To assess the impact of the implementation of neonatal screening on hospitalization and death rates due to sickle cell disease in patients from the state of Maranhão, Brazil.
MethodsA descriptive study was performed of all inpatients and deaths of patients with a diagnosis of sickle cell disease in Maranhão between 1999 and 2012. Data were collected from the Hospital Information System of the Brazilian National Health Service (SUS) and the Death Information System of the Ministry of Health. The implementation of newborn screening tests in Maranhão took place in 2005, and so the periods 1999–2005 (pre) and 2006–2012 (post) were analyzed for trend analysis using a multiple linear regression model. Fisher's exact test was used for the analysis of categorical variables and the Kruskal–Wallis test for continuous variables.
ResultsThe rate of hospitalization increased from 0.315 (pre) to 1.832 (post), indicating 5.82 times more admissions (p-value=0.04). The mortality rate increased from 0.115 to 0.216, that is 1.88 times higher, but this was not statistically significant (p-value=0.586). The median age at admission dropped from 11.4 years to 8.7 years (p-value=0.0002), whereas the median age at death increased from 10 years to 14 years (p-value=0.665).
ConclusionThe increases in the rates of hospitalization and death after the implementation of neonatal screening suggests that previously there was an underdiagnosis of sickle cell disease and that screening, along with other factors, increased “visibility” in the state of Maranhão.
Hemoglobin (Hb) S originated in Africa where the mutation in the beta-globin gene was advantageous insomuch as heterozygotes have more resistance against malaria.1 In Brazil, sickle cell disease (SCD), the most prevalent hereditary disease, affects the black population most. It is estimated that about 45% of the Brazilian population and 72% of the population of the state of Maranhão is of African descendancy. Moreover, in Brazil there are 25–30,000 SCD patients with 3500 new cases diagnosed annually.2 In Maranhão there is an incidence of 72 cases per 100,000 live births (1:1389) for SCD with one carrier of the sickle cell trait in every 30 births.2
In recent years, in countries like the USA, there has been a significant improvement in the survival of SCD patients. In 1973, the estimated mean age at death of SCD patients in the USA was 14.3 years, with 50% of deaths occurring during the first five years of life.3 In 1992, a study in the USA showed that the mean age at death had increased to 42 years for men and to 48 years for women. In this study, the pattern of mortality varied with age and there was a peak incidence of death among SCD children occurring between one and three years of age; deaths of under 20-year-old patients were predominantly due to pneumococcal sepsis.4
Measures such as neonatal screening, the use of prophylactic penicillin between three months and five years of age, vaccination for pneumococcus, meningococcus and Haemophilus, and training in respect to early recognition of splenic sequestration, reduced the mortality rate to less than 5% in the first five years of life.5 The authors concluded that these measures resulted in, on average, over 85% of affected children surviving beyond the age of 20.5
In Brazil, research on hemoglobinopathies, in particular sickle cell anemia, occurred after the government Ordinance No. 822 came into force on June 6, 2001; this law was designed to improve early diagnosis and to provide adequate treatment within the first few months of life. In December 2002, a test to diagnose hemoglobinopathies was implanted in the state of Maranhão.6 The test was performed by the Association of Parents and Friends of Exceptional Children (APAE) in the city of São Luís, and by 2005 it was applied to 72% of all live births in the state.6
The objective of the current study was to compare trends in the mortality and hospital admission rates of SCD patients in Maranhão before and after the implementation of the neonatal screening test.
