Preeclampsia is one of the major health problems causing maternal morbidity and mortality, complicating 3–8% of pregnancies. It has been suggested that the alterations in the coagulation and fibrinolysis play a role in the pathogenesis of preeclampsia. The markers of platelet activation include platelet count, platelet distribution width, mean platelet volume and plateletcrit.
Study designIt was a case-controlled study which included a total of 60 patients (30 cases and 30 controls). Blood samples were collected and the platelet indices – platelet count, plateletcrit, mean platelet volume and platelet distribution width – were evaluated using the Sysmex XN1000 and compared between the two groups.
ResultsThe MPV and PDW also showed a significant difference (p>0.05) between the two groups, with a significant positive correlation with increasing blood pressure (MPV – r=+0.6126, p<0.05 and PDW – r=+0.6441, p<0.05). The PC and PCT had lower values in the preeclampsia patients, however the difference between the two groups was not statistically significant.
ConclusionThe MPV and PDW showed a significant difference between the two groups and increasing values with increasing BP. However, the PC and PCT in our study did not show a significant correlation with preeclampsia. Thus, the platelet indices, mainly the MPV and PDW, which are economical and easily available, can be reliable in the prediction and early diagnosis of preeclampsia, as well as a marker for the severity of preeclampsia.
Preeclampsia is one of the major health problems causing maternal morbidity and mortality, complicating 3–8% of pregnancies.1 It is a complex, multisystem disorder of unknown etiology. According to the International Society for the Study of Hypertension in Pregnancy (ISSHP), PE is defined as de novo hypertension, occurring after 20 weeks of pregnancy, together with proteinuria.2 It has also been suggested that the alterations in coagulation and fibrinolysis play a role in the pathogenesis of preeclampsia.3 The markers of platelet activation include platelet count (PC), platelet distribution width (PDW), mean platelet volume (MPV) and plateletcrit (PCT).4 These indices are cost-effective and easily available as they are derived from routine blood investigations.2 Platelet indices may be used as an early markers for the diagnosis of thromboembolic diseases.2 These parameters can be used for prediction of Pregnancy Induced Hypertension (PIH) before the derangement in prothrombin time (PT), activated partial thrombin time (ApTT) and thrombin time (TT) values areobserved.5 Thrombocytopenia is the most common hematological abnormality observed in preeclampsia and it may be due to consumption of platelets during abnormal activation of the coagulation system.2,3,6 A number of studies have shown that D-dimer, soluble vascular endothelial growth factor receptor and platelet distribution width may be used as preeclampsia, however due to varied effects on the coagulation-fibrinolytic system in preeclampsia in late pregnancy, no conclusive evidence can be drawn.7
Thus, in our study we aim to find a relationship between the platelet indices, namely platelet count, plateletcrit, mean platelet volume and platelet distribution width with preeclampsia, and try to assess whether these parameters could be used as markers for early diagnosis, as well as for the purpose of prognostication of the disease.
MethodsThe study was a prospective, case-controlled study and was conducted in the Department of Pathology and Department of Gynecology, ESIC Medical College and Hospital, Faridabad within a period of three months (July–September 2017). A total of 60 consenting patients were included in the study with 30 cases of preeclampsia (BP >140/90mmHg and proteinuria >300mg/day in patients of >20 weeks gestation) and 30 age-matched healthy pregnant females with a gestation period >20 weeks as controls.
Patients with pre-existing hypertension, renal disorders, diabetes mellitus and hematological disorders were excluded from the study.
Under aseptic conditions, the sample (2ml) was collected in ethylene diamine tetra acetic acid (EDTA) vials. The samples were analyzed on the Automated Counter Sysmex XN1000 on which were observed the platelet indices, which include platelet count (PC), mean platelet volume (MPV), platelet distribution width (PDW) and plateletcrit (PCT). A comparison between the above-mentioned platelet indices was made between cases and controls.
Statistical analysisThe median and interquartile ranges of all the parameters were calculated for cases and controls. A comparison in platelet indices between the cases and controls was made using the Mann–Whitney test and the p<0.05 was considered to be significant. A correlation between the MPV and BP, as well as the PDW and BP, was also made by calculating the Spearman's rank correlation coefficient (r) and the p value was calculated using (r). The value of p<0.05 was considered significant.
Ethical clearance was obtained from the institutional ethical committee.
