Hematology Specialist Association 18. National Congress
Mais dadosCancer remains a significant challenge within the healthcare system. According to the 2022 GLOBOCAN report, approximately 20 million people were diagnosed with cancer, and 10 million people passed away due to the disease. A significant improvement in the prevention, diagnosis, and treatment of cancer has resulted in a greater chance of overall survival for patients. Although survival rates for these patients have improved, they may be at risk for secondary malignancies.
Secondary malignancy (SM) is defined as a tumor that differ from the primary tumor in terms of location, histopathology and genetics. Secondary malignancies could be classified into two categories based on the time of occurrence: synchronous tumors occur within six months of an initial primary cancer, while metachronous tumors occur after six months. Despite various genetic and environmental factors being implicated, the pathogenesis remains unclear. There are no standard protocols for screening, prevention, diagnosis, or treatment. Additionally, most studies on this topic conducted on data from the SEER (Surveillance, Epidemiology, and End Results) database. Although this database has the advantage of including many patients, it is insufficient to examine potential risk factors because it doesn't include individual medical information such as personal and family medical history, or alcohol and smoking use.
In this study, we aimed to reveal the incidence of secondary malignancy in hematological cancer patients, analyze the potential risk factors and determine which factors are associated with the development of secondary malignancies.
MethodologyThis retrospective study was conducted on 2,003 patients diagnosed with Hodgkin Lymphoma (HL), Non-Hodgkin Lymphoma (NHL), Chronic Lymphocytic Leukemia (CLL), Essential Thrombocytosis (ET), Chronic Myeloid Leukemia (CML), Primary Myelofibrosis (PMF), Polycythemia Vera (PV), Myelodysplastic Syndrome (MDS) and Multiple Myeloma (MM) who applied to the Hematology Clinic of Bezmialem Vakif University Hospital between February 2012 and May 2024. Patients aged above 18 years and had adequate medical records were included in the study. Patients with a prior history of cancer or an inadequate medical history were excluded.
The study group consisted of patients with secondary malignancies. Control subjects were matched to the study group based on age, gender, and diagnosis. Clinical parameters compared between the study and control groups included age, gender, presence of B symptoms, stage (early or advanced), primary involvement (nodal or extranodal), extranodal involvement, relapse, hematopoietic stem cell transplantation (HSCT), treatments received (radiotherapy and chemotherapy), modifiable risk factors (diabetes, hypertension, smoking, alcohol use), and a family history of cancer.
For statistical analysis, occurrences of SM by the site of diagnosis were described by counts and frequencies. Differences between groups were evaluated by the pearson chi- square or fisher exact test. Logistic regression models were used to determine predictors of occurrence of SM in patients with hematological malignancies. Survival probabilities and relapse were estimated using the Kaplan-Meier method. Cox regression analysis was performed to evaluate the factors affecting survival times and relapse. The hazard ratio (HR) with corresponding 95% confidence interval was determined based on the Cox proportional hazards model. Statistical significance level was set as 0.05 and SPSS (version 28) package program was used in calculations. All p values < 0.05 were considered statistically significant.
This study was approved by Bezmialem Vakif University Ethical Committee (2024/50).
Results1,757 of 2,003 hematological malignancies were analyzed, 51 of whom developed SM. There was no SM in patients with PV, and one patient with MDS was excluded for inadequate records. A total of 248 cases were selected as controls. The 299 patients with hematological malignancies had a median follow-up of 70 months (95% CI 46.7-93.2) and a median age of 64 years (range 24-89), and 154 (51.50%) were female. Among these 51 cases of SM, the mean time to secondary malignancy development was 103.61 months (95% CI 88.7-118.4), and 11 had synchronous (21.6%) and 40 had metachronous (78.4%) tumors (Figure-1A). A majority of SM were found in Non-Hodgkin Lymphoma (NHL) (n=26, 51%). The most common type of SM was lung cancer (n=9, 17.6%) (Figure-1B).
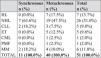
In terms of age, gender, B symptoms, stage, primary and extranodal involvement, HSCT, chemotherapy, or modifiable risk factors, there was no statistically significant difference between patients with and without SPM. However, relapse and radiotherapy were significantly more common in the control (p=0.023 and p=0.038, respectively). Moreover, a family history of cancer was statistically significant in the study group (p= <0.001) (Table-1). In the multivariate logistic regression analyses, family history of cancer, no relapse, and no radiotherapy were associated with an increased risk of secondary cancer (Table-2).
There were no significant differences in survival times between the groups (Figure-2A). Cox multivariate analysis showed advanced age and male gender to be risk factors for OS (Table-3).
The mean time to relapse for hematologic malignancies was 106.6 months (range 98.8–114.4 months). SM patients had a longer time to relapse than controls (p=0.004) (Figure-2B). Cox multivariate analysis showed that patients who got autologous transplantation and those who did not develop secondary malignancy were at higher risk of relapse (Table-3).
ConclusionIn conclusion, this study indicates that a family history, no relapse history, and no radiotherapy are associated with an increased risk of secondary malignancy development. Survival times between patients with and without secondary malignancy didn't differ significantly. It's also important to note that both synchronous and metachronous cases were included in our study. Interestingly, the study group had better clinical outcomes than the control group. The findings may be a result of a conscious and meticulous approach taken by patients with multiple malignancies and their clinicians. Therefore, early screening, follow-up, and a multidisciplinary approach should be considered in managing these patients from the moment of initial diagnosis. Further studies are needed to validate our findings and provide a more comprehensive understanding of the risk factors and outcomes associated with secondary malignancies.
Figure-1A. The distrubution of secondary malignancies based on hematological malignancies.
Figure-1B. Distribution based on the types of secondary malignancies.
Clinical features of patients
Multivariate analysis result to determine risk factors for SM development
Risk factors for overall survival and relapse in patients.