MethodsData related to the deaths and hospitalizations of SCD patients in Maranhão from 1999 to 2012 were collected. Data related to the hospitalizations were obtained from an abbreviated version of the Hospital Information System (SIH) of the Brazilian National Health Service (SUS) annual database and data related to deaths were obtained from the Death Information System (SIM/SUS). The cases were selected using the 10th revision of the International Classification of Diseases (ICD-10) codes for SCD: D57.0 (SCD with crisis), D57.1 (SCD without crisis), D57.2 (double heterozygous sickle cell disorders) and D57.8 (other sickle cell disorders). Two age groups were determined: 0–19 years and 20 years or more. The period 1999–2005 was considered the pre-screening test implementation period and 2006–2012 was considered the post-implementation period. Although the test officially started in Maranhão in December 2002, it actually achieved true coverage from 2005 onwards. The rates of hospitalization and mortality due to SCD were calculated per 100,000 inhabitants. The total population served as the denominator because in Maranhão Black people make up 74% of the population and this methodology has already been reported in the literature and will allow comparisons between the results of this study and others.7,8 The annual population data were obtained from the Brazilian Institute of Geography and Statistics (2000, 2010 and population estimates) and the total population of Maranhão grew from 5,418,354 to 6,714,314 between 1999 and 2012.
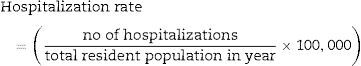
The rates of hospitalization and mortality due to SCD were calculated according to the following formula:
Fisher's exact test was used to compare the percentage distribution of individuals by gender and age between the two periods. The non-parametric Kruskal–Wallis test was used to compare the median age between the periods.