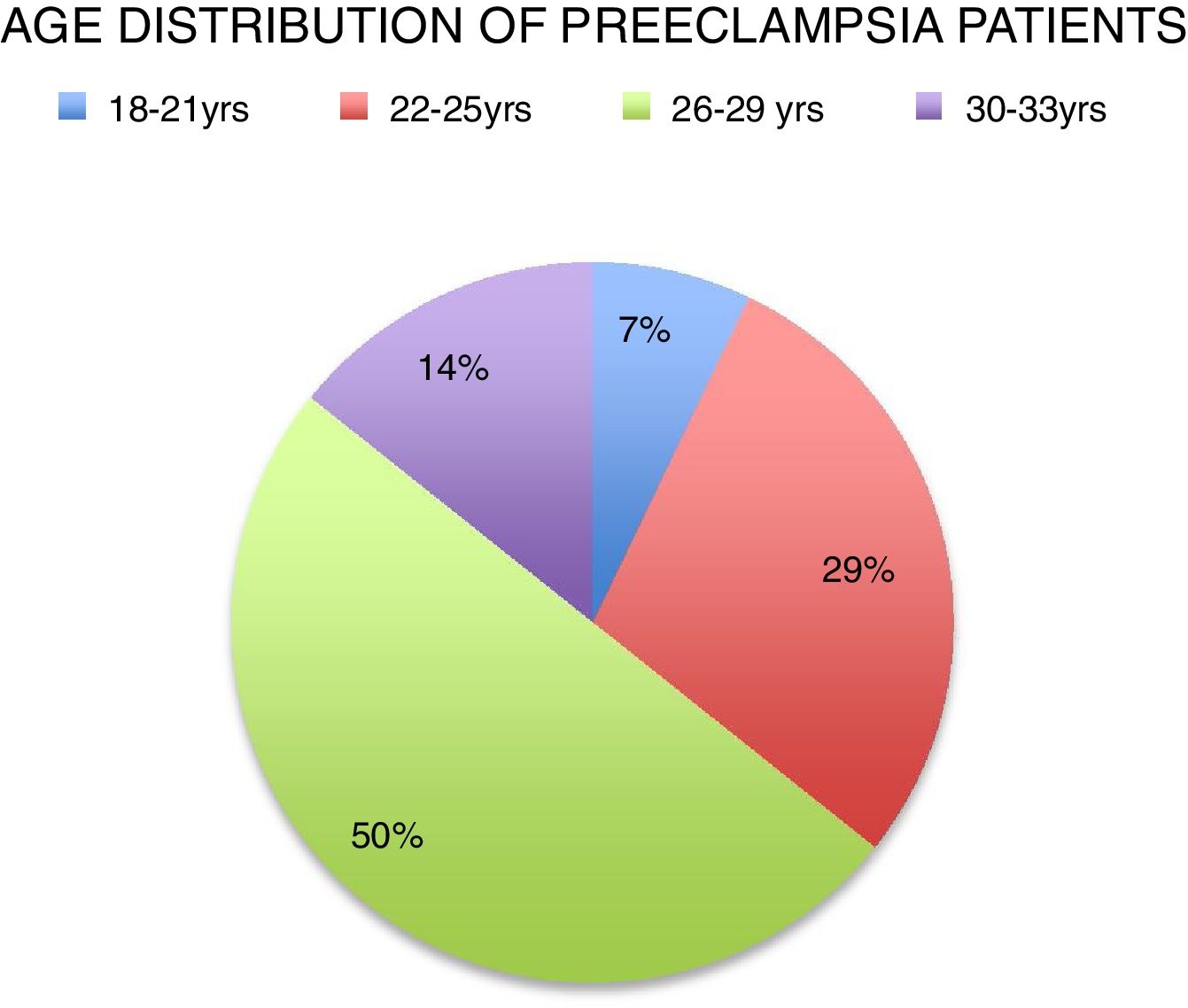
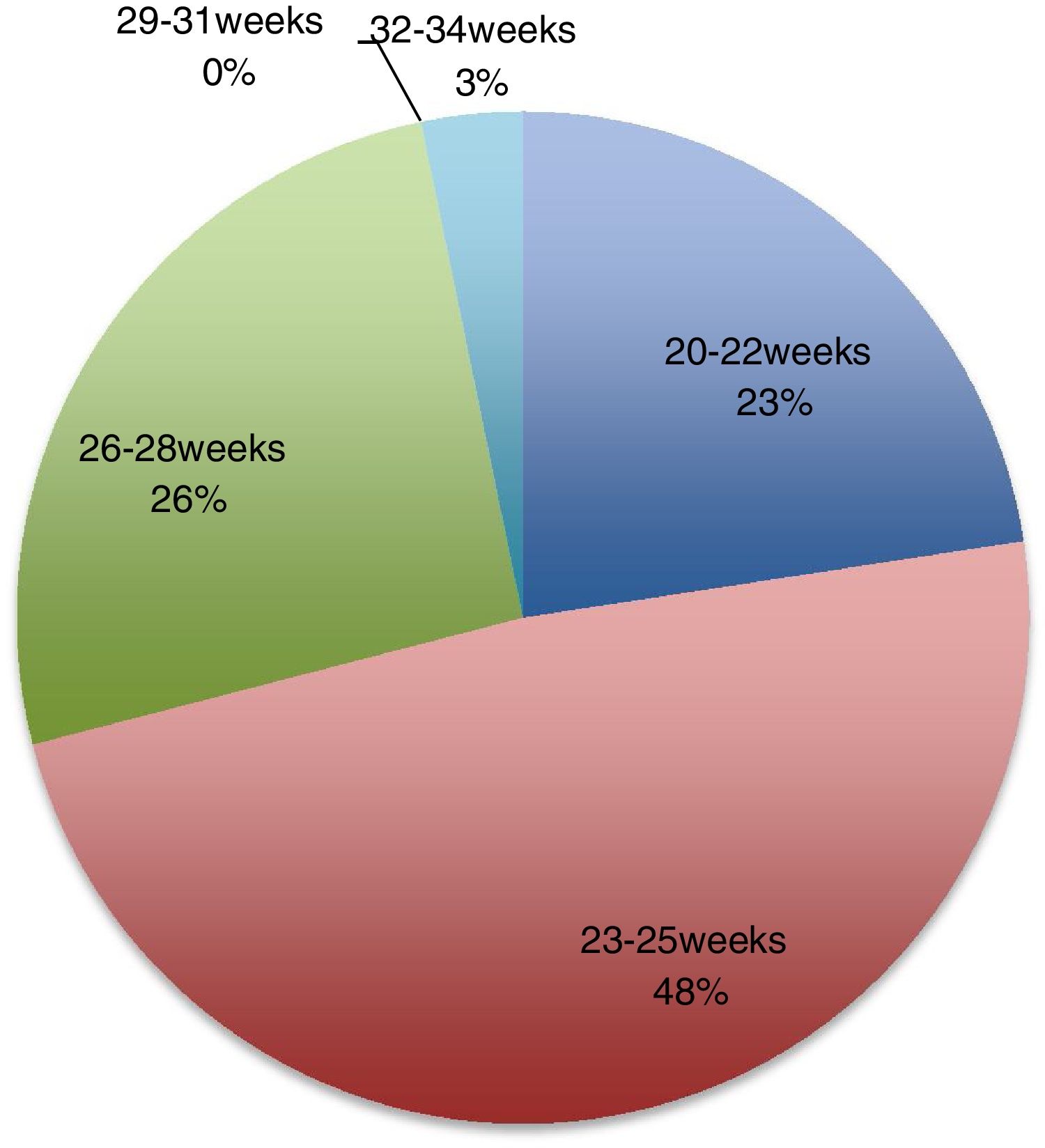
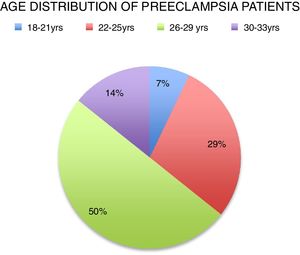
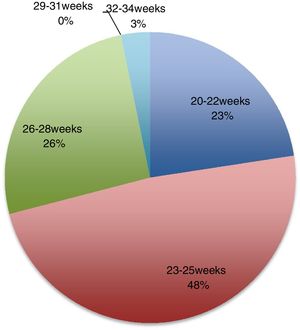
ResultsA total of 60 patients, 30 cases having preeclampsia with BP >140/90mmHg and proteinuria and 30 healthy pregnant females with gestation >20 weeks were included in the present study. The females in both the groups were in the age group (20–35 yrs). The mean age of the patients with preeclampsia was 26 years, with most in the age group 26–29 yrs (50%) (Figure 1). The mean period of gestation at the time of the collection of samples in the preeclampsia group was 24 weeks, with the highest duration being 32 weeks and 48% of the patients belonging to the group 23–25 weeks (Figure 2). The mean age and period of gestation of the controls was 24 yrs and 30 weeks, respectively at the time of the sample collection.
