A 29-year-old woman with stage IVB Hodgkin's lymphoma was treated with doxorubicin, bleomycin, vinblastine, and dacarbazine. Two weeks after the first cycle was completed, she developed pruritic, linear erythematous lesions in a flagellate-like pattern on the trunk, neck and arms. After oral prednisone therapy and cessation of bleomycin, the lesions started to recede.
Bleomycin is a cytotoxic glycopeptide, isolated from the soil fungus Streptomyces verticillus. It inhibits the incorporation of thymidine, causing DNA fragmentation. Bleomycin is used to treat several malign tumors such as Hodgkin's lymphoma (HL), squamous cell carcinoma and germ cell tumors.1
The side effects of this drug are gastrointestinal (mucositis, anorexia, and weight loss), respiratory (tachypnea, pneumonitis and pulmonary fibrosis), and dermatological (erythema, cutaneous rash, vesicles, palmary and plantar scaling, hyperpigmentation, alopecia and the less common flagellate dermatitis) as well as general symptoms such as fever and malaise.2
Here we report on a case of a 29-year-old female patient with HL, who developed the cutaneous reaction known as bleomycin-induced flagellate dermatitis during treatment.
Case reportThe 29-year-old, female patient (ETL) was diagnosed in March 2012 with HL (nodular sclerosis subtype, stage IIIB-X with all B symptoms: involvement of cervical, retroperitoneal, and supraclavicular lymph nodes; bulky mass>10cm). International prognostic score (IPS) was 1 (albumin<4g/dL). HIV, hepatitis B and hepatitis C serologies were negative. The doxorubicin (25mg/m2), bleomycin (10mg/m2), vinblastine (6mg/m2), and dacarbazine (375mg/m2) chemotherapy protocol (ABVD) was the regimen of choice followed by involved-field radiotherapy (IF-RT) of the bulky mass.
Nearly two weeks after the first cycle of ABVD, just before the second cycle, the patient started with generalized and increasing pruritus along with the appearance of several linearly arranged hyperchromic plaques in the cervical region, trunk and arms. There was a moderate response to the pruritus with the administration of prednisone (20mg/day), although established lesions remained intact.
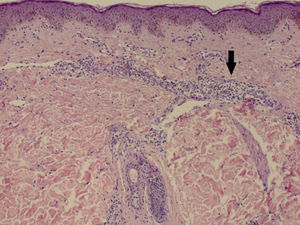
The investigation went further and a skin biopsy was performed revealing an inflammatory dermal infiltration suggesting a drug eruption compatible with bleomycin-induced flagellate dermatitis. Due to the continuation of the skin lesions with severe pruritus, bleomycin was withdrawn from the regimen on Day 1 of Cycle 4.
The patient continued to be treated with the AVD regimen up to the sixth cycle and still received prednisone (20mg/day), which was gradually reduced until suspension in September 2012 (one month after completing the sixth cycle). After the suspension of bleomycin, the skin lesions gradually subsided with complete resolution after three months. The patient was referred for IF-RT and currently has an optimal clinical state, without any evidence of lymphoma.
