To evaluate the association between clinical, pulmonary, and cardiovascular findings in patients with sickle cell disease and, secondarily, to compare these findings between sickle cell anemia patients and those with other sickle cell diseases.
MethodsFifty-nine adults were included in this cross-sectional study; 47 had sickle cell anemia, and 12 had other sickle cell diseases. All patients underwent pulmonary function tests, chest computed tomography, and echocardiography.
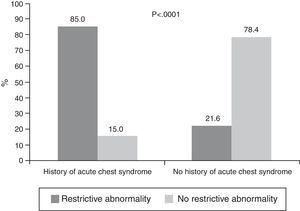
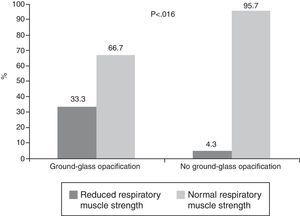
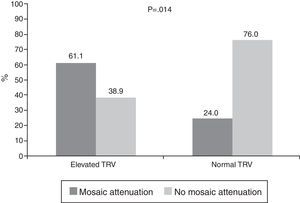
ResultsAbnormalities on computed tomography, echocardiography, and pulmonary function tests were observed in 93.5%, 75.0%; and 70.2% of patients, respectively. A higher frequency of restrictive abnormalities was observed in patients with a history of acute chest syndrome (85% vs. 21.6%; p-value<0.0001) and among patients with increased left ventricle size (48.2% vs. 22.2%; p-value=0.036), and a higher frequency of reduced respiratory muscle strength was observed in patients with a ground-glass pattern (33.3% vs. 4.3%; p-value=0.016). Moreover, a higher frequency of mosaic attenuation was observed in patients with elevated tricuspid regurgitation velocity (61.1% vs. 24%; p-value=0.014). Compared to patients with other sickle cell diseases, sickle cell anemia patients had suffered increased frequencies of acute pain episodes, and acute chest syndrome, and exhibited mosaic attenuation on computed tomography, and abnormalities on echocardiography.
ConclusionA significant interrelation between abnormalities of the pulmonary and cardiovascular systems was observed in sickle cell disease patients. Furthermore, the severity of the cardiopulmonary parameters among patients with sickle cell anemia was greater than that of patients with other sickle cell diseases.
Sickle cell disease (SCD), the most common monogenic hereditary condition in Brazil and worldwide, it affects more than 30 million people.1 It is estimated that 4% of the Brazilian population has the sickle cell trait and that between 25,000 and 50,000 individuals have the disease in the homozygous (SS) or compound heterozygous states (SC, SE, SD, and Sβ-thalassemia).2 In Brazil, SCD is unevenly distributed among the population, as it is more prevalent in the Brazilian states with the greatest numbers of individuals who are descendants of slaves.3
SCD is characterized by the presence of phenotypes that range from almost no symptoms to severe symptoms. Its onset occurs during the first year of life, and the disease extends throughout life; it is associated with high morbidity and mortality.4 The symptoms are due to hemolytic anemia and cause severely painful episodes; life-threatening complications due to bacterial sepsis, and splenic sequestration, acute chest syndrome (ACS), and chronic organ damage are also observed. All of these complications are due, at least in part, to chronic hemolysis and episodes of intermittent vascular occlusion, which lead to tissue injury and organ dysfunction. Advances in the care of SCD patients have led to increased survival, which in turn has led to the increased occurrence of chronic damage.5,6
The lung is one of the organs most involved in SCD.7 It is estimated that approximately 90% of adults with SCD have abnormal pulmonary function.8 Chronic lung disease is likely associated with recurrent episodes of ACS caused by infections, fat embolism, and pulmonary infarction.1,5,9 Pulmonary hypertension (PH) is believed to be a major cause of death in adult patients, although more recently, its incidence and pathophysiology have been extensively debated.10,11 Importantly, only 10% of SCD patients are monitored for early detection of PH.5 Its pathophysiological mechanism is complex and probably multifactorial.11,12
Cardiovascular complications have been increasingly diagnosed due to the increased longevity of SCD patients,13 who have enlarged heart chambers, an alteration that begins in adolescence.11 Cardiomegaly, chest hyperactivity, and heart murmurs are often present, mostly secondary to a state of chronic anemia, PH, and microcirculatory obstruction related to hemoglobinopathies.11,14 Cardiac iron overload is a postulated but unproven mechanism in SCD patients.14 Heart failure is uncommon, and its presence is associated with older age, coexistence of systemic hypertension and kidney failure.14 Little has been reported in the literature about the impact of the homozygous or heterozygous states on hemodynamic changes.11,15
