Consensus of the Brazilian association of hematology, hemotherapy and cellular therapy on patient blood management
More infoThe preoperative clinical and laboratory evaluations of the patient is an essential step to ensure the safety and success of any surgical procedure. This assessment aims to identify any underlying medical conditions and risk factors and determine suitability for surgery. With this step, the medical team can adapt the care plan to meet each patient's specific needs, increasing the chances of a successful procedure. Good clinical assessment and comprehensive laboratory testing, when integrated into a Patient Blood Management approach, are invaluable in promoting safety of care, reducing transfusion risks, improving surgical outcomes, and optimizing resource utilization. This approach not only elevates the quality of care, but is also aligned with evidence-based practice and patient-centered principles, making it an essential component of the perioperative process.
Preoperative assessment is crucial for the early diagnosis and treatment of conditions that may adversely affect the patient's evolution, both intraoperatively and postoperatively. Thus, preoperatively, a systematic approach, including clinical and laboratory assessments, should minimize or even eliminate identified risk factors and contribute to a shorter hospital stay, a lower risk of complications and better clinical outcomes.1 Therefore, it is recommended that every service has a protocol with a preoperative assessment algorithm. The existence of a protocol ensures that higher-risk patients undergo the necessary additional evaluation and unnecessary assessments are avoided for patients at low risk for complications.2 In this article, recommendations are proposed based on current literature, however, each center must adapt these recommendations to their own reality.
Patient Blood Management (PBM) is a patient-centered, systematic and evidence-based approach that aims to improve clinical outcomes through the management and preservation of the patient's own blood.1,3,4 The preoperative period is the first opportunity to apply the three pillars of PBM with the diagnosis and treatment of anemia and iron deficiency, as well as the optimization of coagulation before surgery; these are essential points for success of this approach. Hence, a preoperative evaluation should begin as soon as surgery is indicated, allowing an early diagnosis of anemia and coagulation disorders, thereby ensuring an adequate time interval of at least four weeks of treatment before the date of the surgery. If anemia is diagnosed, it is necessary to continue an investigation of coagulopathies and elective non-oncological surgeries should, whenever possible, be postponed until the anemia and coagulopathies are resolved.
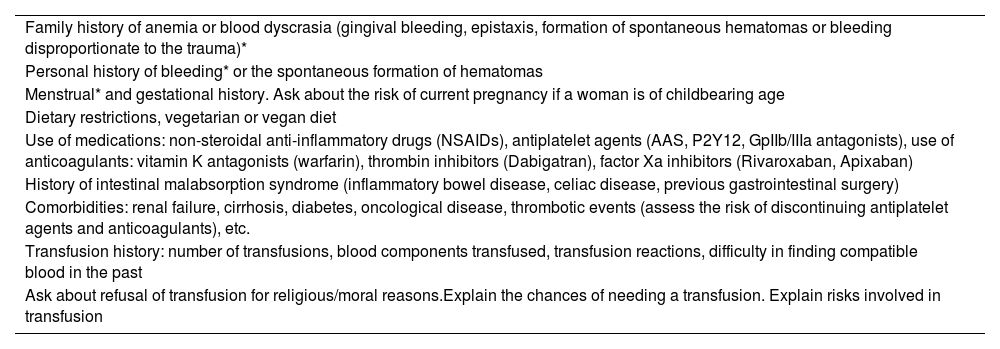
Preoperative assessment should include an interview and physical examination aimed at identifying patients at greatest risk of bleeding. Advanced age, female sex, low body weight, chronic kidney disease and liver disease are characteristics associated with a higher risk of perioperative transfusion. The patient should be asked about signs and symptoms of anemia, bleeding manifestations, risk factors for anemia and iron deficiency, known family history of anemia or hereditary coagulopathies, as well as the use of allopathic and homeopathic medicines that increase the risk of bleeding, in particular antiplatelet agents and anticoagulants (Table 1).