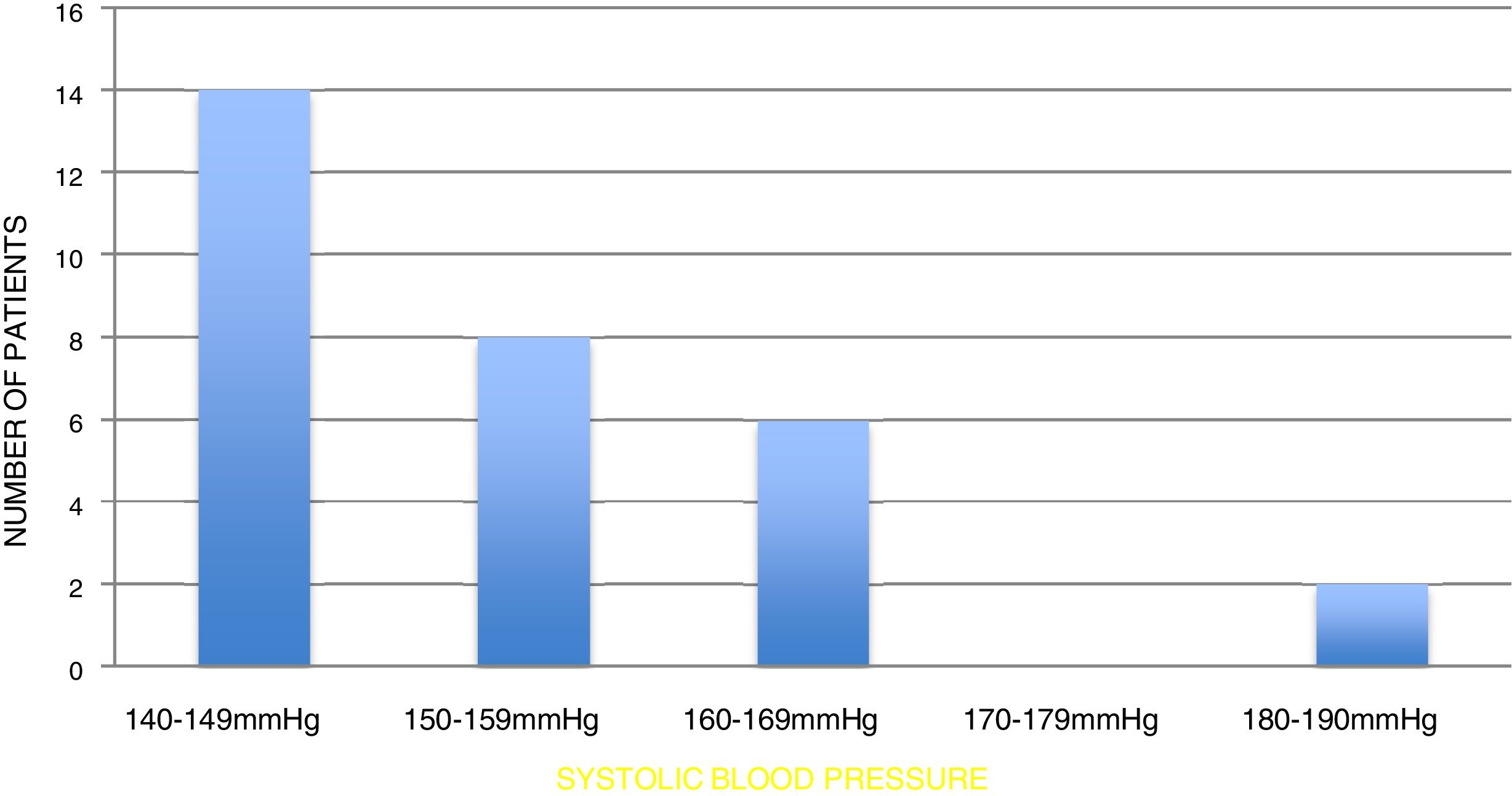
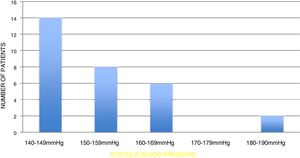
Six out of 30 patients had a systolic BP >160mm/hg with the highest value being 190mmHg. Similarly, seven out of 30 patients had a diastolic BP ≥100, the highest value being 110 (Figure 3).