To analyze the trend, a model of the evolution of the results in the initial period was created using multiple regression to check linear and quadratic models, with and without exponential growth, and the model that best fit the data was used. After analyzing the trends, R2 values, and the results of the adjustments of regression analysis, a simple linear trend model was used to analyze the mortality and hospitalization rates. Extrapolation was subsequently performed for the first period, which would be the ‘natural’ trend. The effect of the ‘natural’ trend was then removed (detrended) for both periods and the means of the two periods were compared using the t-test for two groups. A value of significance of 0.05, which corresponds to a confidence level of 95%, was assumed for statistical analysis.
ResultsHospitalization ratesTotals of 128 and 840 SCD patients were hospitalized in the pre-test (before 2005) and post-test periods, respectively.
The median ages by year at admission ranged from eight to 35 years old. When the results of the two periods were compared, the median fell from 11.4 years in the pre-test period to 8.7 years in the post-test period (p-value=0.0002 – Kruskal–Wallis).
The percentage of males was slightly higher than that of females; 53.9% in the pre-test period and 51.9% in the post-test period.
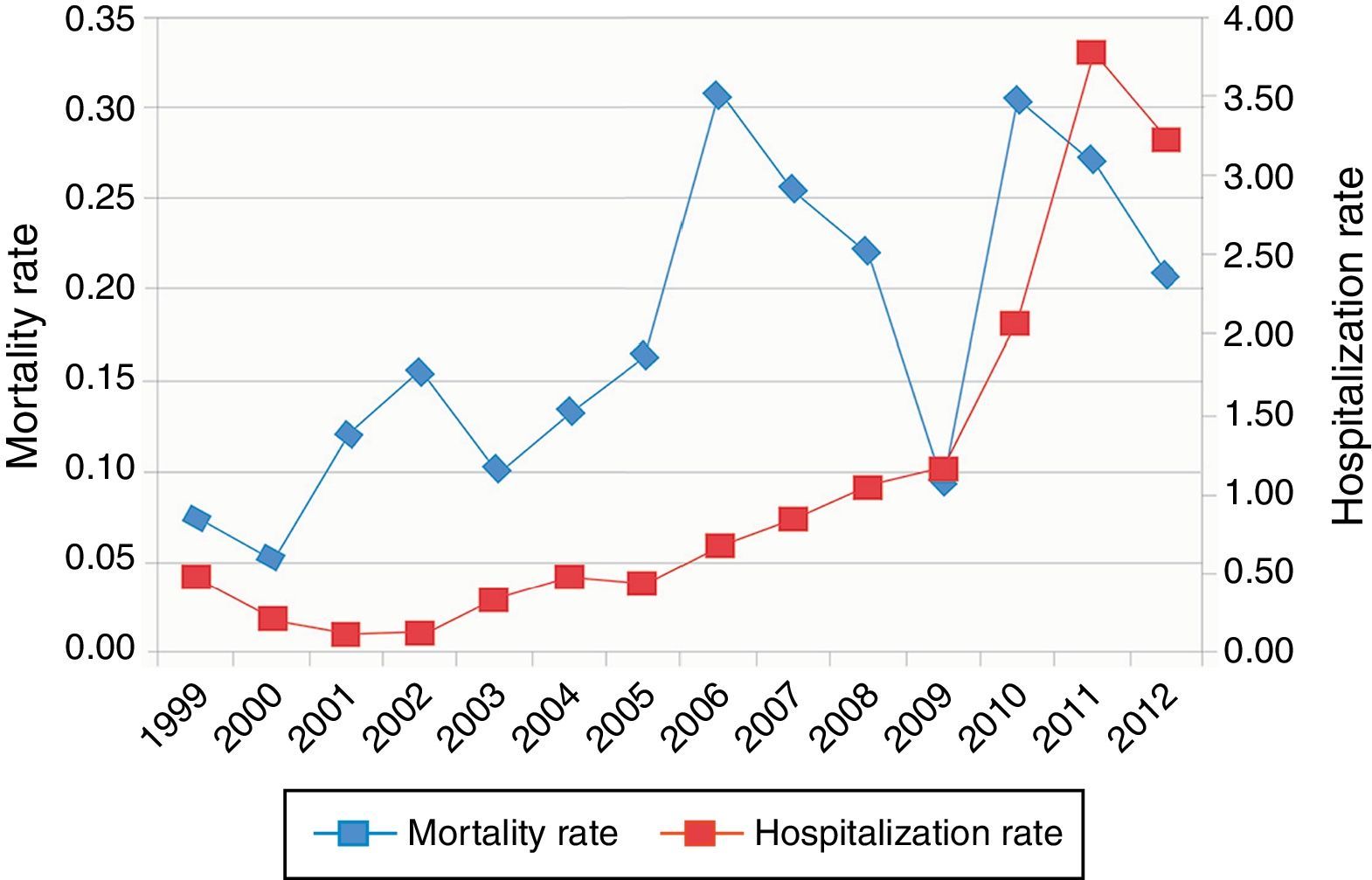
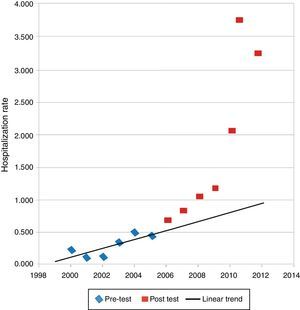
Figure 1 shows that in the pre-test period there were much fewer hospitalizations, with a marked upward trend in the post-test period. The mean hospitalization rate increased 5.82-fold from 0.315 in the pre-test period to 1.832 in the post-test period. The t-test was used to check if the mean hospitalization rate of the new period was different to the old considering detrended data, i.e. considering the ‘natural’ trend where a change in the mean would indicate a change in the trend; a descriptive level of 0.040 was obtained, from which it was concluded that the trend in the hospitalization rate changed significantly.