Preoperative clinical interview.
| Family history of anemia or blood dyscrasia (gingival bleeding, epistaxis, formation of spontaneous hematomas or bleeding disproportionate to the trauma)* |
| Personal history of bleeding* or the spontaneous formation of hematomas |
| Menstrual* and gestational history. Ask about the risk of current pregnancy if a woman is of childbearing age |
| Dietary restrictions, vegetarian or vegan diet |
| Use of medications: non-steroidal anti-inflammatory drugs (NSAIDs), antiplatelet agents (AAS, P2Y12, GpIIb/IIIa antagonists), use of anticoagulants: vitamin K antagonists (warfarin), thrombin inhibitors (Dabigatran), factor Xa inhibitors (Rivaroxaban, Apixaban) |
| History of intestinal malabsorption syndrome (inflammatory bowel disease, celiac disease, previous gastrointestinal surgery) |
| Comorbidities: renal failure, cirrhosis, diabetes, oncological disease, thrombotic events (assess the risk of discontinuing antiplatelet agents and anticoagulants), etc. |
| Transfusion history: number of transfusions, blood components transfused, transfusion reactions, difficulty in finding compatible blood in the past |
| Ask about refusal of transfusion for religious/moral reasons.Explain the chances of needing a transfusion. Explain risks involved in transfusion |
If there is a history of atypical/increased bleeding, it is recommended to apply a validated tool to estimate the risk of coagulation disorders (Bleeding Assessment Tool).5
Anemia affects 30 to 40 % of patients preoperatively and is an independent risk factor for transfusion. It is also associated with higher perioperative mortality and morbidity, including kidney injury, cardiovascular events and a higher rate of hospital readmissions. Transfusion, in turn, is associated with higher morbidity and mortality, higher infection rates, hospital readmission and longer hospital stays. Even so, the inappropriate use of red blood cell transfusions in patients, for whom anemia was not recognized or adequately treated preoperatively, is common.6
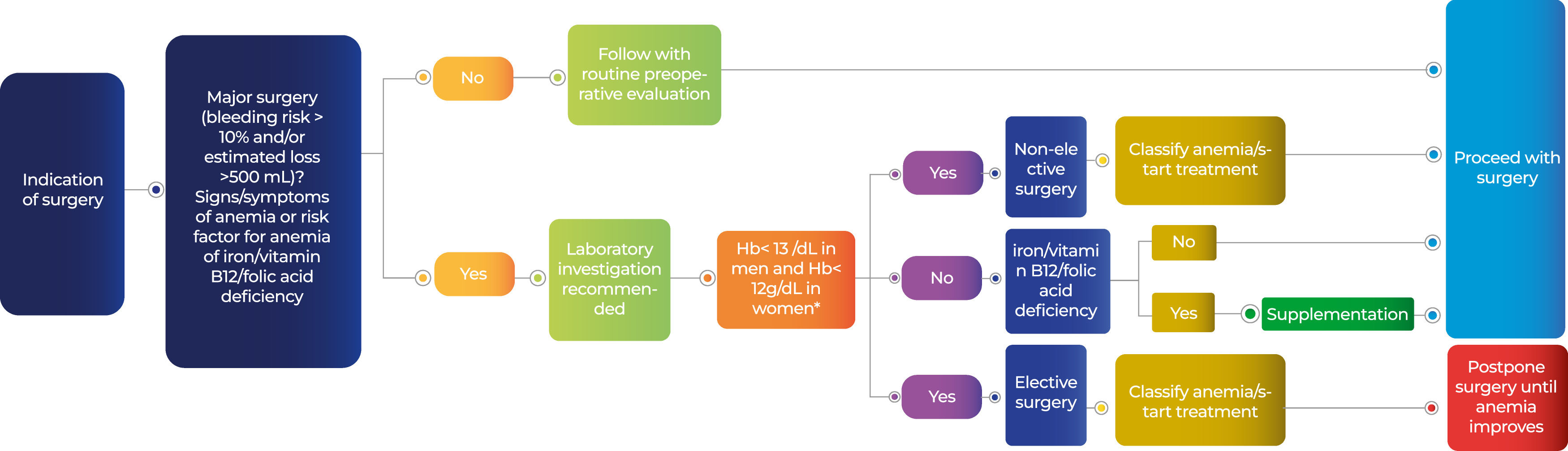
An investigation of anemia should be carried out for every patient undergoing surgery when the estimated blood loss is >500 mL or the risk of transfusion is >10 %. Patients with complaints suggestive of anemia or with risk factors for anemia or those with Sickle cell disease should also be investigated.7 Due to the high prevalence and negative clinical impact, it is recommended that the presence of iron deficiency be investigated in the entire at-risk population, even in the absence of anemia.7 Furthermore, it is suggested that vitamin B12 and folic acid deficiencies should be assessed, even in the absence of anemia. This is because, although less prevalent (10 %), they are two reversible risk factors and deficiency can negatively affect recovery due to anemia in the postoperative period.6 It is advisable that each institution has an algorithm for screening, investigating and treating anemia.8 Other tests, such as reticulocyte count, C-reactive protein, thyroid-stimulating hormone (TSH), among others, can be requested later, or even in parallel with the initial tests, in order to speed up the preoperative investigation.