Most of the patients had systolic BP in the range of 140–149mmHg and only one patient had systolic BP of 190mmHg, which was the highest value observed (Figure 3).
Platelet indices, namely platelet count, mean platelet volume, platelet distribution width, and plateletcrit, were evaluated in both cases and controls.
None of the patients had any evidence of thrombosis or organ damage. The PT/INR was within the normal range. Thus, all the patients included in the study had mild to moderate preeclampsia.
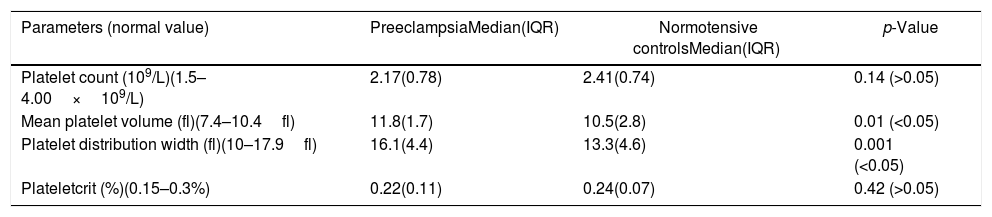
The platelet count was on the lower side in the patients with preeclampsia, as shown in Table 1 (median of 2.17×109, with interquartile range of 0.78), as compared to the healthy pregnant females (median of 2.41 with interquartile range of 0.74), however none of the patients had severe thrombocytopenia. The difference was not statistically significant with p>0.05 (Table 1). Similarly, the plateletcrit was lower in the preeclampsia group (median of 0.22%, with interquartile range of 0.11), compared to the normal healthy group (median of 0.24%, with interquartile range of 0.07), but the difference was not significant with a p>0.05 (Table 1).