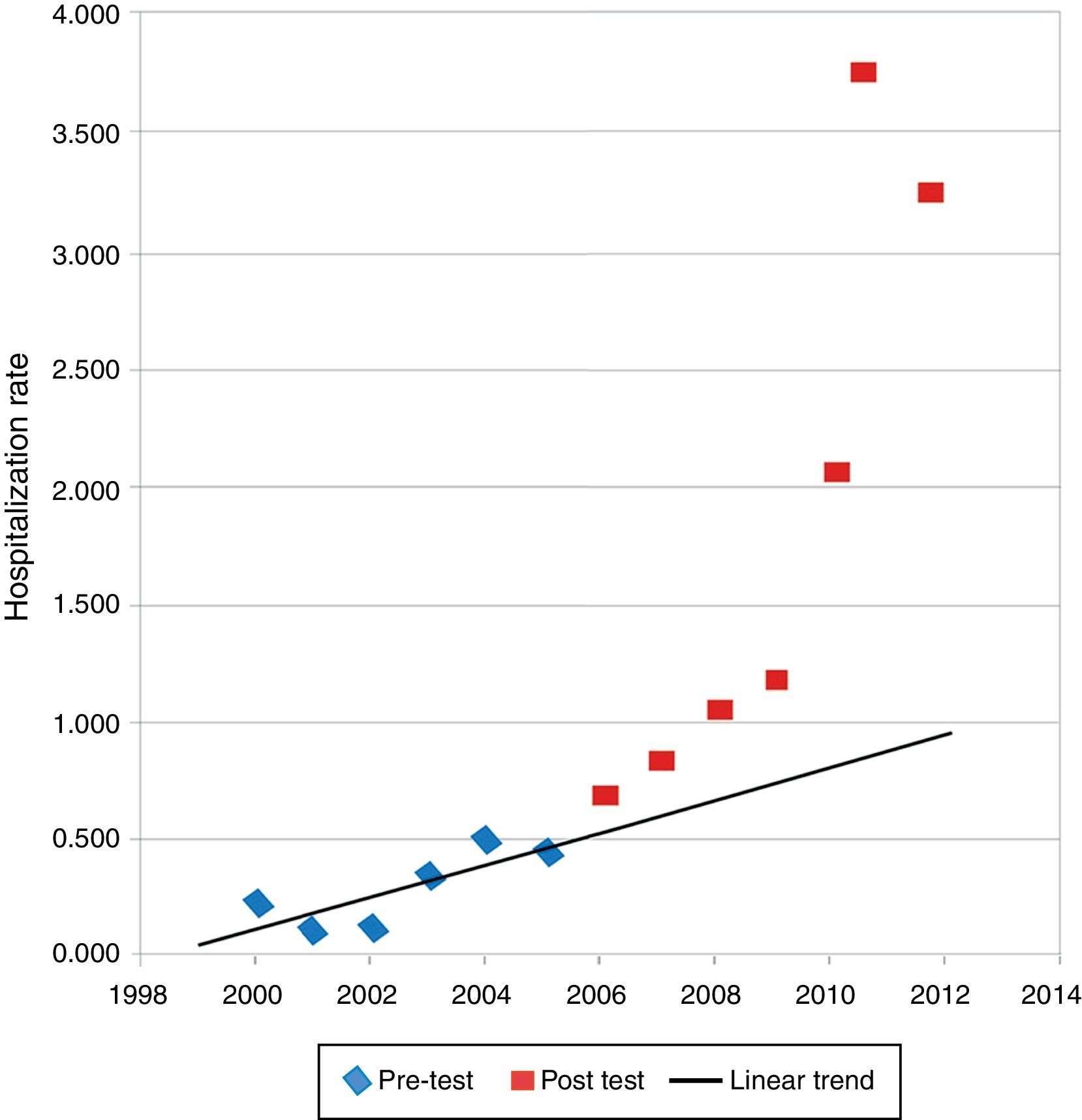
Figure 2 shows the final model for the hospitalization rate in the period 1999–2005. The majority of points from 2006 onwards are above the line, indicating that there was a change, an increase in the rate of hospitalization.
Mortality rateForty-seven patients died in the pre-test period and 107 died in the post-test period. The median ages at death by year ranged from six to 26 years. When the results between the two periods were compared it was noted that the medians were higher in the post-test period, with the median increasing from 10 years old in the pre-test period to 16 years in the post-test period (p-value=0.247 – Kruskal–Wallis).