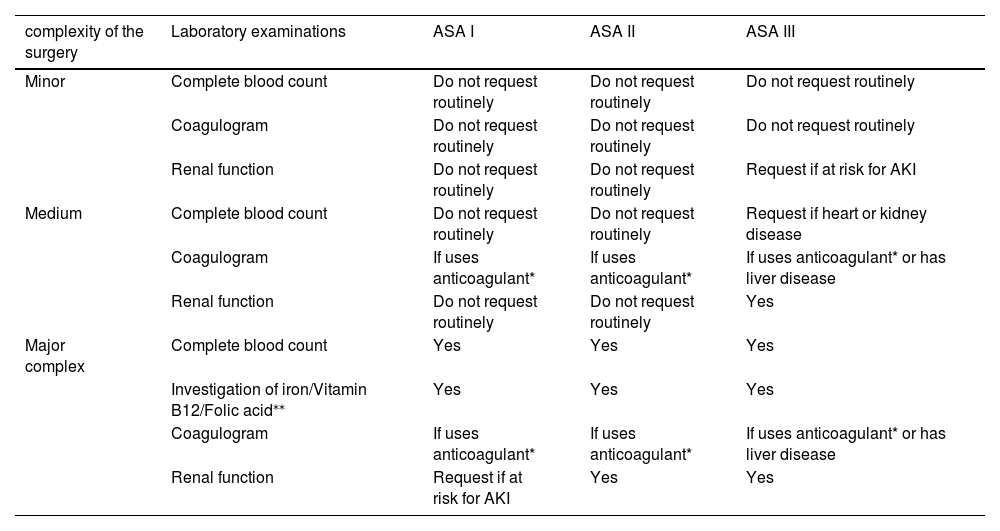
Table 2 summarizes the initial laboratory tests that should be requested according to the complexity of the surgery and the patient's individual risk. Exams should be performed at least four weeks before the scheduled surgery date to allow for adequate investigation and treatment. Figure 1 provides a suggestion for the initial approach to patients with anemia. Further details on the preoperative investigation and treatment of anemia are discussed in another article in this consensus on the Preoperative Management of Patient Anemia.
Laboratory evaluation according to the complexity of the surgery and patient risk.
| complexity of the surgery | Laboratory examinations | ASA I | ASA II | ASA III |
|---|---|---|---|---|
| Minor | Complete blood count | Do not request routinely | Do not request routinely | Do not request routinely |
| Coagulogram | Do not request routinely | Do not request routinely | Do not request routinely | |
| Renal function | Do not request routinely | Do not request routinely | Request if at risk for AKI | |
| Medium | Complete blood count | Do not request routinely | Do not request routinely | Request if heart or kidney disease |
| Coagulogram | If uses anticoagulant* | If uses anticoagulant* | If uses anticoagulant* or has liver disease | |
| Renal function | Do not request routinely | Do not request routinely | Yes | |
| Major complex | Complete blood count | Yes | Yes | Yes |
| Investigation of iron/Vitamin B12/Folic acid⁎⁎ | Yes | Yes | Yes | |
| Coagulogram | If uses anticoagulant* | If uses anticoagulant* | If uses anticoagulant* or has liver disease | |
| Renal function | Request if at risk for AKI | Yes | Yes |
Source: ASA (American Society of Anesthesiologists) – Classification: ASA I - (a normal healthy patient); ASA II - (a patient with mild systemic disease); ASA III - (a patient with severe systemic disease); ASA IV - (a patient with severe systemic disease that is a constant threat to life); AKI: acute kidney injury.