Platelet indices in Preeclampsia and normotensive controls.
| Parameters (normal value) | PreeclampsiaMedian(IQR) | Normotensive controlsMedian(IQR) | p-Value |
|---|---|---|---|
| Platelet count (109/L)(1.5–4.00×109/L) | 2.17(0.78) | 2.41(0.74) | 0.14 (>0.05) |
| Mean platelet volume (fl)(7.4–10.4fl) | 11.8(1.7) | 10.5(2.8) | 0.01 (<0.05) |
| Platelet distribution width (fl)(10–17.9fl) | 16.1(4.4) | 13.3(4.6) | 0.001 (<0.05) |
| Plateletcrit (%)(0.15–0.3%) | 0.22(0.11) | 0.24(0.07) | 0.42 (>0.05) |
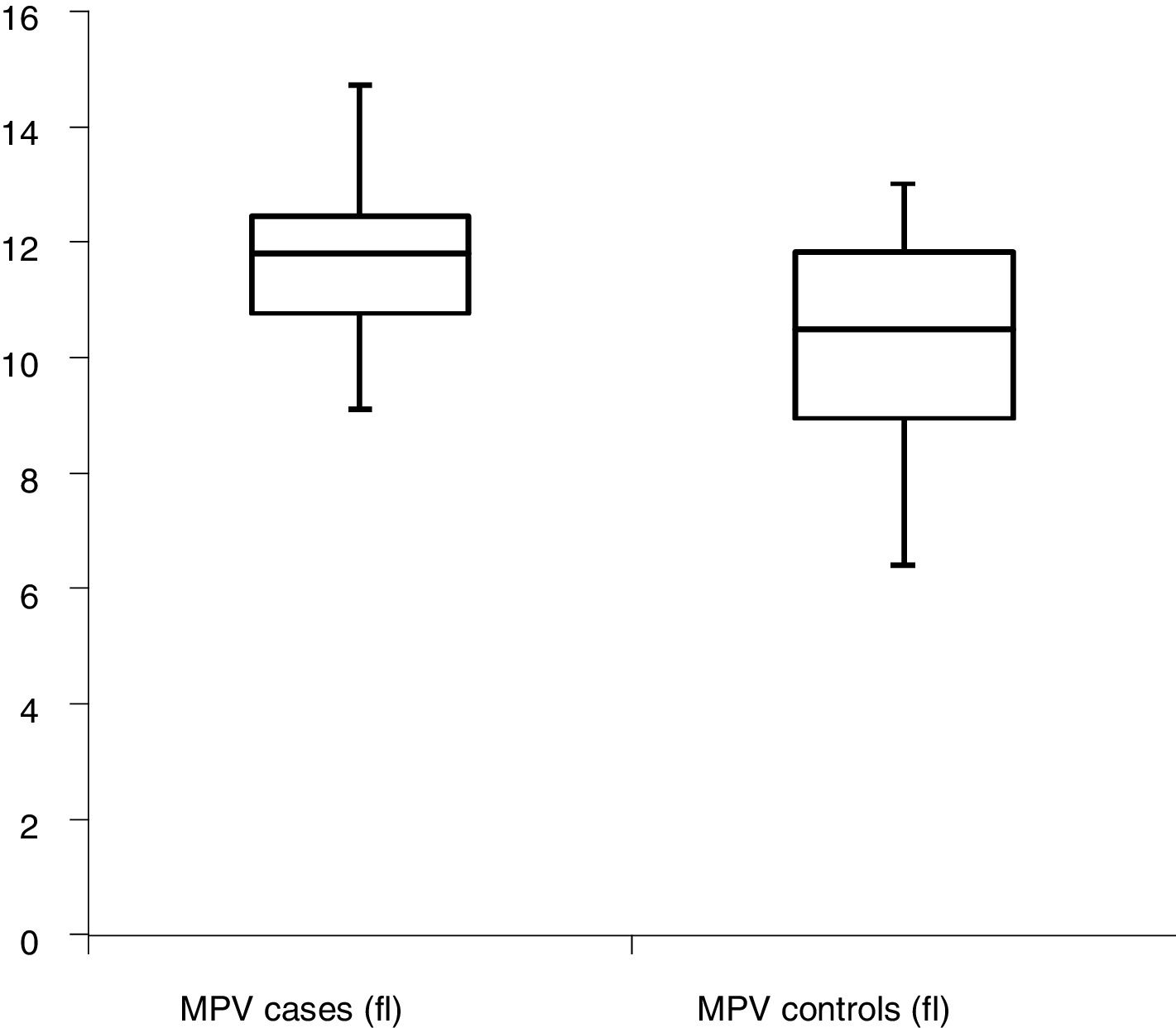
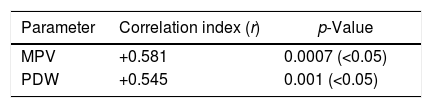
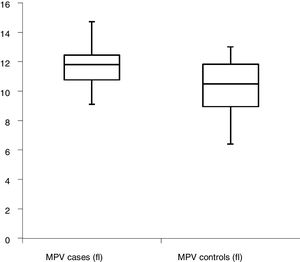
The MPV in preeclampsia and healthy females was elevated, with median values of 11.8 and 10.5 and interquartile ranges of 1.7 and 2.8, respectively. The difference between cases and controls was statistically significant, with a p<.05 (Table 1). The graphical representation of the MPV among cases and controls are depicted in Figure 4. The correlation coefficient r had a value of +0.58, indicating a positive correlation. In this case, the p value was highly significant (Table 2) and thus, it can be suggested that the increase in the MPV values is directly proportional to the increase in the blood pressure.