Figure 1 shows the trend in deaths over the years; there was already an increasing trend in the pre-test period and this trend continued in the post-test period, but with greater variability. The mean mortality rate increased by 1.88 times from 0.115 in the pre-test period to 0.216 in the post-test period. Detrended data were used to check whether the mean in the post-test period was different from that of the pre-test period using the same procedure as the hospitalization rates. The t-test of both groups gave a descriptive level of 0.586, from which it was concluded that the trend in hospitalizations did not change significantly.
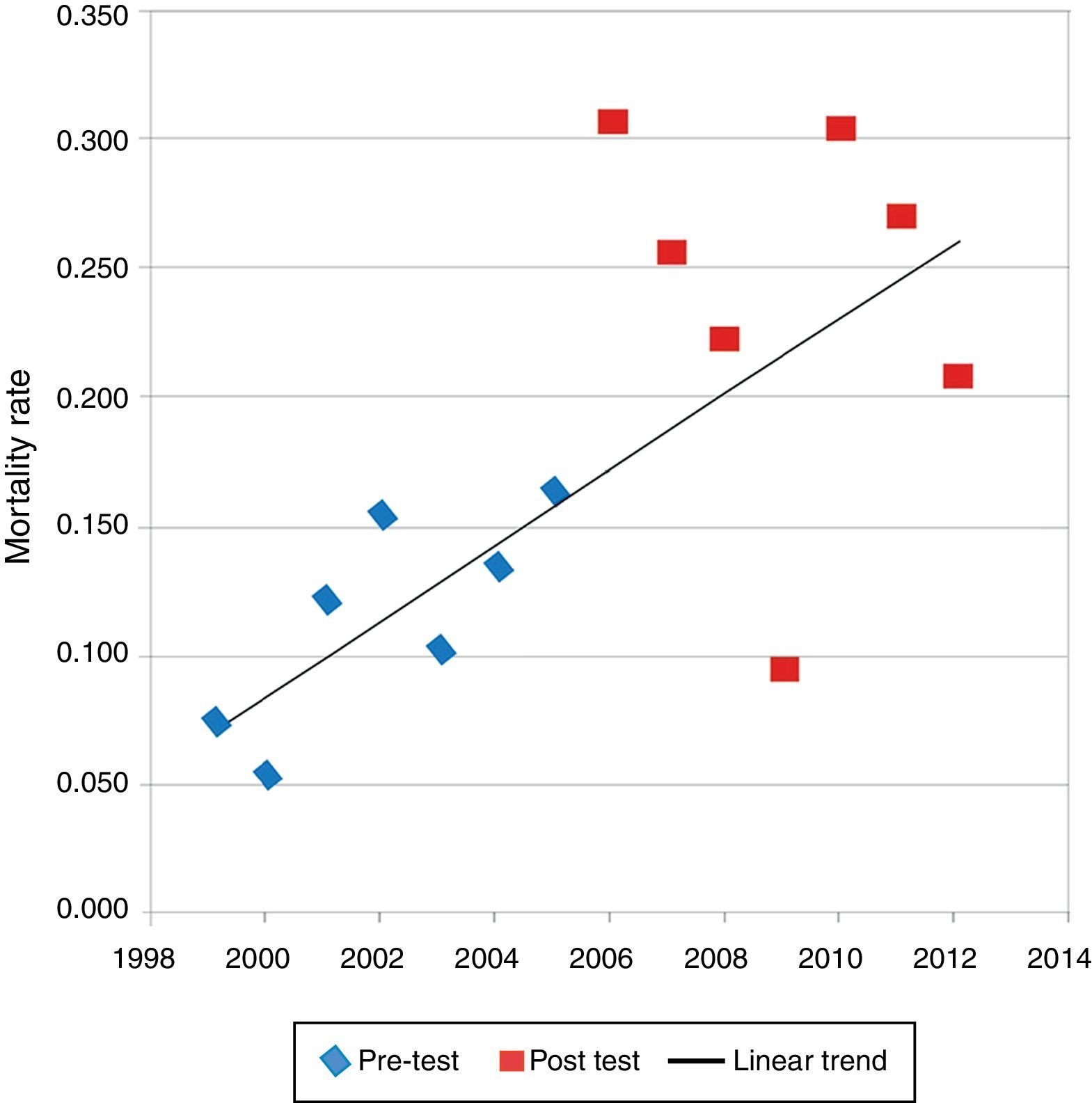
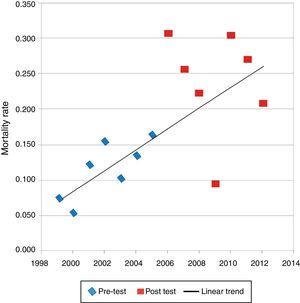
Figure 3 shows the final model for the mortality rate. If the death rate had continued at the same level, the values for future years would have been close to the extrapolated line. If there had been a significant change in the mortality rate due to the screening test, the majority of the points from 2006 onwards would be above the line. In this graph, it can be seen that from 2006 onwards some points are above the line, others are around the line, and some are below.
