Blood transfusions are one of the most performed medical procedures in the world. Thus, as education in transfusion medicine is vital to medical care, it should aim to promote a responsible practice with the rational use of blood by doctors. This study aims to investigate the situation of the teaching of transfusion medicine in medical schools in Brazil.
MethodThe websites of the 249 Brazilian medical schools in operation in June 2015 were visited and the curricula of the medical courses were investigated in respect to the presence or absence of a transfusion medicine discipline. When available, the subject grids were analyzed to verify whether a description of content regarding transfusion medicine was given within other disciplines.
ResultsOf the 249 medical school sites visited, information on the curriculum was obtained from 178. Of the medical schools that published their curriculum, 132 (74.1%) did not have disciplines of transfusion medicine or hematology and only seven (3.9%) had a discipline of transfusion medicine in the curricular grid.
ConclusionsEducation on transfusion medicine is of fundamental importance for safe and efficient transfusion practices. Deficiencies in medical knowledge of this subject have been found worldwide. The results of this study indicate a possible deficiency in teaching the basics of this specialty. Thus, additional prospective studies to assess the knowledge and practice of transfusion medicine in Brazilian medical schools are warranted, which could prompt a discussion on the importance of offering training in transfusion medicine to medical students.
Blood therapy, hemotherapy, or transfusion medicine is the medical specialty that deals with the use of blood, blood components and blood products as treatment. In Brazil, despite the first transfusions dating from the early twentieth century, this specialty only gained real importance in the 80s with the advent of acquired immunodeficiency syndrome (AIDS).1 Transfusion medicine is a heavily regulated practice, with specific laws guiding the complete process of blood manipulation, from collecting, processing and storage to the transfusion of blood components, as described in the Brazilian norms.2–4
Blood transfusions are the most performed procedure in American hospitals.5 In Brazil, according to the Hemovigilance Report of the Brazilian Government Health Department (Agência Nacional de Vigilância Sanitária – ANVISA) published in 2014, 3,127,957 transfusions were conducted during 2012.6 Despite becoming increasingly safe due to the improvement of serological tests, transfusions still expose the recipient to numerous risks such as transfusion-transmitted infections, sepsis, hemolytic transfusion reactions due to human error, immunomodulation and others. As most medical specialties request transfusions, critical knowledge regarding the correct indication of blood products, potential risks and expected benefits of the procedure is important in all areas for the rational use of blood.7,8
Despite the relevance of the aforementioned factors, studies conducted in different countries around the world have demonstrated insufficient knowledge of physicians on this subject. Studies have been conducted in countries such as the United States, United Kingdom, Tunisia, Canada and Iran to assess the degree of knowledge about transfusion medicine of newly graduated doctors; all studies reported lower than expected results.9–12 In a poll conducted in 86 medical schools in the United States, most had less than three hours in the curricular grid dedicated to transfusion medicine.5 This study aims to investigate the situation of the teaching of transfusion medicine in medical schools in Brazil, by analyzing curricular grids available on the internet and reviewing the literature.
MethodThe websites of the 249 Brazilian medical schools in operation in June 2015 were visited. The number of medical courses was obtained by accessing www.escolasmedicasdobrasil.com.br and the Ministry of Education website, www.emec.mec.gov.br. The curricula of the medical courses were investigated on the websites of medical schools in respect to the presence or absence of a transfusion medicine discipline. If such a specific discipline was not found, the subject grids were searched for any mention of transfusion medicine (transfusion indications or treatment of blood loss) within other disciplines, such as hematology, internal medicine or surgery.
Each undergraduate course was classified in one of the following groups:
- (i)
The course presents a transfusion medicine discipline in the curriculum.
- (ii)
The course presents transfusion medicine as a topic within the hematology discipline, but does not have a transfusion medicine discipline.
- (iii)
The course does not present a transfusion medicine or hematology discipline in the curriculum.
- (iv)
The course has no transfusion medicine or hematology discipline in the curriculum, but content on transfusion medicine is mentioned in the grid of another discipline.
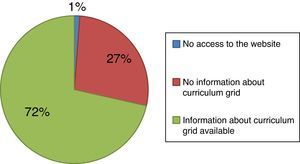
Of the 249 medical school sites visited, information on the curriculum was obtained from 178, nearly 70% of the total. Information on the curricula of the medical course was not available in 68 sites of medical schools, and access to three sites was unavailable and so they were excluded. Figure 1 shows the profile of medical schools whose sites were visited.
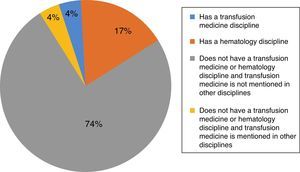
Of the schools that displayed their curriculum, about three-quarters (74.1%) did not have transfusion medicine and hematology disciplines. A smaller portion, 17,4% of the medical schools had a hematology discipline and 4.4% did not present transfusion medicine or hematology, but blood transfusions were mentioned in the grid of another discipline. Only 3.9% had a transfusion medicine discipline. The distribution frequency for the respective groups is shown in Figure 2.