Request exam and plan depending on the anticoagulant. Performing prothrombin time (TP) and activated partial thromboplastin time (aTPP) tests are not recommended routinely, as they do not estimate the risk of bleeding in the absence of clinical history of hemorrhagic manifestations.
For all patients that will be submitted to major surgery and for any patient with signs/symptoms of anemia or with risk factors for anemia/iron or vitamin deficiency.
Adapted from Excellence and People (2008).2
Initial evaluation of anemia in the preoperative period.
*Some specialists suggest the same cutoff point of 13 g/dL for women, as the volume of blood loss in the surgery is the same for both men and women, however it represents a higher percentage for women who generally have a lower blood volume.
Adapted from Gómez-Ramirez et al. (2019).6
The transfusion of blood components must be cautiously indicated when, after investigation and appropriate treatment, there is no satisfactory recovery of hemoglobin level and there are concomitant signs of impaired tissue oxygenation and/or hemodynamic instability. Red blood cell transfusions should not be used preoperatively to correct mild to moderate anemia. Furthermore, when transfusion is indicated, a restrictive transfusion strategy should be chosen as it is not inferior to the liberal strategy and also reduces the risks associated with transfusions.8 In iron deficiency anemia, the treatment of choice is iron, with red blood cell transfusions restricted to very severe cases. In these cases, the volume to be transfused must be sufficient to improve the symptoms of tissue hypoxia and treatment should then continue with iron replacement.7
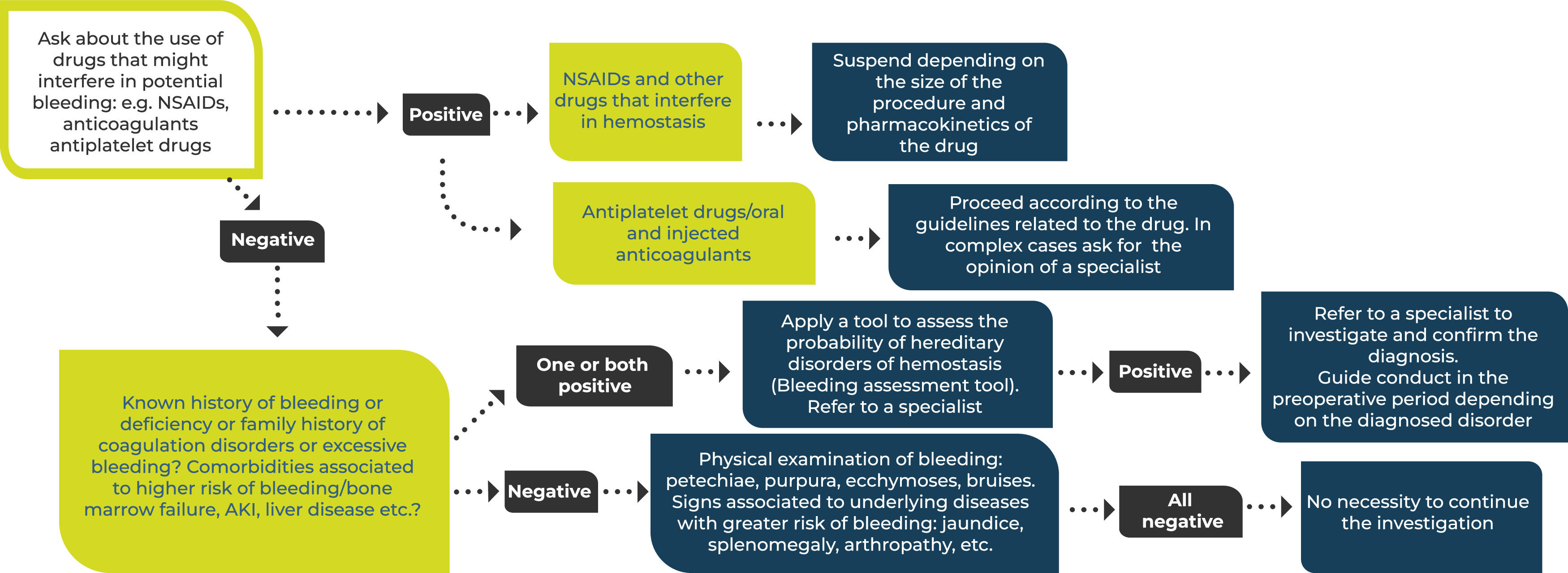
Hemorrhage is still the most common perioperative complication. Although local factors inherent to the surgical procedure are involved, many patient-related risk factors can be identified and managed preoperatively. If the initial interview is positive for a history of bleeding, the application of a validated tool to assess the risk of bleeding (Bleeding Assessment Tool) is recommended.5 Many still consider it standard to perform routine prothrombin time (PT) and partial activated thromboplastin time (aPTT) tests to assess the risk of bleeding in surgical patients. However, evidence does not support this strategy and current guidelines do not advocate the indiscriminate use of these tests for every patient, since they are not capable of predicting the risk of bleeding in patients without a suggestive history.9,10Figure 2 provides a suggestion for the initial approach to assess the risk of bleeding.
Initial clinical evaluation of hemostasis in the preoperative period.