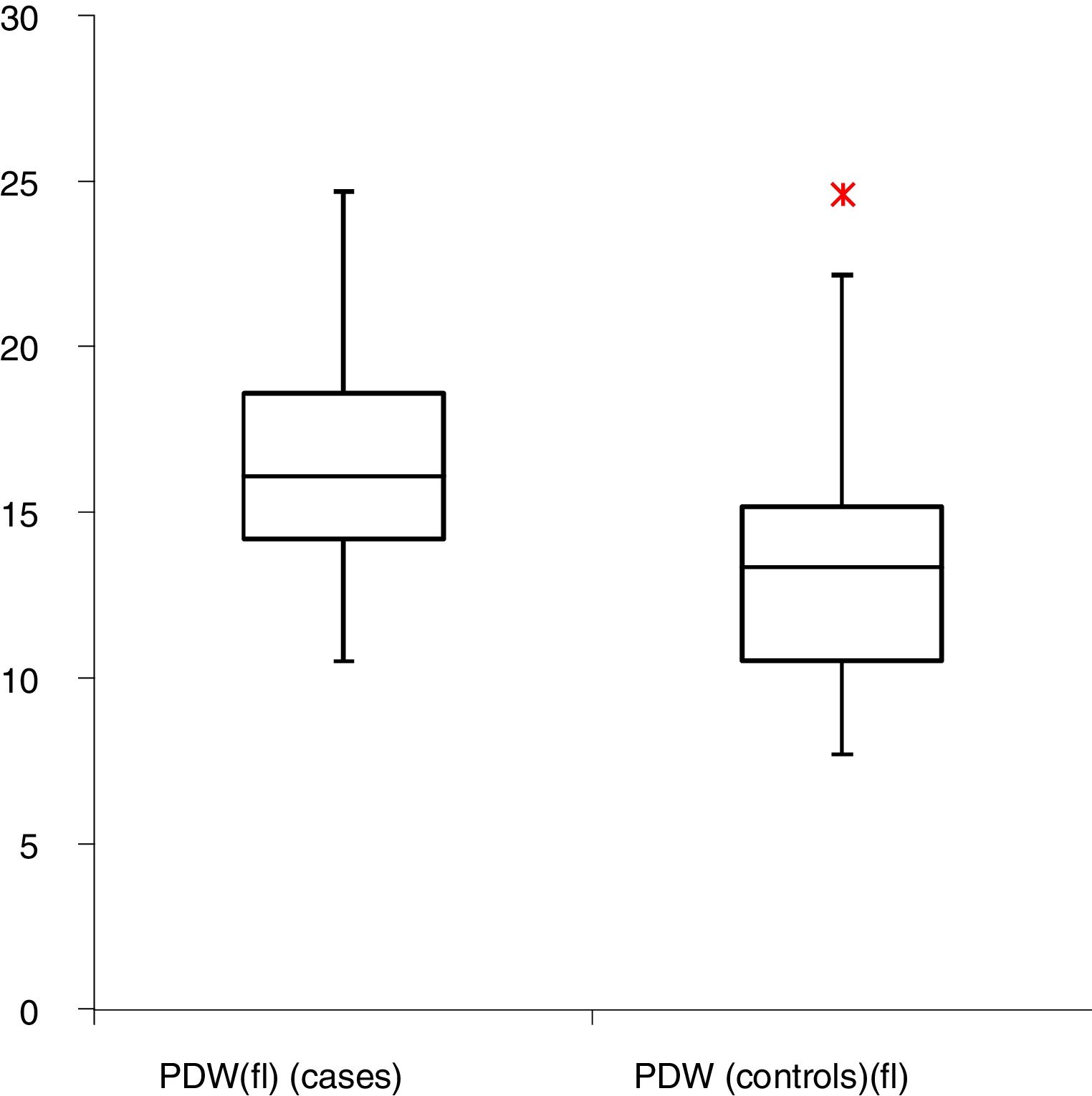
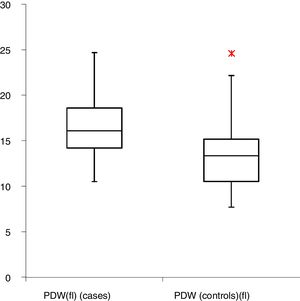
Similarly, platelet distribution width increased in both the preeclampsia group and the normotensive pregnant females, but the values were significantly higher in preeclampsia. The median value of the PDW was 16.1fl in preeclampsia and 13.3 in normotensive patients, respectively and the difference was statistically significant (p<0.05), with higher values in preeclampsia (Table 1). The graphical representation of the PDW among cases and controls is depicted in Figure 5. It was observed that the patients with higher elevations in BP had higher values of PDW. The correlation coefficient r had a value of +0.54 and a highly significant p value (Table 2).
DiscussionPregnancy induced hypertension is a significant cause of maternal and fetal morbidity and mortality in developing countries.5 The current study was undertaken to study the correlation between platelet indices and blood pressure in preeclampsia. While thrombocytopenia and low PCT values were not significant in the preeclampsia patients, in comparison to normotensive pregnant females, other parameters, namely MPV and PDW, showed a significant difference between the two groups.
