Consensus of the Brazilian association of hematology, hemotherapy and cellular therapy on patient blood management
More infoPatient Blood Management (PBM) is a holistic approach to managing blood as a resource of each patient; it is a multimodal strategy that is implemented using a set of techniques that can be applied in individual cases. In fact, the overall result of the implementation of PBM cannot be fully appreciated or explained by simply summing up the effects of the individual strategies and techniques used, since they can only produce the expected ideal result if combined. Implementing a PBM program in healthcare offers several benefits including improved patient safety, better outcomes, cost savings, conservation of resources, evidence-based practice, transfusion alternatives, improved quality of care, compliance with accreditation standards, patient-centered care, and professional education and training.
PBM is not a simple protocol, it is not just a change of a process in isolation, it is not reduced to the individual habits of a professional, it does not only focus on reducing expenses or saving resources and it is not the search for specific clinical results alone. Implementing PBM aims to coordinate all these aspects and others, which is why it is a change to a patient-centered care philosophy.
The biggest difficulty in introducing a PBM program is the lack of a widely accepted, reproducible practice for implementing and monitoring it.1 However, there are suggestions and successful experiences shared by different groups. As this is a multidisciplinary process, the positive engagement of the different areas involved under the guidance of the institutional management is essential.
It is important to highlight that the implementation of PBM can face several difficulties.2 Doctors and other professionals may resist the implementation of a new institutional guideline because they do not understand its real clinical usefulness and consider it just another bureaucratic measure. Therefore, attitudes that promote team commitment are fundamental, such as high-tech actions, agility in procedures and sharing the clinical and financial results gained with the PBM program.
In 2018, a conference held in Frankfurt systematically reviewed the literature for recommendations related to PBM. Ten clinical recommendations and 12 general recommendations were generated, including three for the management of preoperative anemia, six for transfusion thresholds and three for the implementation of the PBM program. These recommendations address topics such as: a) adverse effects and relevant clinical effects; b) program compliance, flexibility and flexibility; and c) cost-effectiveness.
