Bone marrow necrosis (BMN) is considered a rare condition that occurs mainly in hematological and sometime in non-hematological disorders. It was defined by the disruption of more than 50% of the bone marrow architecture with the necrosis of the stroma and myeloid tissue without cortical bone involvement.1 Bone marrow examination is considering the cornerstone in diagnosing and assessing hematological disorders as in marrow necrosis.2 BMN caused by high dose chemotherapy given for the management of some leukemia. The diagnosis of BMN usually confirmed during the post-mortem period, but it should be highly suspected in those cases with severe BM failure with febrile neutropenia.3
A granulocyte-colony stimulation factor (GCSF) is considered an essential part of the management of febrile neutropenia. GCSF helps to decrease the duration of admission following myeloablative chemotherapy protocol.4 Few cases of BMN have been reported, mainly in acute leukemia either during induction chemotherapy or during conditioning protocol for autologous or allogeneic stem cell transplantation.5–8
Here, we report a 19-year-old male with refractory Hodgkin's lymphoma with high-risk bulky stage IVB, treated by salvage chemotherapy for autologous stem cell transplantation that developed BMN following administration of G-CSF.
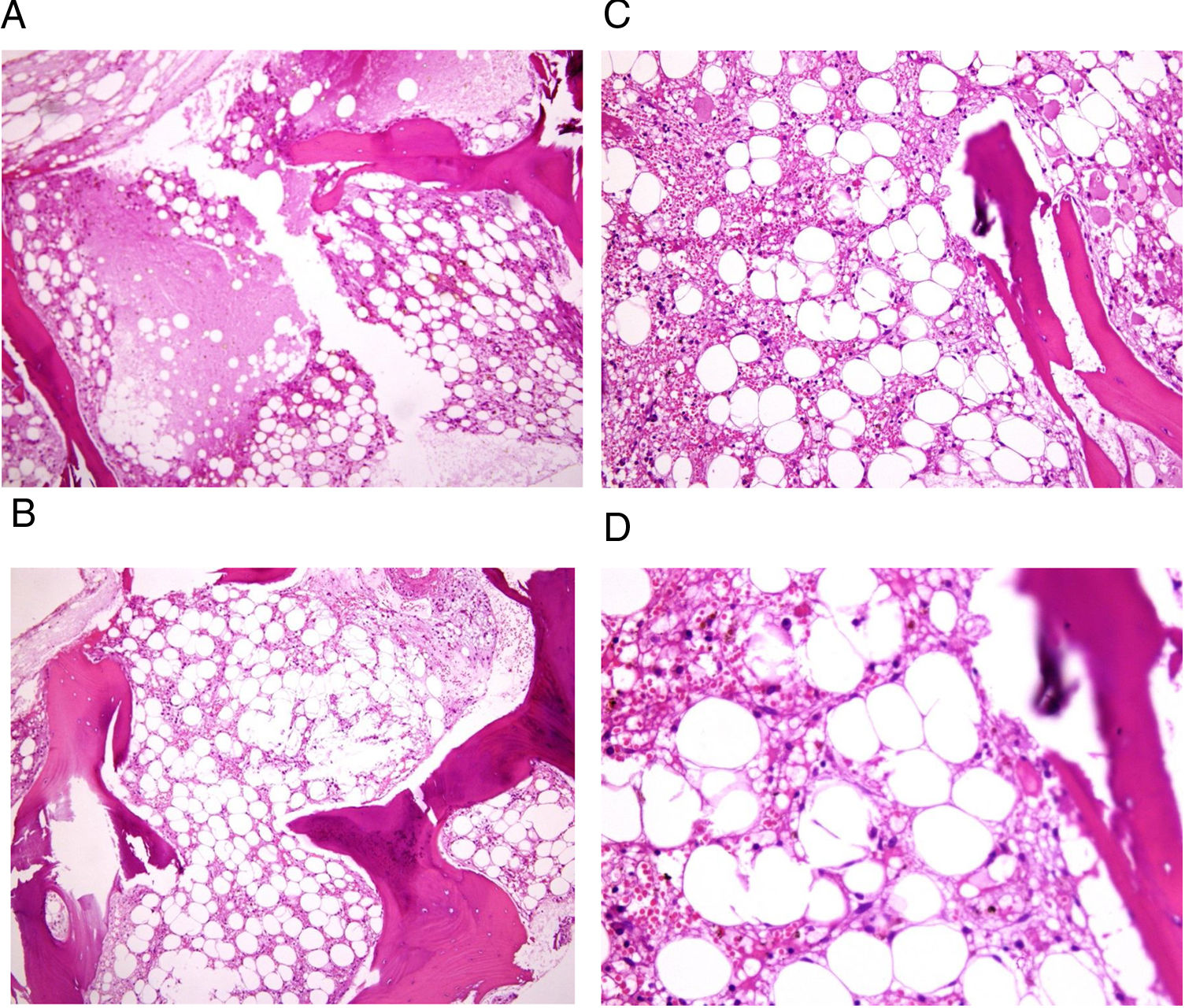
Case reportA 19-year-old man presented with neck swelling, fever, night sweat, and significant weight loss for 6-month duration. He was diagnosed as a stage IVB bulky mediastinal (>10cm) classical Hodgkin's Lymphoma-lymphocyte depleted (HL-LD) with many Reed-Sternberg cells with positive CD30 and CD15 and pleural effusion. He received six courses of ABVD with a positive FDG-PET scan after the last course. The patient was subjected to another biopsy for confirmation of diagnosis, which yielded the same classical HL-LD type. Then the hospital Multidisciplinary team decided to give him salvage followed by autologous stem marrow transplantation. He had been prepared for autologous stem cell transplantation after receiving salvage (BeGEF) chemotherapy protocol. The patient got partial remission after salvage chemotherapy. Stem cells were harvested after giving 10 days of granulocyte colony-stimulating factor (G-CSF+Plerixafor). The collection of stem cells had been completed, and patients discharged well. One week later, the patient returned to the hospital complaining of fever and headache. On examination, he had blurred vision, purpura, ecchymosis, bleeding from gum, and epistaxis. Full blood count showed thrombocytopenia, leucopenia, and anemia with vitreous hemorrhage on ophthalmoscope eye examination. The patient remained for 35 days in the intensive care unit, he had multiple blood cultures, and was received different modalities of antimicrobials but the patient did not respond, and the patient was kept on blood and platelets transfusion. Repeated blood cultures were negative, but CT scan of chest showed signs of pneumonia. On day 28, bone marrow aspiration and biopsy has been done for him which showed prominent BM necrosis, as in Figure 1A–D. Unfortunately, the patient died on day 35 after stem cell harvesting.