DiscussionIn the present study, the mean hospitalization rate increased significantly from 0.315 in the period prior to the implementation of the neonatal screening test to 1,832 in the post-test period. One of the hypotheses for this increase is the better reporting of cases requiring hospital care. One of the causes of under-reporting is the difficulty of making a diagnosis. This problem was reduced with the implementation of the neonatal screening program, which probably facilitated the early diagnosis of SCD children, thereby raising the number of hospital admissions. Other causes of under-reporting could include poor hospital care, the incorrect use of ICD codes, and the lack of hospital registration with no consequent recording in the SIH/SUS system of cases which remained emergencies throughout the period of hospital treatment.
Despite progress, the hospitalization rate in Maranhão is still far below the national average. A Brazilian study,7 based on data from the SIH/SUS for 2002, reported hospitalization rates for SCD of 1.8 in the state of Bahia, and 6.0 and 7.0 for the states of São Paulo and Rio de Janeiro, respectively. These states have the following percentages of black population: Bahia: 78.8%; Maranhão: 74.3%; São Paulo: 45.3% and Rio de Janeiro: 30.9%.9
Given that the overall prevalence of SCD in the black population is 0.22%,9 the expected number of cases in 2002 would have been 11,339 in Bahia, 9486 in Maranhão, 10,191 in Rio de Janeiro, and 10,918 in São Paulo. In other words, the expected number of cases in the four states would be very similar, and thus the hospitalization rates should have been very similar. However, the actual hospitalization rates are much higher in Rio de Janeiro and São Paulo. Currently, the rate of hospitalization in Maranhão is 1,832, similar to the state of Bahia, but about 3–4 times less than the states of São Paulo and Rio de Janeiro in that study.7
It is possible that the low hospitalization rates in Maranhão occur not only due to under-reporting of patients who required hospital treatment, but also due to the low level of hospital care for patients with SCD in the state. Under-reporting of patients was reduced after the implementation of the neonatal screening test. This analysis infers that the hospitalization rates for SCD are a reflection of the quality of medical care provided to patients and the social differences that exist between Brazilian regions.
After the implementation of the neonatal screening test in Maranhão there was a significant reduction in the median age of hospitalized SCD patients, from 11.4 years in the pre-test period to 8.7 years in the post-test period. This shows the initial impact of the test on the youngest age groups. The data reflect the national reality as the 2002 Brazilian study7 reported that hospitalizations were generally of younger patients, with most being under the age of 29 years, and around 70% under 19 years. The median ages were 11 years in Bahia, and 12 years in Rio de Janeiro and São Paulo.
Confirming a reduction in the under-registration of deaths attributed to SCD caused by a lack of diagnosis, the present study noted that there was an increase, albeit insignificant, in the mean mortality rate of almost 200% from the pre-test period to the post-test period. It is believed that there was no statistical significance for this increase due to the great variability in the post-test period (in 2009, in particular, and in 2012 there were decreases) and that the number of deaths in each group was small.