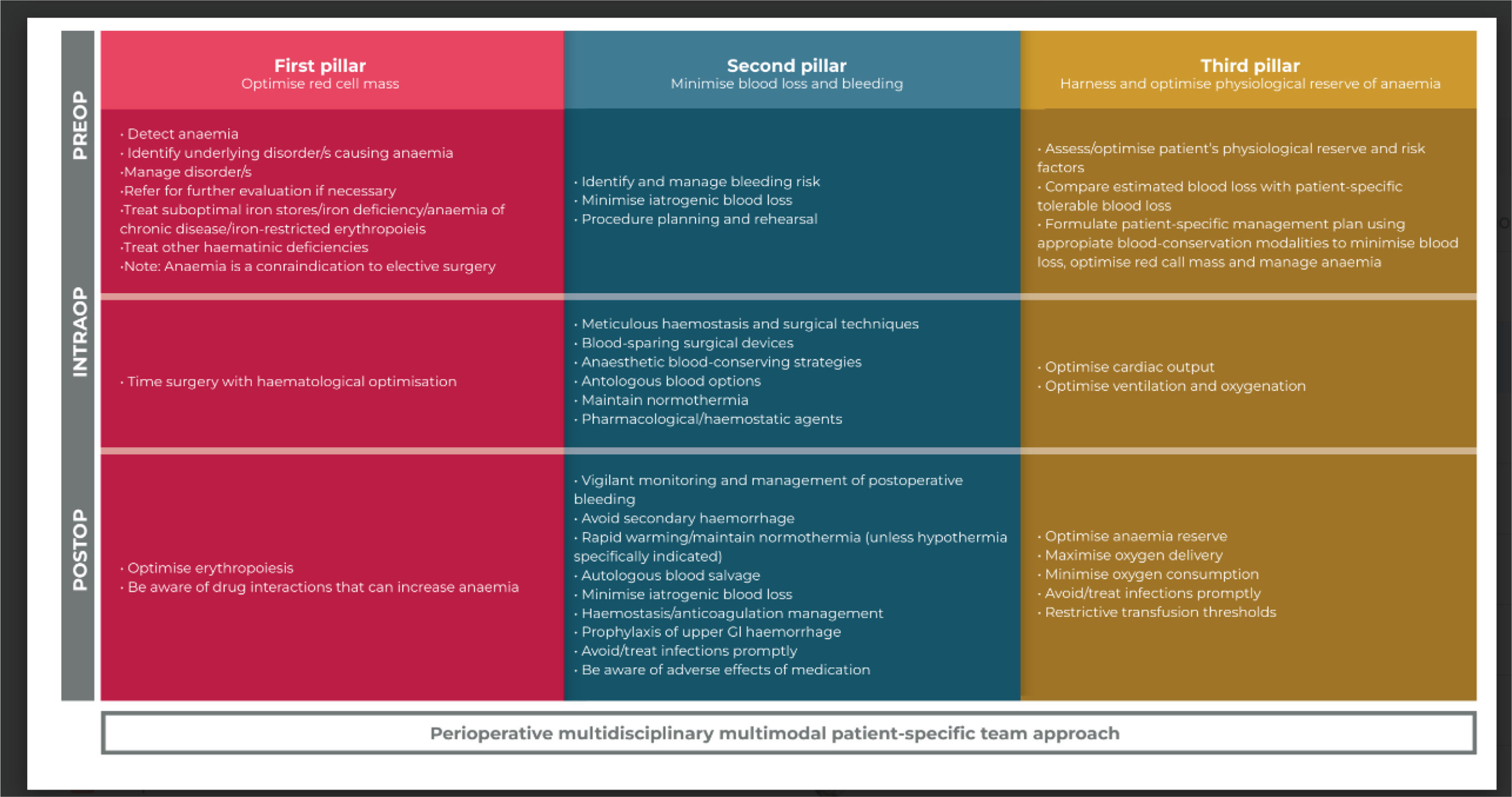
The pillars of patient blood management (PBM)The implementation of the PBM program must accomplish the three pillars of the practice (Figure 1):4
- 1)
Screening, diagnosis and adequate treatment of anemia; 2) minimization of surgical, procedural and iatrogenic blood loss and the management of bleeding due to coagulopathies throughout treatment; and 3) increasing tolerance of the patient's anemia.
- 1.
Anemia Management: To detect anemia, identify its cause, use supportive agents and reduce oxygen consumption.
- 2.
Multidisciplinary strategies to conserve the patient's own blood, including optimization of hemostasis and/or coagulopathies: reduce blood loss, collect tests rationally (microtubes), use surgical techniques that minimize blood loss, consider scheduled autotransfusions, employ intraoperative cell recovery and apply normovolemic hemodilution. Assess hemostasis, treat coagulopathies, reverse anticoagulation, use antifibrinolytics, consider the administration of desmopressin, lower the criteria for platelet transfusion and transfuse specific components, when necessary.
- 3.
Anemia Tolerance: Harness and optimize the patient's anemia physiologic reserve by formulating a patient-specific management plan, using appropriate blood conservation modalities to minimize blood losses, optimize red blood cell mass and control anemia. Set restrictive transfusion limits and optimize oxygen supply/consumption. Reduce diagnostic phlebotomies.5
- 1.
The three pillars of PBM and its strategic matrix (three treatment phases).
Adapted from: Thomson, J & Hofmann, Axel & Barrett, Claire & Beeton, A & Bellairs, G & Boretti, L & Coetzee, Marius & Farmer, Shannon & Gibbs, Matthew & Gombotz, H & Hilton, Caroline & Kassianides, C & Louw, Vernon & Lundgren, C & Mahlangu, Johnny & Noel, Colin & Rambiritch, V & Schneider, Frank & Verburgh, Estelle & Patie, A. (2019). Patient blood management: A solution for South Africa. South African Medical Journal. 109. 471. 10.7196/SAMJ.2019.v109i7.13859.5
PBM, a patient-centered care conduct, places the patient as the central figure of treatment, sharing information and decisions, obtaining consent and basing therapeutic decisions on patient-specific data (age, comorbidities, diagnosis, stage of the disease, hemodynamic reserve, oxygenation, among others). Thus, the decision to perform a transfusion is based on the clinical data of the patient taking into account their specific situation rather than pre-established laboratory values.