(A–D) Bone marrow biopsy of a patient with bone marrow necrosis showed disturbed marrow architecture, with diffuse bone marrow necrosis, cells revealing coagulative necrosis, with loss of normal staining, cells are embedded in an amorphous eosinophilic background. Stained by Hematoxylin & Eosin.
The conditioning protocols for autologous stem cell transplantation designed for refractory Hodgkin lymphoma currently including the administration of G-CSF to enhance the collection of stem cells. If could not get enough amount of stem cell, you can add CXCR4 antagonist (Plerixafor) on day 5 onward.9 The incidence of BMN varies. Some authors found a higher prevalence of BMN in a patient with Hodgkin lymphoma, reaching up to 20–25%7,8 while Janssens et al. reported BMN in only 2% of patients with Hodgkin lymphoma.10
To our knowledge, there is no case report of BMN after the collection of stem cells using G-CSF (Plerixafor) for the patient with refractory Hodgkin lymphoma. However, BMN was reported following the administration of G-CSF (Plerixafor) before conditioning for non-Hodgkin lymphoma.11 It is interesting to note that in this case, the time between administration of G-CSF (Plerixafor) and development of BMN was only 1 week, which agrees with that reported by Osuorji et al. and Katayama et al.4,6 One theory behind that may be due to bone marrow microvascular occlusion because of G-CSF (Plerixafor) induces the rapid proliferation of myeloid cell lines and consequent BMN.12 The involvement of bone marrow by Reed-Sternberg cells and intense stimulation by G-CSF (Plerixafor) has changed the microenvironment and microcirculation of the marrow. The latter effect might cause BMN later on. The Clinical features of patients who suffered from BMN usually include bone pain, fever, anemia, thrombocytopenia, leucocytosis, and leucoerythroblastic blood smear.10 The presentation with bone pain, high temperature, and pancytopenia confer fatal results and poor prognosis, as in our case, which is similar to the case report by Elgamal et al.8
ConclusionBMN related to G-CSF (Plerixafor) administration is still underestimated. Bone marrow involvement in Hodgkin lymphoma may be considered as a risk factor for the development of BMN, and the latter offers a poor prognosis.
Conflicts of interestThe authors declare no conflicts of interest.
Special thanks to Shorsh hospital and Hiwa hospital for performing a pathological report and managing the case, special thanks to the patient family who permitted us to publish his data.