Due to the increased life expectancy of SCD patients, many morphological and functional parameters associated with the respiratory and cardiovascular systems need to be elucidated to allow these parameters to be incorporated into patient follow-up. The hypothesis of this research was that there is a relationship between abnormalities of the respiratory and cardiovascular systems in adults with SCD. Therefore, the present study aimed to evaluate the association between clinical, pulmonary, and cardiovascular findings in SCD patients and, secondarily, to compare these findings between patients with sickle cell anemia (SCA) and patients with other sickle cell diseases (OSCD).
MethodsThis cross-sectional study was conducted between May 2013 and June 2015 and evaluated patients with SCD in regular follow-ups at the Hospital Universitário Pedro Ernesto (HUPE) of the Universidade do Estado do Rio de Janeiro (UERJ). Patients aged ≥18 years with SCA or OSCD were included. Exclusion criteria were a blood transfusion within the previous three months, a vaso-occlusive pain episode within the previous month, reports of heart disease or lung disease unrelated to SCD, a smoking history of >10 pack-years, and a history of respiratory infection in the previous three weeks. Pack-years was calculated by multiplying the number of packs of cigarettes smoked per day by the number of years the person had smoked.16 Based on these criteria, twelve patients were excluded for the following reasons: significant history of smoking (n=5), blood transfusion in the previous three months (n=5), and vaso-occlusive pain episodes in the previous month (n=2).
Among the 59 study participants, forty-seven had SCA, and 12 had OSCD (10 patients had the Hemoglobin (Hb) SC form, and two patients had the Hb SD form). No patient had the heterozygous Sβ form of SCD. The study was approved by the Research Ethics Committee of HUPE-UERJ (number 231.033), and all participants signed an informed consent form. The study was conducted in accordance with the Helsinki Declaration as revised in 2008.
Using a computerized system (Collins Plus Pulmonary Function Testing Systems, Warren E. Collins, Inc., Braintree, MA, USA), spirometry, whole-body plethysmography, and respiratory muscle strength (RMS) were evaluated. The pulmonary function tests (PFTs) followed the standards and interpretation established by the American Thoracic Society (ATS).17 The equations of Pereira (spirometry) and Neder (whole-body plethysmography and measurement of RMS) were used to interpret the functional parameters.18–20 Restrictive abnormalities were diagnosed when the total lung capacity (TLC) was below the lower limits of normal (LLN), and obstructive abnormalities were diagnosed when the forced expiratory volume in one second/forced vital capacity (FEV1/FVC) ratio was below the LLN.17
Chest computed tomography (CT) scans (including the upper abdomen) were performed using a 64-channel multislice CT scanner (Brilliance 40, Philips Medical Systems, Cleveland, OH, USA). The images were acquired in the axial plane, with the patient supine, using the following technical parameters: 120kV and 130–190mA, section thickness of 2mm, and pitch of 1 between the jugular notch and the xiphoid process, with maximal inspiration and expiration and without gantry tilt. After image acquisition, reconstruction was performed at high resolution with a 512×512 matrix using a high-frequency algorithm, window width of 1200HU, and middle center of −800HU. Intravenous contrast was not used in any of the tests performed. The CT findings were interpreted independently by two radiologists, and a consensus was established in cases of disagreement. The following CT findings were evaluated: reticular pattern, ground-glass opacification (GGO), mosaic attenuation, lobar volume loss, and traction bronchiectasis.21,22 The spleen size was also evaluated in this study by CT.
