Hemorrhage is a frequent medical emergency in the hospital environment. Hemorrhagic shock is a form of hypovolemic shock in which severe blood loss leads to inadequate oxygen supply at the cellular level. A significant loss of intravascular volume can sequentially lead to hemodynamic instability, decreased tissue perfusion, cellular hypoxia, organ damage and death.1,2 If the bleeding continues without control, death occurs quickly.3
Hemorrhagic shock is one of the main reversible causes of death in the world. An estimated 1.9 million deaths per year worldwide are associated with hemorrhage/hemorrhagic shock.2 The causes of hemorrhage resulting in shock range widely and include trauma, major surgeries such as, for example, obstetric surgery, transplantation and rupture of an aneurysm.3
Between 2013 and 2015, the average number of deaths related to failure to manage bleeding represented 32 % of all catastrophic events at Hospital Israelita Albert Einstein (Sao Paulo, Brazil). These events were due to failures in recognition and early treatment, as well as the lack of logistics between the hospital's support areas, which resulted in the delay of patient care.4 In view of this scenario, the institution developed a protocol called Code H (hemorrhagic code), which consists of recognizing sudden changes in the vital signs of adult patients that are associated with acute bleeding or hemodynamic instability and early referral for its resolution.
In this sense, the present work seeks to verify whether patients at risk of bleeding after the implementation of Code H had better outcomes and lower costs when compared with patients of the same severity before the implementation of the Code H protocol. In the period from 01/2001 to 12/2014, before the implementation of Code H, 19,824 hospitalizations occurred and 285 patients were included; from 03/2016 to 12/2020, there were 285 occurrences of the activation of Code H.
In the pre-Code H period, the inclusion parameters were: panic results in laboratory tests (consisting in critical results so that the physicians needed to be informed to take action), use of four or more units of red blood cell concentrate and consumption of Beriplex and Haemocomplettan (prothrombin complex and recombinant fibrinogen, respectively, used in the treatment of hemorrhages). In the post-Code H period, all patients for whom Code H was actioned were included.
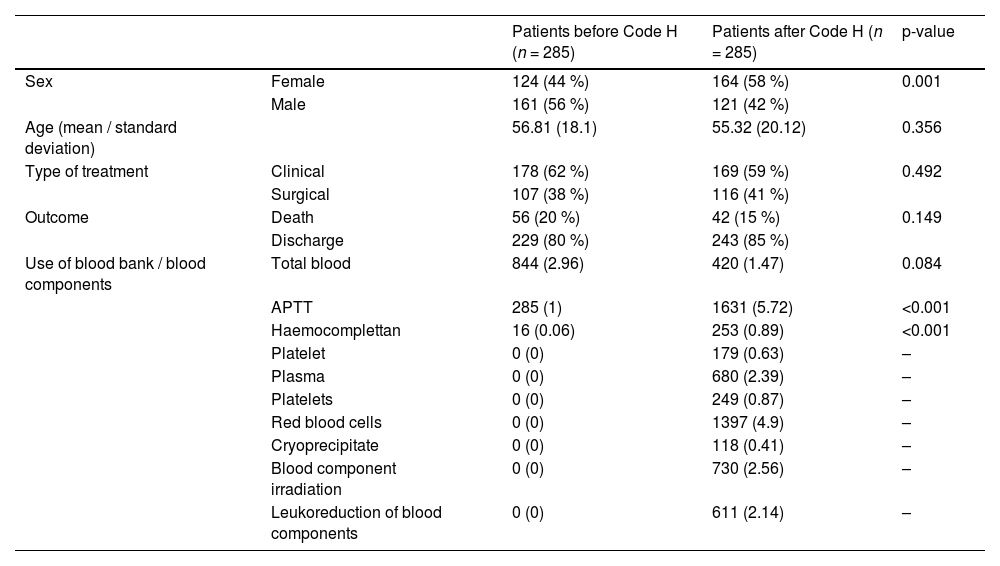
The items consumed by patients of both groups with similar hospitalization profiles were analyzed after pairing using the propensity score shown in Table 1.
Profile of patients analyzed after pairing using propensity scores.
APTT: Activated partial thromboplastin time.