Thrombocytopenia has been observed in various studies and reported to be an early marker in preeclampsia.1,4,5 A few studies have also reported decreased platelet counts as the disease progressed, but normal counts in the initial stages.7 In our study, the platelet counts were comparable between the two groups, with a slight reduction in the preeclampsia patients. Thus, the normal platelet counts in preeclampsia in our study can be explained on the basis that most of the patients had mild preeclampsia at an early gestational age (majority 20–28 weeks). Our findings regarding platelet count are consistent with the study by Han, Xiaojie, Hongmei et al.7 They too did not report a significant difference between normal and mild preeclampsia and severe preeclampsia patients and suggested that decreased platelet count may be due to the gestation itself, rather than the preeclampsia. Thus, the platelet count, though an important parameter in preeclampsia, cannot be used as a definitive marker for the same.
The mean platelet volume showed a significant difference between the two groups, with an increase in the MPV greater in preeclampsia than in normal healthy pregnant females. Similar findings were reported in several other studies as well.1–3,4,5,7–9 According to Dadhich et al. the MPV values increased with the duration of gestation, as well as the severity of the disease.3 In our study, a higher MPV was noted in patients with more severe disease, and a highly significant correlation was also found between the increased BP and MPV values. Dundar et al. found a significant increase in the MPV weeks before the diagnosis of preeclampsia.10 However, Al Sheeha et al.1 and Altinbas et al.11 have reported no significant difference between the normal healthy pregnant females and preeclampsia patients. Thus, it can be suggested that the MPV can be used as a valuable marker in the diagnosis and prediction of preeclampsia, as well as in the prognosis of the disease.
Similar to the MPV, the platelet distribution width also showed a significant increase in the preeclampsia patients, compared to the normal control group. The values were also higher in patients with more severe elevations of blood pressure. Similar findings were reported by various authors.2–5,9,12 Giles et al. reported aPDW of 16fl in preeclampsia and 12fl in normal pregnant females, which was in accordance with our study, in which the PDW was 16.84fl in preeclampsia and 13.68fl in the control group.12 A few authors have also reported no significant difference.1 We found a significant correlation of the PDW with the BP in the preeclampsia patients and it was also found that increased BP was accompanied by increased PDW values. The increase in both the MPV and PDW, which are the markers of platelet activation, suggests an active turnover of platelet production in the bone marrow due to peripheral consumption. The increase in values of both the MPV and PDW, along with increased BP, further suggests that they are also elevated in severe preeclampsia with higher elevations of BP.
The plateletcrit in our study showed a mild reduction in the preeclampsia patients and the difference of the values in the cases and controls was however not significant, with the p<0.05. Karateke et al.4 and Freitas et al.9 have demonstrated a significant decrease in the platelet concentration in preeclampsia. This could be due to the fact that in our study the platelet count in preeclampsia patients tends toward normal and the PCT is calculated using platelet counts.
All the participants in both the groups demonstrated a normal platelet count, but slight reduction in the platelet count was noted in the preeclampsia group. Both the MPV and PDW had higher values in the preeclampsia patients and in cases with higher elevations of blood pressure, the MPV and PDW was also raised. Significant elevation in the MPV was noted with elevated blood pressure. The PCT, on the other hand, was lower in the preeclampsia group, indicating a decreased concentration of platelets. These results may point toward a continuous consumption, as well as an activation of platelets.
Hence, according to our study platelet indices, namely the MPV and PDW, could be used as detection markers for preeclampsia, as well as markers for the severity of preeclampsia. The platelet count and plateletcrit, though comparable between the two groups, showed decreased values in the preeclampsia group, but statistical significance could not be found and their reliability as markers for preeclampsia cannot be commented upon.
ConclusionPreeclampsia is a serious condition which leads to maternal morbidity and mortality. The increase in the MPV and PDW was observed in preeclampsia. The MPV and PDW showed a significant correlation with increased BP. However, the platelet count and PCT in our study did not show a significant correlation with preeclampsia. Thus, the platelet indices, mainly MPV and PDW, which are easily available, as well as economical, can also be used in the prediction and early diagnosis of preeclampsia and as markers for the severity of preeclampsia, however further studies with larger numbers of patients are required.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the ICMR, New Delhi for awarding the Short Term Studentship Project to the student Nitesh Thalor (3rd Semester MBBS student).