randomized study performed by Meyer et al. concluded that for every minute of delay in the administration of blood products, there is a 5 % increase in the odds of mortality.16 If the prehospital procedure had not been implemented in the region, the patients treated would have received blood products only at hospital, thereby increasing the delay in to receiving PRBCs by an average of 25 min (range: 12–59), not counting the time spent at the scene of the accident (mean: 43 min) and possible delays in the administration of PRBCs.
According to Brown et al.,17 prehospital transfusion of PRBCs was associated with a decrease in the incidence of shock and an improvement in hemodynamic parameters. Greene et al.18 concluded that prehospital transfusion led to a significant increase in SBP and mean blood pressure, besides decreasing the shock index. Similarly, in the present article, after the procedure, improvements in hemodynamic parameters, increases in systemic blood pressure, decreases in HR and decreases in shock index values to close to normal were observed. Furthermore, a 15-minute reduction in hemostasis time is associated with a reduction in 30-day mortality, stressing the importance of early transfusion, which may be related to greater survival than the one third found in the current analysis.19
According to Brazilian law, the direct use of low-titer group O whole blood or thawed plasma in prehospital transfusions is not covered by the current legislation.20,21 On the other hand, the implementation of fresh frozen plasma could lead to a huge waste, a fact that contributed to the choice of PRBCs in the service. Moreover, the blood center does not produce and distribute units of whole blood, a situation that would require restructuring in respect to production and storage logistics. Implementation of the use of plasma or whole blood units is expected depending on a future governmental release.
The present review has some noteworthy limitations. First, due to the relatively small number of patients seen in the year 2021, the final results cannot be extrapolated to a larger sphere. In addition, some medical records had incomplete data, hindering the collection of information. There was also no control group to compare outcomes and parameters, making it difficult to speculate on how effective transfusion in prehospital care is in effect.
ConclusionIn Latin America, the first prehospital PRBC transfusion service started in September 2020 in a provincial city of the state of São Paulo. Over the 1st year of prehospital transfusions, no blood products were wasted and no adverse effects were reported. On evaluating the results, the introduction of prehospital PRBC transfusions was successful, with significant improvement in hemodynamic parameters. This review should be a starting point to expand the implementation of prehospital blood transfusions to other centers in Brazil and Latin America, and also to encourage future studies with a larger number of patients in order to better define the efficacy of prehospital transfusions.