The immature platelet and immature reticulocyte fractions represent the ratios of platelets and reticulocytes recently released into the circulation and thus with higher RNA content. They are considered early indicators of bone marrow recovery.
ObjectiveThe aim of this study was to determine the reference ranges for the immature platelet and reticulocyte fractions of hematologically normal individuals in a university hospital.
MethodsVenous blood samples collected in ethylenediaminetetraacetic acid K3 were analyzed using a Sysmex XE-5000™ analyzer. Individuals with platelet and reticulocyte counts within the reference ranges, and a blood count within the laboratory's screening criteria were included. Individuals with clinical conditions that could affect hematological results were excluded. The immature platelet fraction, high, medium and low fluorescence reticulocyte fractions and reticulocyte hemoglobin equivalent were evaluated. The reference ranges were determined according to the recommendations of the International Federation of Clinical Chemistry.
ResultsOne hundred and thirty-two outpatients were evaluated. The mean age was 44 years (range: 13–80 years), 72 (54.5%) were women treated in a university hospital. The mean platelet count was 250.8×109/L and the mean reticulocyte count was 0.052×109/L. The following reference ranges were obtained: immature reticulocyte fraction 1.6–12.1%, the high, medium and low fluorescence reticulocyte fractions were 0.0–1.7%, 1.6–11.0% and 87.9–98.4%, respectively, the reticulocyte hemoglobin equivalent was 30.0–37.6% and immature platelet fraction was 0.8–5.6%. There was a statistically significant difference (p-value=0.006) between genders in respect to the immature platelet fraction with 0.8–4.7% for females and 0.7–6.1% for males. The immature reticulocyte fraction was directly correlated with the reticulocyte count.
ConclusionDetermining the reference range is critical to the introduction of a new parameter. The reference ranges obtained herein corroborate those reported in previous publications and will contribute to the clinical and laboratory application of the indices.
Recent advances in the field of hematology analyzers used in clinical laboratories allow the determination of additional hematologic parameters, providing useful information for the diagnosis and/or treatment of various pathologies.1 Among these parameters are the immature fractions of platelets and reticulocytes.1–3
The immature platelet fraction (IPF) and immature reticulocyte fraction (IRF) are young cells that have recently been released into the circulation, and are considered indicators of bone marrow recovery.1–3 They are important in various clinical situations, such as thrombocytopenia, anemia, bone marrow regeneration following the transplantation of hematopoietic stem cells and after chemotherapy.2,4–13
The IPF and IRF are determined using hematology analyzers with fluorescence and light scatter technology. Immature fractions have larger amounts of RNA than mature platelets and reticulocytes. Thus, the use of fluorescent probes that label the RNA permit the differentiation and quantification of the IRF and IPF.1–3,6 Automated systems provide a graphic display of the different populations according to the size and amount of RNA. Based on this, the indices are calculated as a percentage of total reticulocytes and platelets.1–3,6
Different populations of reticulocytes are separated according to the size and the amount of RNA and classified as being low (LFR), medium (MFR) or high (HFR) fluorescence reticulocyte fractions. The combined counts of the HFR and MFR correspond to IRF. The reticulocyte hemoglobin equivalent (Ret-He) parameter corresponds to the hemoglobin content of the reticulocytes, and is studied as an indicator of the incorporation of iron in reticulocytes.15–18
Advances in automation have provided additional blood count parameters that enable new interpretations of the examination. However, clinical application can only occur once the reference ranges have been determined with knowledge of pre-analytical variables (time, temperature, anticoagulants) and standardization of the methodology.1,2,16,17,19–21
Some reference ranges have been calculated by the manufacturer, while others have not yet been determined. Thus, it is recommended that each laboratory calculates the reference range for its population, taking into account the routine and the methodology used.22–24 Subjects should be stratified by age and gender and meet strict criteria in the selection of the individuals in the pre-analytical and analytical phases and for statistical analysis.22–24
This study aims to determine the reference ranges for the IPF, IRF, LFR, MFR, HFR and Ret-HE in hematologically normal patients treated at a university hospital, in order to study the roles of the parameters as predictors of engraftment in bone marrow transplantation, one of their main clinical applications.
MethodsVenous blood samples collected in ethylenediaminetetraacetic acid K3 (EDTA-K3) were analyzed in a Sysmex XE-5000™ analyzer (Sysmex Corporation, Japan). To minimize variations due to sample age, all assays were performed within four hours of collection; the samples were kept at room temperature until the time of analysis. The analyzer uses the same reagent to measure the IPF and IRF in the reticulocyte channel.
The platelet detection method employs hydrodynamic focus and direct current technology. The IPF and IRF are determined by fluorescence and light scatter using fluorescent RNA markers.1–3 The Ret-He is obtained by flow cytometry technology using a polymethine dye, specific for RNA/DNA. The forward light scatter intensity correlates to the cellular hemoglobin content.