Transthoracic Doppler echocardiography was performed by the same examiner using an iE33 system (Philips Medical Systems, MA, USA). The images were stored on digital media and reviewed by a second examiner; both examiners were blinded to the patient groups. Tricuspid regurgitation velocity (TRV) was considered high when the value was ≥2.5ms−1.23
Statistical analysisThe Shapiro–Wilk test was used to evaluate sample homogeneity. The results are expressed as median values and interquartile ranges or numbers (percentages). Inferential analysis included the chi-square test or Fisher's exact test to compare the findings with categorical data and the Mann–Whitney test or Kruskal–Wallis ANOVA to compare findings with numerical data. Dunn's multiple comparison test was applied to identify subpopulations that differed significantly. Data were analyzed using SAS software version 6.11 (SAS Institute, Inc., Cary, NC, USA). p-Values<0.05 were considered statistically significant.
ResultsThe study population (n=59) included 32 women and 27 men, with a median age of 27 (range: 22–39) years. The median Hb level was 8.32 (range: 7.60–10)g/dL. Abnormalities on CT scans, echocardiography, and PFTs were observed in 93.5%, 75.0%, and 70.2% of the patients, respectively. The clinical features as well as the PFT, CT, and echocardiography results are shown in Table 1.
Clinical data, lung function, computed tomography abnormalities, and echocardiography findings of 59 patients.
| Variable | Value – n (%) |
|---|---|
| Clinical data (n=59) | |
| Male gender | 27 (45.8) |
| Afro-descendant | 59 (100) |
| History of vaso-occlusive pain episode | |
| None | 22 (37.3) |
| 1/year | 26 (44.1) |
| ≥2/year | 11 (18.7) |
| History of acute chest syndrome | 25 (42.4) |
| History of asthma | 9 (15.3) |
| History of stroke | 6 (10.2) |
| History of seizures | 4 (6.78) |
| History of avascular necrosis | 15 (25.4) |
| History of acute splenic sequestration | 8 (13.6) |
| History of transfusions | |
| None | 16 (27.1) |
| 1/year | 31 (52.5) |
| ≥2/year | 12 (20.3) |
| History of infections | |
| None | 16 (27.1) |
| 1/year | 32 (54.2) |
| ≥2/year | 11 (18.7) |
| History of hospitalizations | |
| None | 18 (30.5) |
| 1/year | 32 (54.2) |
| ≥2/year | 9 (15.3) |
| Hydroxyurea therapy | 34 (57.6) |
| Lung function (n=57) | |
| No abnormality | 17 (29.8) |
| Restrictive abnormality | 20 (35.1) |
| Obstructive abnormality | 7 (12.3) |
| Reduced respiratory muscle strength | 29 (50.9) |
| Computed tomography (n=46) | |
| No abnormality | 3 (6.50) |
| Reticular pattern | 10 (21.7) |
| Ground-glass opacification | 9 (19.6) |
| Mosaic attenuation | 18 (39.1) |
| Lobar volume loss | 20 (43.5) |
| Traction bronchiectasis | 4 (8.70) |
| Spleen | |
| No abnormality | 6 (13) |
| Atrophic | 36 (78.3) |
| Splenomegaly | 4 (8.70) |
| Echocardiography (n=56) | |
| No abnormality | 14 (25) |
| Increased right atrium | 6 (10.7) |
| Increased right ventricle | 6 (10.7) |
| Increased left atrium | 37 (66.1) |
| Increased left ventricle | 29 (51.8) |
| Elevated tricuspid regurgitation velocity | 25 (44.6) |
| Diastolic dysfunction | 9 (16.1) |
A comparison of patients with and without abnormalities in the PFTs found no significant differences in clinical, CT, or echocardiography findings. However, a higher frequency of restrictive abnormalities was observed in the PFTs of patients with a history of acute chest syndrome (Figure 1). A higher frequency of reduced RMS was also observed in the PFTs of patients with a GGO pattern on CT (Figure 2).