Spain developed a PBM implementation method that was gradually incorporated into several hospitals and is currently being used in 59 institutions. This program, called Maturity Assessment PBM (MAPBM), aims to establish objective measures, obtain a benchmark, facilitate access and disseminate the results of PBM programs.1 The European Union itself published practical guides on implementing PBM both in hospitals6 and at the national level.7
In Brazil, Benites et al. reported a positive experience implementing a PBM program in a university hospital.8 According to the authors, “The project was promptly approved by the hospital Board due to the relevance of the proposal, which required few financial resources, as the project is mainly based on the reorganization of workflows”.
The PBM program can cover more than 100 different procedures, apportioned to the three pillars. However, it is recommended that PBM proposals and measures should be implemented in the form of ‘packages’, aiming at greater effectiveness.9 These packages of measures must be considered as a basis and adapted to the conditions of each institution taking into account its complexity, staff and costs involved in the program. Therefore, the healthcare institution must select priority initiatives and define the type of PBM program to be implemented. It can be a simpler approach for internal institutional use or a more robust program, aiming at audits and accreditation by specialized groups, such as the Joint Commission and the Association for the Advancement of Blood & Biotherapies (AABB).4,10
Suggestions for packages of measures to be implemented- a.
The creation of a PBM project coordination group, responsible for implementing education and training activities in different areas of the health sectors.9 This group must be multidisciplinary and include professionals such as a clinical team leader, executive team leader, anesthesiologist, surgeon, critical care doctor, nurse, gastroenterologist, hematologist, cardiologist, obstetrician-gynecologist, financial representative, information technology technician and patient representative.
- b.
Establishing a method to objectively measure PBM in order to collect data and evaluate its effectiveness. This includes indicators such as the number of consultations, preoperative therapeutic approaches, number of transfusions, length of hospital stay, mortality rate, transfusion reactions, costs, among others.2,3
- c.
Implementation of an education program for doctors and nurses in priority areas, such as the operating room, intensive care unit, emergency room and laboratories. Furthermore, it is important to include outpatient clinics of different specialties, training courses for nurses, nursing and medical schools, medical and nursing residencies, specialization courses and programs for lay people/patients. These courses can be offered in person and/or online.
- d.
Development of general PBM protocols and specific protocols for areas such as cardiology, transplants, obstetrics, vascular surgery, among others.11,12 This includes pre-surgical outpatient PBM, transfusion algorithms, perioperative/inpatient protocols (covering the period before and after surgery), checklists for specific situations and massive transfusion protocols in cases such as postpartum, post-trauma, transplants and heart surgery.
- e.
Incorporation of electronic support that assists in decision-making regarding transfusion practice, especially in surgical and clinical specialties.13-15
- a.
Recommendation
PBM implementation is challenging due to the level of complexity and the need to manage an unusually large number of diverse stakeholder groups. Therefore, it is recommended that a PBM implementation coordination group be created, with support from hospital management, doctors, the hemotherapy department and multidisciplinary teams and with patient support.
The implementation of a PBM program is extremely important to improve healthcare. In addition to promoting significant clinical benefits, its implementation also provides economic advantages. By adopting PBM, hospital resources can be directed in a more cost-effective way, benefiting both patients and healthcare institutions. Therefore, it is imperative that healthcare managers and professionals seriously consider implementing PBM programs as a crucial strategy to improve the quality of care and to optimize available resources. A series of articles will be published covering in greater depth the pillars of PBM that contribute to this process.
Supporting internet references1 - PBM – Patient Blood Management: II Série de Webinar de Hemoterapia – link: https://youtu.be/PByJcH9gFzo
2 - HEMO PLAY Podcast #Ep48 - Conheça o projeto PBM da ABHH – link: https://youtu.be/TyegH31X7cI
3 - WEBINAR COLABORATIVO SOBRE PATIENT BLOOD MANAGEMENT – link: https://youtu.be/V1-iIHN_KZo