Patients with normal blood counts within the screening criteria established by the laboratory such as hemoglobin greater than 12.0g/dL and platelet and reticulocyte count values within the normal ranges (platelet count greater than 150.0×109/L and reticulocytes 25–80×109/L) were included. Patients with diabetes, human immunodeficiency virus (HIV), cardiovascular diseases, pregnant women, hematologic diseases, cancer, and thyroid disease were excluded, as these conditions may affect the hematological results.19–21
The IPF, IRF, the reticulocyte ratios (HFR, MFR and LFR) and Ret-He were evaluated. Assays were routinely submitted to internal and external quality controls.
Statistical analysisThe reference ranges were determined using of the Statistical Package for Social Sciences version 18.0 (SPSS Inc., Chicago, IL, USA). Symmetric variables are expressed as the mean and standard deviation, while asymmetric variables are expressed as the median, 2.5–97.5 percentiles within a 95% confidence interval, as recommended by the International Federation of Clinical Chemistry (IFCC).22–24 Spearman's and Pearson's correlation tests were also used.
ResultsOne hundred and thirty-two outpatients were evaluated. The mean age was 44 years (range: 13–80) and 72 (54.5%) were women treated at a university hospital. The mean platelet count was 250.8×109/L and the mean reticulocyte concentration was 1.1% (range: 0.6–1.7%) with a count of 52×109/L (range: 49–54×109/L).
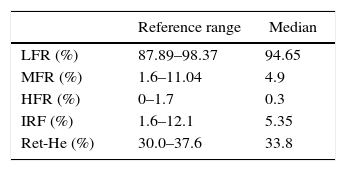
The median value of the IRF was 5.3% with a range of 1.6–12.1%. The reference ranges of the HFR, MFR and LFR were 0.0–1.7%, 1.6–11.0% and 87.9–98.4%, respectively. The mean Ret-He was 33.8% with a range of 30.0–37.6% (Table 1).
Reference interval and median for reticulocyte index.
| Reference range | Median | |
|---|---|---|
| LFR (%) | 87.89–98.37 | 94.65 |
| MFR (%) | 1.6–11.04 | 4.9 |
| HFR (%) | 0–1.7 | 0.3 |
| IRF (%) | 1.6–12.1 | 5.35 |
| Ret-He (%) | 30.0–37.6 | 33.8 |
LFR: low fluorescence ratio; MFR: medium fluorescence ratio; HFR: high fluorescence ratio; IRF: immature reticulocyte fraction; Ret-He: reticulocyte hemoglobin equivalent.
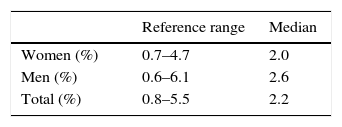
The median IPF was 2.2% with a range of 0.8–5.6%. A statistically significant difference (p-value=0.006) between genders was only found for the IPF, with 2.0% for females (range: 0.8–4.7%) and 2.6% for males (range: 0.7–6.1%). The IRF presented a direct correlation (Spearman Rank-order Coefficient=0.40) with the reticulocyte count (Table 2).
DiscussionAlthough not directly used in clinical decision making, the reference range is critical to the introduction of new parameters and the interpretation of laboratory results.22–24 The reference range shows the variation of likely values in ‘healthy’ individuals who do not present clinical conditions that can affect the studied variables.22–24
Immature platelets and immature reticulocytes are precursor cells recently released into the blood stream that contain larger amounts of RNA. Thus, they can be distinguished from the mature platelets and reticulocytes and quantified using RNA fluorescent labeling.1–3 Several studies have demonstrated the value of these indices in the context of hematopoietic stem cell transplantation as indicators of hematopoiesis, in transfusion assessment and the anticipation of successful engraftment.1–8 The Ret-He is useful in the evaluation of hematopoiesis, with respect to the incorporation of iron.14–17
The reference range obtained for the IPF was in accordance with the studies by Takami et al. (mean 2.0%; range: 0.5–5.7%),9 Gonzalo et al. (median: 2.3%; range: 0.6–7.2%),4 Yamaoka et al. (mean of 3.0±1%),8 and Briggs et al. (range: 1.1–6.1%).2 The study by Ko et al. found lower IPF values (range: 0.5–3.3%).18
The reference range for the IRF was similar to that of Gonzalo et al. who obtained a median of 4.7% (range: 1.1–11.4%).4 Although they used the same methodology, these studies were conducted with the use of a Sysmex XE-2100™ analyzer. Other authors employed other methodologies to determine the reference ranges for the IPF and IRF and so they were not compared with the results of the current study.
Determining the reference range involves several steps, including selection of subjects, methodology and statistical analysis.22–24 It is essential that it is carried out for new parameters that are not widely used by laboratories and clinics. The reference ranges for the IRF and IPF reported in this study are consistent with the literature and will contribute to the clinical application of these indices.
Conflicts of interestThe authors declare no conflicts of interest.
We would like to thank the staff at the Hematology Unit, Department of Clinical Pathology, Hospital de Clínicas de Porto Alegre.