A comparison of patients with and without abnormalities on CT scans found no significant differences in the clinical, PFT, or echocardiography findings. However, the Hb levels were significantly different between patients with a normal spleen [8.90 (range: 7.40–10)g/dL], splenic atrophy [8.20 (range: 7.70–9.70)g/dL], and splenomegaly [10.9 (range: 10–12)g/dL] on CT scans (p-value=0.025).
A comparison of patients with and without abnormalities on echocardiography found a significant difference between patients with and without a mosaic attenuation pattern observed on CT scans, as well as a higher frequency of mosaic attenuation pattern in patients with abnormal echocardiography (50% vs. 15.4%; p-value=0.033) and with elevated TRV (Figure 3). Moreover, lower serum Hb levels were observed in patients with abnormal echocardiography [(8.13 (range: 7.32–8.37) vs. 10.1 (range: 9.40–11.7)g/dL; p-value=0.0006)] and in those with elevated TRV [8.10 (range: 7.25–9.34) vs. 9.42 (range: 7.81–10.6)g/dL; p-value=0.023]. A comparison of patients with and without increased left ventricle (LV) size found a higher frequency of restrictive abnormalities among those with increased LV size (48.2% vs. 22.2%; p-value=0.036). A comparison of patients with and without increased right atrium (RA) size and increased right ventricle (RV) size revealed a higher frequency of parenchymal abnormalities on CT scans (40% vs. 2.6%; p-value=0.028).
A comparison of SCA and OSCD patients revealed no significant age difference [27 (range: 22–41) years in the SCA group vs. 26 (range: 23–36) years in the OSCD group; p-value=0.90]. However, Hb levels differed significantly between these two groups [8.10 (range: 7.40–8.90)g/dL in the SCA group vs. 11.1 (range: 10.0–12.9)g/dL in the OSCD group; p-value=0.0001]. A history of leg ulcers and priapism was reported in seven and six SCA patients, respectively; however, none of the OSCD patients had a history of priapism or leg ulcers. Comparisons of clinical, PFT, CT, and echocardiography data between the two groups are shown in Table 2.
Clinical findings, lung function, computed tomography abnormalities, and echocardiography.
| Variable | SCA group | OSCD group | p-value |
|---|---|---|---|
| Clinical data (n=59) | (n=47) | (n=12) | |
| Male gender | 22 (46.8) | 5 (41.7) | 0.83a |
| Afro-descendant | 47 (100) | 12 (100) | 1.00a |
| History of vaso-occlusive pain episode | |||
| None | 13 (27.7) | 9 (75) | 0.009a |
| 1/year | 23 (48.9) | 3 (25) | |
| ≥2/year | 11 (23.4) | 0 (0) | |
| History of acute chest syndrome | 24 (51.1) | 1 (8.30) | 0.008b |
| History of asthma | 7 (14.9) | 2 (16.7) | 0.27a |
| History of stroke | 6 (12.8) | 0 (0) | 0.24a |
| History of seizures | 4 (8.51) | 0 (0) | 0.19a |
| History of avascular necrosis | 13 (27.7) | 2 (16.7) | 0.52a |
| History of acute splenic sequestration | 8 (17) | 0 (0) | 0.14a |
| History of transfusions | |||
| None | 6 (12.8) | 10 (83.3) | <0.0001a |
| 1/year | 29 (61.7) | 2 (16.7) | |
| ≥2/year | 12 (25.5) | 0 (0) | |
| History of infections | |||
| None | 8 (17) | 8 (66.7) | 0.003a |
| 1/year | 29 (61.7) | 3 (25) | |
| ≥2/year | 10 (21.3) | 1 (8.33) | |
| History of hospitalizations | |||
| None | 9 (19.2) | 9 (75) | 0.001a |
| 1/year | 29 (61.7) | 3 (25) | |
| ≥2/year | 9 (19.2) | 0 (0) | |
| Hydroxyurea therapy | 33 (70.2) | 1 (8.30) | <0.0001b |
| Lung function (n=57) | (n=45) | (n=12) | |
| No abnormality | 11 (24.4) | 6 (50) | 0.088a |
| Restrictive abnormality | 18 (40) | 2 (16.7) | 0.12a |
| Obstructive abnormality | 6 (13.3) | 1 (8.33) | 0.54a |
| Reduced respiratory muscle strength | 23 (51.1) | 6 (50) | 0.95b |
| Computed tomography (n=46) | (n=37) | (n=9) | |
