Intravascular large B-cell lymphoma (IVLBCL) is a rare entity characterized by an almost exclusive growth of lymphoid cells within the lumen of blood vessels.1 Accurate diagnosis is particularly challenging because clinical manifestations are variable, and routine laboratory tests are usually non-specific. When affecting the CNS, brain is the most common location, followed by optic nerve, cerebrospinal fluid (CSF) and rarely the spinal cord.2
We present the case of a middle-aged female patient with repeated episodes of fever of unknown origin. She was admitted to the hospital and thorough workups were performed. The only abnormal findings were increased lactate dehydrogenase (LDH) and erythrocyte sedimentation rate (ESR) levels. During hospitalization, she suffered progressive asymmetrical lower limb weakness, analgesia and anesthesia in L5- S1 and sacral roots with complete loss of sphincter control.
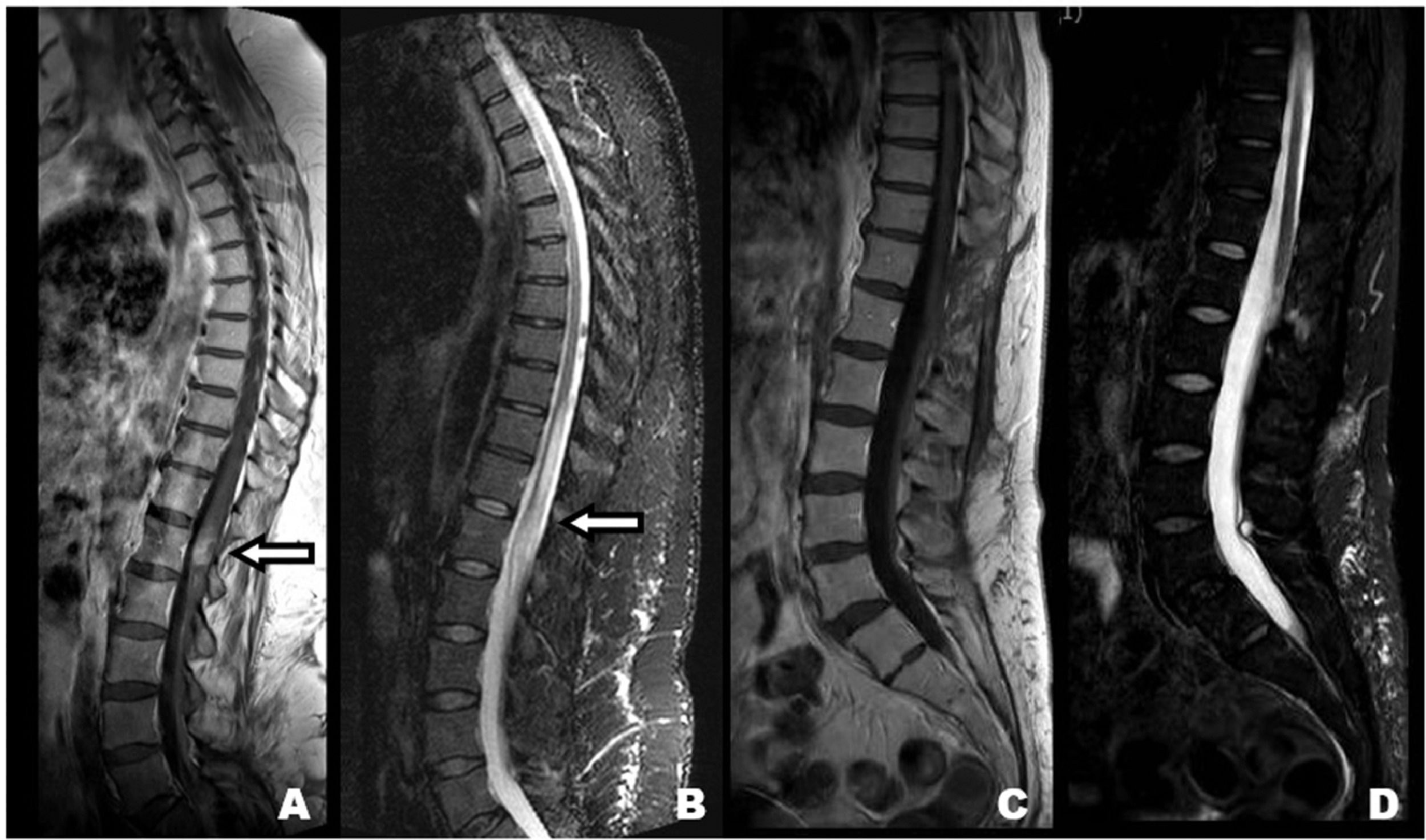
Spinal cord MRI revealed an expansive intramedular lesion concerning the conus medullaris (Figure 1; A-B). It exhibited patched hyperintense areas in both STIR and T2 sequences. Contrast enhancement was avid but focused in the conus medullaris. Neurosurgery Department was consulted to obtain tissue samples, that were analyzed by an expert neuropathologist reporting the presence of atypical B cells inside vessels (Figure 2).