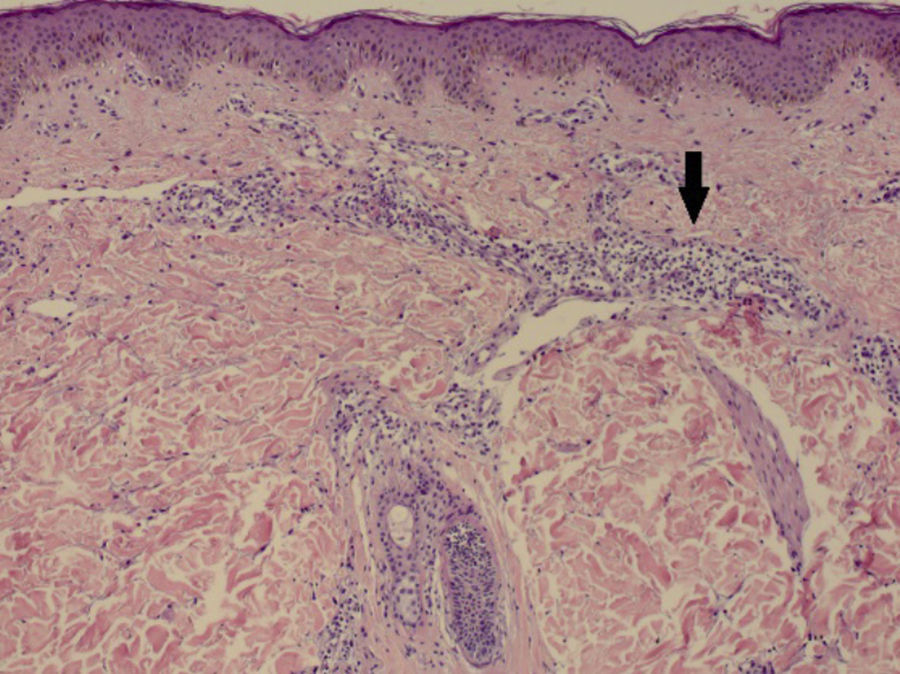
DiscussionHerein, we report on a case of bleomycin-induced flagellate dermatitis in a 29-year-old woman with HL after the introduction of the ABVD chemotherapy protocol. Although doxorubicin, vinblastine, and dacarbazine can cause erythematous or even necrotic skin lesions, the whip-like pattern associated with hyperpigmentation and severe pruritus is characteristic of bleomycin-induced flagellate dermatitis. Thus, a diagnosis of bleomycin-induced dermatitis is the most likely one. The term ‘flagellate’ derives from the Latin ‘flagellum’ referring to the characteristic whip-like appearance of the eruption. It occurs in 10% of patients treated with this drug,4 although severe and disseminated lesions are very rare. The typical skin alterations are pruritic, multiple linear lesions, initially urticarial and later with changes in pigmentation, located mainly on the thorax and back (Figure 1).3,4
First, it was believed that the occurrence of bleomycin-induced flagellate dermatitis was dose-related, but some patients developed this condition after receiving very low doses of bleomycin. The time between the administration and the onset of the clinical symptoms varies between one day and nine weeks.3
After administration, a hydrolase enzyme metabolizes bleomycin. This enzyme is almost not found in skin and lung tissues which may explain the accumulation and consequent aggression in these areas. Another pathological mechanism proposed to explain these lesions suggests that even minor trauma to the skin, for example a scratch or pressure against bone prominences, may cause increased blood flow to these areas allowing the drug to accumulate.5
There are no histopathological findings that absolutely characterize bleomycin-induced flagellate dermatitis. In this case report, the skin biopsy revealed inflammatory dermal infiltration with eosinophil predominance consistent with several other drug eruptions (Figure 2), therefore correlation with clinical findings is needed. The findings in the acute phase include vacuolization in the basal layers of the epidermis, melanin incontinence, and scattered dyskeratotic keratinocytes. In later stages, merely a few post-inflammatory changes can be found. Histological and ultra-structural studies suggest that bleomycin reduces the epidermal turnover, resulting in prolonged contact between melanocytes and keratinocytes.3,6
The decision to withdraw the drug from therapy seems to be consensus in the literature among different authors, however, the management of the symptoms varies in accordance with the experience of each service. Generally, therapy with corticosteroids or antihistamines has been beneficial, decreasing pruritus and limiting trauma to the skin.4,6 The eruptions are usually self-limiting and recede after 6–8 months yet they can reoccur or worsen after further exposure to bleomycin.3,6 In this case report, the eruptions lasted for approximately five months.
Conflicts of interestThe authors declare no conflicts of interest.
We deeply thank Dr. Milivia Enokihra from the Dermatology Department of the Federal University of São Paulo (UNIFESP) for the skin biopsy.