| No abnormality | 2 (5.40) | 1 (11.1) | 0.49a |
| Reticular pattern | 9 (24.3) | 1 (11.1) | 0.36a |
| Ground-glass opacification | 7 (18.9) | 2 (22.2) | 0.57a |
| Mosaic attenuation | 17 (46) | 1 (11.1) | 0.038a |
| Lobar volume loss | 15 (40.5) | 5 (55.6) | 0.33a |
| Traction bronchiectasis | 4 (10.8) | 0 (0) | 0.41a |
| Spleen | |||
| No abnormality | 4 (10.8) | 2 (22.2) | 0.0001a |
| Atrophic | 33 (89.2) | 3 (33.3) | |
| Splenomegaly | 0 (0) | 4 (44.4) | |
| Echocardiography (n=56) | (n=44) | (n=12) | |
| No abnormality | 6 (13.6) | 8 (66.7) | 0.0006a |
| Increased right atrium | 6 (13.6) | 0 (0) | 0.22a |
| Increased right ventricle | 6 (13.6) | 0 (0) | 0.22a |
| Increased left atrium | 33 (75) | 4 (33.3) | 0.010a |
| Increased left ventricle | 27 (61.4) | 2 (16.7) | 0.006b |
| Elevated tricuspid regurgitation velocity | 24 (54.6) | 1 (8.33) | 0.004b |
| Diastolic dysfunction | 8 (18.2) | 1 (8.33) | 0.61a |
Results expressed as numbers (percentages). SCA: sickle cell anemia; OSCD: other sickle cell diseases.
The main findings of this study are that cardiopulmonary abnormalities, comprising both the structure and function of the cardiac and pulmonary systems, are frequent in adults with SCD. The restrictive abnormalities observed on the PFTs are associated with a much higher frequency of ACS and increased LV size. In addition, a significant association was found between decreased RMS and a higher frequency of a GGO pattern on CT scans. Patients with elevated TRV showed a higher frequency of mosaic attenuation on CT scans and lower serum Hb levels. Compared to the OSCD group, SCA patients were more likely to have a history of vaso-occlusive pain episodes, a history of ACS, a mosaic attenuation pattern on CT scans, and abnormalities on echocardiography; all of these findings showed significant differences between the two groups.
The respiratory and cardiovascular systems are the most important systems involved in SCD and are responsible for the significant morbidity and mortality of the disease. In the present study, evaluations using PFTs, CT, and echocardiography in adult patients showed a high frequency of impairment of the lungs (93.5%) and heart (75%), with these results being similar to those found in other studies.8,10,21,22,24 With an increasing life expectancy of SCD patients, a higher percentage of this population is expected to develop chronic complications, including pulmonary fibrosis and PH.25
Previous studies have suggested that the detection of abnormalities in PFTs is the first clear sign of chronic sickle cell lung disease; therefore, these tests could be valuable for patient management and follow-up.7,8 Similar to the studies conducted by Lunt et al.21 and Sylvester et al.,22 restrictive abnormalities were observed in 35.1% of the patients evaluated in the current study. An association between restrictive damage and a higher frequency of ACS was also observed, which can be explained, at least in part, by chronic hemolysis and repeated episodes of intermittent vascular occlusion, which lead to tissue damage.8,22 In contrast to the study by Delclaux et al.,24 which found no association between echocardiographic findings and the parameters obtained in the PFTs, an association between restrictive abnormalities and increased LV size was observed in this study. This is not surprising because LV dilation can reduce lung volume via several mechanisms, including pulmonary congestion and the direct effect of compression of the heart on the pulmonary parenchyma.26 Therefore, a cardiac evaluation should be performed in the absence of an apparent pulmonary cause that justifies the restrictive abnormality observed in PFTs.