NSAIDs: non-steroidal anti-inflammatory drugs; AKI: acute kidney injury. Adapted from the National Blood Authority (2015).11
For any surgical procedure where significant patient blood loss may be anticipated, such as major, complex surgeries with a known high risk of significant blood loss, discussions involving the surgical team, anesthetist, and hematologist/hemotherapist can identify opportunities to plan preoperative or intraoperative measures in order to reduce the chance of allogeneic transfusion. The possibility of benefitting from preoperative autologous blood donation, acute normovolemic hemodilution or intraoperative blood recovery should be discussed.12-14 Every service that performs major surgeries should have a written protocol describing the indications for each of these modalities, as well as the procedure itself.12
The benefit of autologous donation in terms of reducing the likelihood of allogeneic transfusion is relatively small and may actually increase the risk of postoperative anemia, especially if the donation is made close to the date of surgery without sufficient time for recovery of red blood cell mass and/or without adequate iron supplementation in parallel. However, autologous donation has special value when the patient refuses an allogeneic transfusion or if there is complex alloimmunization and difficulty in finding a compatible donor.12
Recommendations
- We recommend that good pre-operative clinical and laboratory assessments of the patient be carried out aiming at identifying cases of anemia and potential coagulation disorders in order to promote patient safety, reduce transfusion risks, improve surgical results and optimize the use of resources.
- Anemia investigation should be carried out for every patient undergoing surgery when the estimated blood loss is >500 mL or the risk of transfusion is >10 %. Patients with complaints suggestive of anemia or with risk factors for anemia and/or iron deficiency should also be investigated.
- If the initial interview is positive for a history of bleeding, the application of a validated tool to assess bleeding risk is recommended.
- Every service that performs major surgeries should have protocols for preoperative autologous blood donation, acute normovolemic hemodilution and intraoperative blood recovery as part of the preoperative evaluation of surgical patients.
Good clinical assessment and comprehensive laboratory testing, when integrated into a Patient Blood Management approach, are invaluable to promote safety, reduce transfusion risks, improve surgical outcomes, and optimize resource utilization. This approach not only enhances care but also aligns with evidence-based practice and patient-centered principles, making it an essential component of the preoperative process.