The median age at death was very low (ten years in the pre-test period and 14 in the post-test period) with no significant difference between the two periods. At the national level, the median age at death is about twice that in Maranhão. In 2002, the median age at death for SCD patients was 26.5 years in Bahia; 31.5 in Rio de Janeiro and 30.0 in São Paulo.7 The current situation in Maranhão is comparable to that of Brazil in 1996, when the median reported age at death was 18.5 years.10
SCD patients live much longer in some other countries. The aforementioned US cohort study reported that the median age at death was 42 years for men and 48 for women. For patients with Hb SS it was 60, and for patients with the Hb SC genotype it was 68.4 Another cohort study performed in Jamaica reported a median age at death of 53 years for men and 58.5 years for women with Hb SS.11 The mean age at death in SCD patients seems not to have changed since studies conducted by Platt et al. in the early 1990s because a recent study examining the age at death using death certificate data from the US National Center for Health Statistics showed that in the US in 2005, considering all the genotypes, the median age at death of SCD patients was 42 years for women and 38 years for men.8 Perhaps this particular study had an inherent bias because if patients with SCD live longer it is less likely that their death certificate will include sickle cell disease as the cause.
In the current study, it was not expected that there would be a change in the age at death, but only in the absolute number of recorded deaths due to improved notification. In a future analysis, in some decades, when patients diagnosed by screening reach adulthood, it may be possible to observe an increase in the median age at death in Maranhão.
The present study has shown that the implementation of a neonatal screening test for hemoglobinopathies has not yet resulted in an increase in the survival of patients with SCD in Maranhão, when one considers the low age at death and the marked difference between the ages at death compared to elsewhere in Brazil, and internationally.
Prompt diagnosis of the disease on its own is not enough to have a positive impact on patient survival. This has been observed in two Brazilian cohort studies related to neonatal screening (one in the state of Minas Gerais and the other in the state of Rio de Janeiro) where it was observed that even with a carefully controlled program, the probability of children with Hb SS dying was still considered to be high, with 71.8% of deaths occurring in under two-year-old children.12 Infections and splenic sequestration13 were the main causes of death, and 23% of deaths occurred outside the hospital environment.12 It is clear that in addition to a neonatal screening test for hemoglobinopathies it is necessary to optimize other measures, such as family counseling about the serious complications of the disease, effective vaccination and drug distribution programs, as well as access to effective medical care to treat clinical complications. On the other hand, the socioeconomic characteristics of the population also influence the survival of SCD patients and, according to some researchers,14 the presentation and severity of the disease depend on socioeconomic status, nutrition, preventive measures and access to health services. These are all relevant issues in Maranhão, which has one of the worst human development indexes (HDI=0.639) in Brazil; the state was in the second from bottom position overall of Brazilian states in 2010.15
Despite the fact that the SIH/SUS encompasses the majority of hospital admissions in Brazil, a limitation of the present study is the validity of information provided by the SIH/SUS. It is possible that not all the health facilities in the state of Maranhão that care for SCD patients systematically register their admissions in the SIH/SUS system. This leads to an under-estimation of the frequency of hospitalizations. Failure to properly complete ICD information may well be another limitation in accurately checking the occurrence of hospitalizations for SCD.
The under-reporting of deaths is a problem in the state of Maranhão. However, the situation has improved in recent years, when the notification of deaths increased from 48.8% in 2001 to 70% in 2011. Nevertheless, this is much lower than in states in the south and southeast of Brazil, where the figure has been close to 100% since 1991.16 Another limiting factor is the quality of information.
It is concluded that the key reason for the apparent paradox of increased mortality and hospitalization rates after the implementation of neonatal screening is the increased ‘visibility’ of SCD, which is primarily due to physicians, who are responsible for filling out death certificates and diagnostic data required to authorize hospital admittance.
Conflicts of interestThe authors declare no conflicts of interest.