In the present study, the impairment of RMS was observed in 50% of patients and was the most commonly observed abnormality in the PFTs. Ohara et al.27 recently reported cases of weakness of the respiratory muscles in SCD patients. Several mechanisms may be involved in decreased RMS in these patients, including shallow breathing due to chest pain, subacute vaso-occlusion, which affects muscle performance, and deformities of the thoracic cavity resulting from successive bone infarctions and osteoporosis.27,28 Interestingly, an association between decreased RMS and the appearance of a GGO pattern on CT scans was found in the current study. Previous research had reported a high frequency of a GGO pattern in SCD patients but did not evaluate its association with pulmonary function.8,21,22 The GGO pattern on CT scans is nonspecific and may reflect the occurrence of different mechanisms. The results of this study suggest that the partial collapse of the airway spaces after inspiration resulting from respiratory muscle weakness could explain, at least in part, this association.29
Recent studies have shown that increased cardiac output, rather than primary changes in pulmonary microvasculature, appears to be responsible for changes in pulmonary hemodynamics in SCD patients.10,11 Mushemi-Blake et al.10 recently demonstrated, via right heart catheterization (RHC), that although more than 35% of patients have elevated TRV, less than 5% have PH. Therefore, the present study used the measurement of TRV instead of the estimation of systolic pulmonary artery pressure. Interestingly, an association between elevated TRV and the appearance of a mosaic attenuation pattern on CT was observed, which is indicative of both occlusive vascular disease and obstructive disease of the small airways.30 The elevated TRV and low serum Hb levels observed in the present study have been reported previously.10
The present study showed higher frequencies of history of vaso-occlusive pain episodes, history of ACS, a mosaic attenuation pattern on CT scans, and echocardiographic changes in SCA patients than in those with OSCD. However, no significant differences were observed in the parameters found in the PFTs. Koumbourlis et al.15 observed normal pulmonary function in children with the Hb SC form of SCD and decreases in pulmonary function over time in a manner similar to that observed in SCA children. Because this study evaluated only adult patients, the absence of significant differences between the two groups in the PFTs seems to be supported, at least in part, by the progressive decline in lung function that occurs from childhood to adulthood. Notably, the two groups presented a high percentage of patients with reduced RMS (51.1% vs. 50.0%).
Some limitations of this study should be mentioned. First, the small sample size of the study and its cross-sectional nature limit an analysis of cause and effect. Second, RHC, which could help assess the impact of cardiopulmonary hemodynamics on the parameters evaluated, was not performed in the study participants. However, RHC is an invasive method and has inherent risks, which makes its implementation impractical in all patients. Despite these limitations, the results justify further research on certain aspects of SCD, including the involvement of RMS, as it may elucidate the pathophysiological mechanisms involved in this disease and assist in the design of rehabilitation programs.
ConclusionIn SCD patients, a significant interrelation between abnormalities of the structure and function of pulmonary and cardiovascular systems was observed. Restrictive abnormalities are associated with increased LV size, whereas a mosaic attenuation pattern on CT scans is associated with elevated TRV. In these patients, an association was observed between reduced RMS and the appearance of a GGO pattern on CT scans. Furthermore, the severity of the cardiopulmonary parameters among SCA patients was higher than that among OSCD patients.
Conflicts of interestThe authors declare no conflicts of interest.