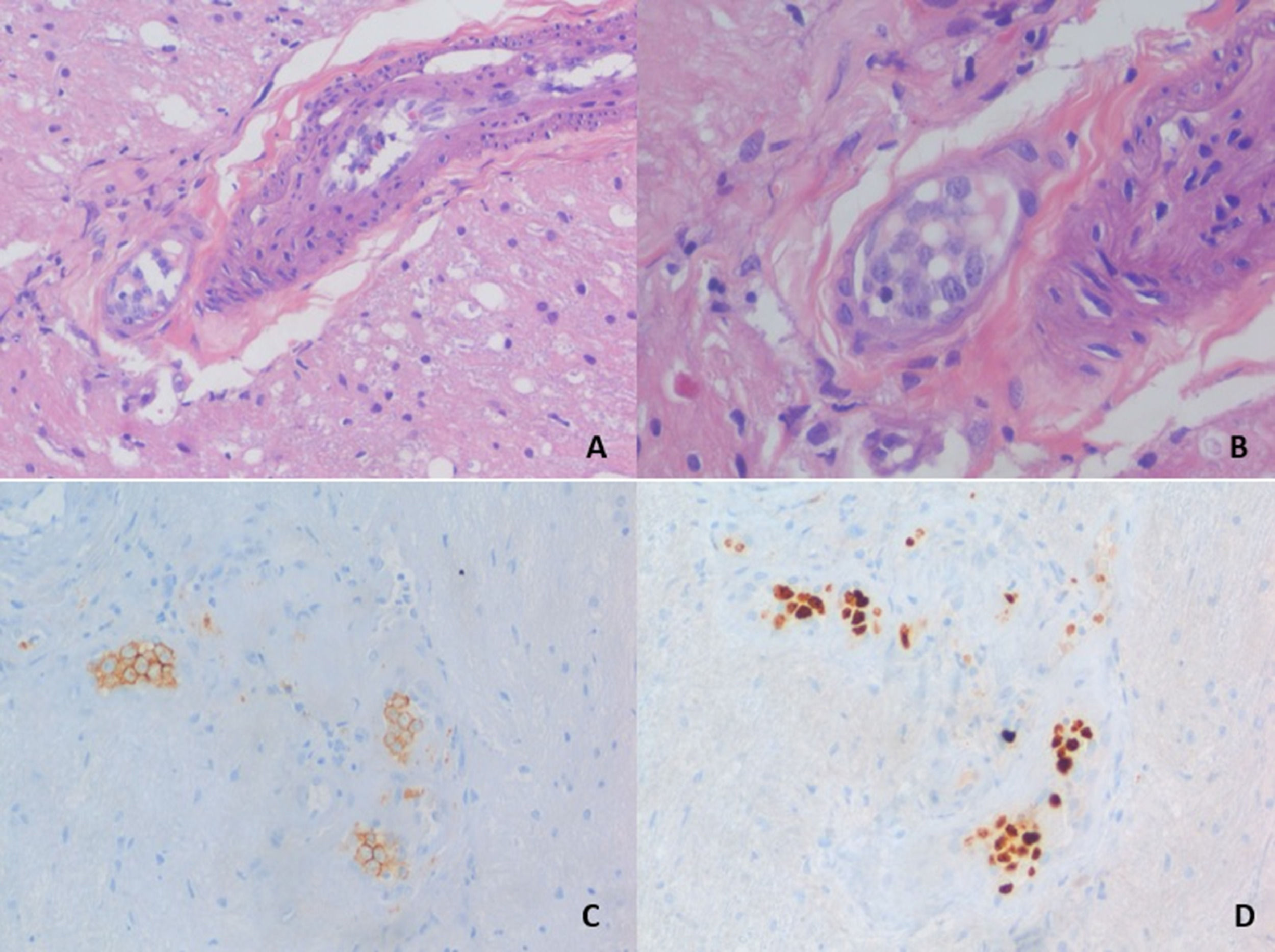
Hematoxylin-eosin staining of a biopsy sampling demonstraiting a blood vessel lumen filled with large cells of round and oval-shaped nuclei, prominent nucleoli and scant to moderate cytoplasm (A, B). These cells express typical B-cell markers as CD-20 (C) and also proliferation markers as Ki-67 (D).
The patient was referred to Hemathology Department, with the definitive diagnosis of intravascular lymphomatosis (B-cell lymphoma) affecting CNS with minimal circulating cells.
She started chemotherapy with Carmustine, Methotrexate and Cytarabine plus monoclonal antibody rituximab.3 Nine months later, she received autologous stem-cell transplantation.
In the last MRI to date, the conus medullaris showed a normal morphology and signal intensity. There was no enhancement after contrast injection (Figure 1; C-D). Repeated PET-scans showed no evidence of distant-disease, neither pre nor post-treatment. In terms of functional outcome, the patient has asymmetrical paraparesis, impending her from standing and walking unassisted, analgesia and anaesthesia with an L3 sensory level. Propioceptive sensibility is abolished bilaterally. Neurogenic bladder and bowel dysfunctions are settled.