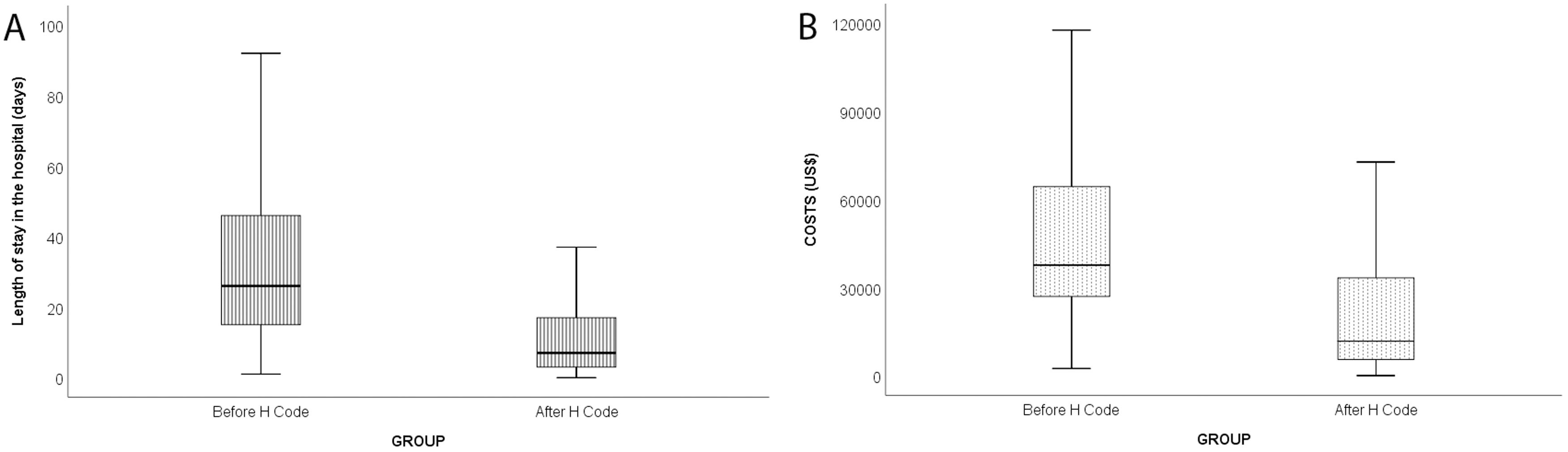
The length of hospital stay reduced significantly after the implantation of the Code H protocol (from 41 days to 16 days; p-value <0.0001), which means an approximate reduction of 50 % in the mean hospital costs (p-value < 0.0001) of each patient (Figure 1).
The estimated savings on comparing the two groups were around BRL 139,437.46 (about US$27,0751) when analyzing the average costs and BRL 123,432.46 (about US$23,967) when analyzing the median cost, generating a total savings for the 285 cases analyzed of BRL 39,739.675.16 (about US$7716,442). The reduction in the average length of stay of patients was about 25.36 days, generating savings for the 285 cases of 7227 hospital days, providing about four hospital beds per year.
The organization of the protocol in the PBM (Patient Blood Management) model was fundamental for the formation of a multi-professional and multidisciplinary team, with processes and flows centered on patient care and safety through multiple coordinated interventions.
As recommended by the Institute for Healthcare Improvement (IHI) in 2004, the Rapid Response Team (RRT) model, a group of professionals with expertise in critical and/or intensive care (anesthesia, clinical laboratory, imaging, blood bank, operating room, intensive care unit, emergency room, interventional therapy, and pharmacy) was implemented. Extensive training was implemented for professionals to quickly and effectively diagnose patients with hemorrhagic shock, as well as to define early treatment.5
Diagnostic tools were used in the precision medicine model to treat the lethal triad (acidosis, hypothermia, and coagulopathy). In the context of PBM, it is important that point-of-care testing (POCT), such as thromboelastometry and platelet function tests are used for rapid and accurate diagnosis of coagulopathies.
Following the PBM model, patients were treated with goal-guided therapies, rationalization in the use of blood components (packed red blood cells, platelets, fresh frozen plasma and cryoprecipitate), blood derivatives (prothrombin complex and recombinant fibrinogen), hemostatic agents (anti-fibrinolytics) and local hemostatics.
The Code H protocol in the PBM model showed expressive results regarding a reduction in the failure of the management of patients with severe hemorrhages and consequent reduction in deaths and improvement in the prognosis of these patients. Positive results were demonstrated with respect to cost effectiveness and improvement of clinical practice. There was a true transformation of the institutional culture regarding patient safety with an impact on medical professionals and multi-professional teams.