DiscussionThe rational use of blood is regarded as a major issue for public health, due to poor inventory, high cost, and concerns on patient safety. Another factor to be noted is that blood, in most countries, is a product that cannot be bought, that is, its availability depends on donations. Therefore, the appropriate use of blood components avoids waste, providing proper stock maintenance to meet the needs of patients who actually have indications for blood transfusions.11
Several studies have shown the inappropriate use of blood and blood components by health professionals.13 Two systematic reviews that included intervention studies to improve transfusion practices indicate that medical education is significantly helpful in this process.14,15
Although this current study is an evaluation of the curricula of medical schools available online, the fact that only 3.9% have the discipline in the curriculum indicates a possible weakness in Brazilian medical schools with regard to transfusion medicine education. Even for those curricula having a hematology discipline, it cannot be guaranteed that transfusion medicine is included. These curricula were grouped separately because, in Brazil, hematology and transfusion medicine are a single specialty, and therefore could be taught together. As for the schools grouped as lacking transfusion medicine and hematology disciplines, although mentioning transfusion medicine in the grid of another discipline, in general, this subject was inserted into the grids of the surgery or internal medicine disciplines. As these disciplines comprise major medical areas with extensive content to be taught, it is questionable how much time is actually devoted to transfusion medicine.
Concerns about the level of knowledge of doctors with regard to transfusion medicine are universal, and several studies have shown that knowledge of doctors falls short on basic hematology issues. O’Brien et al.,16 in a study conducted in 2010 with first-year residents in Washington, noted a significant lack of knowledge about transfusion medicine regardless of the medical specialty, with scores ranging from 24% to 67% (average of 39%). In this study, 41.4% of the medical residents said they had received no formal training in transfusion medicine during their graduate courses. Another study conducted in New York with doctors from various internal medicine specialties showed a lack of knowledge of the specialty, and indicated that participants with more than five hours of formal education in transfusion medicine obtained better results.9
A study in Iran7 conducted in 2007 noted that knowledge on hematology was about a third less than the expected level. Shafiee et al.,17 in another study also conducted in Iran, analyzed the internal medicine discipline regarding knowledge on transfusion medicine and reported scores of less than 50% in issues related to transfusion reactions.
A survey conducted in the United Kingdom10 assessed knowledge about transfusion medicine of resident physicians using questionnaires, and noted that higher scores were achieved by physicians who received education about hematology during their graduate courses. Rebel et al.,18 in a study conducted in the United States, found that knowledge of anesthesiology residents related to transfusion medicine increased after they spent a period in a hematology service.
In a study conducted in South Africa, it was observed that the lack of both experts and formal training in transfusion medicine has consequences due to inadequate hemotherapeutic practices.19 A study in Tunisia assessed the degree of knowledge about hematology of interns and physicians in different specialties; the overall score was 2.9 out of 7.11 In Canada, 48% of responses were considered inadequate in a study that assessed the knowledge of 294 doctors.12
Panzer et al. conducted a study that, by using questionnaires sent to experts, sought to obtain information about transfusion medicine education in several countries, including Brazil, Iran, Australia, Sweden, Germany, India, Indonesia, Israel, Japan and France.8 The authors concluded that the education in hematology of students and residents in most countries is not universal, as the curricula vary greatly between countries and between medical schools. Interestingly, the main reason might be ascribed to the lack of a national curriculum, with the exception of Iran. The main conclusion of the forum was that transfusion medicine education should be intensified for students and residents.
A study that applied a questionnaire to evaluate the knowledge of medical residents on transfusion medicine in nine countries found significant associations between the scores and curriculum time in medical schools; those who received more than two hours of training during the medicine course had higher scores than those who did not receive training.20
In Brazil, an assessment of the participation of health professionals in transfusion practices and training of professionals, held in a university hospital, showed that doctors are involved in the application, prescription, monitoring and compliance. However, 56% did not attend any refresher course on transfusions, 89% had not received training at the institution and 33% did not feel well enough informed about the subject.21 This study suggests that more comprehensive education strategies are needed for medical professionals of different specialties.22,23
The document on the Brazilian Curriculum Guidelines for graduate courses in medicine, published in 2014, is very generic when it addresses the curricular content. The guideline mentions the “diagnosis, prognosis and therapeutic approach to diseases that affect the human being considering prevalence, mortality, potential prevention and educational importance”.24 Thus, it is up to each institution to prioritize or not particular areas, such as transfusion medicine. Although the curriculum has improved in areas such as management and therapeutic methods, transfusion medicine continues to be taught informally in most Brazilian medical schools.23 The topic is learnt in practice without adequate theoretical basis and without real knowledge of the numerous risks related to transfusions.
ConclusionLack of knowledge about transfusion medicine has been reported worldwide. In Brazil, though few studies are available on the subject, an evaluation of the curricula of medical schools demonstrated that only a small percentage has this subject as a discipline. This indicates that medical education still presents challenges. Future research may assist in assessing the significance of formal training in transfusion medicine in the curricula of medical courses, by evaluating the knowledge of Brazilian physicians about this subject and the impact in the medical practice.
Conflicts of interestThe authors declare no conflicts of interest.