CD20 expression was reported at different rates in patients with multiple myeloma. The importance of this B-cell antigen for plasma cells is still unknown. This study aimed to investigate CD20 expression of myeloma cells in bone marrow, and any relationship between the stage of disease, isotype and clinical features.
MethodsSixty-one patients who were admitted to the hematology clinic of the Adnan Menderes Medical School with the diagnosis of multiple myeloma according to the criteria of the “International Myeloma Working Group” were enrolled in this study. Age, gender, Durie–Salmon stage, history of autologous hematopoietic stem cell transplantation, and the distribution pattern and positivity of CD20 expression on multiple myeloma cells in bone marrow were evaluated. The Mann–Whitney U and chi-square tests were used for statistical analysis with a p-value<0.05 being accepted as statistically significant.
ResultsThirty patients (48.9%) had positive scores for CD20 with the distribution pattern being most likely interstitial in 55.6% of the cases. There was no statistically significant difference between immunohistochemical positivity for CD20 expression on multiple myeloma cells, immunoglobulin type, and the stage of disease.
ConclusionThe combination of immunohistochemical studies with flow cytometry may reveal the importance of CD20 positivity in patients with multiple myeloma more clearly.
Multiple myeloma (MM) is a clonal B-cell malignancy characterized by the accumulation of mature plasma cells in the bone marrow and other tissues. The myeloid or other B-cell markers such as CD10, CD19, CD20 and CD22 may be related to the prognosis of patients with MM.1 According to studies, CD20 expression may be related to a poor prognosis, however the prognostic significance in patients with MM needs further investigation.1 CD20 is a phosphoprotein, which plays a role in B-cell development. There are few studies about immunohistochemical evaluations of CD20 expression on myeloma cells in MM.2–4 Robillard et al.2 reported 12 (18%) of 66 patients with CD20 expression. The expression of CD20 by myeloma cells is heterogeneous, and can be detected only in 13–22% of patients.3 The same study reported that disease stabilization is seen in 50–57% of CD20+ patients over a period of 10–27 months.3 Mateo et al.5 reported CD20 expression in 17% of all MM cases with most of them having only CD20+ plasma cells. In recent years, studies have focused on surface antigens due to the importance of targeted therapies. The role of anti-CD20 therapy for MM has yet to be clearly established.4 This study aimed to investigate CD20 expression on myeloma cells in bone marrow and any relationship between the stage of disease, isotype and clinical features.
MethodsSixty-one patients (31 male, 30 female, mean age 64±11 years) with MM were enrolled in this study. The distribution pattern and positivity of CD20 expression on myeloma cells in bone marrow, age, gender, Durie–Salmon stage and the history of autologous hematopoietic stem cell transplantation were evaluated. Clinical characteristics and CD20 expression were evaluated at the time of diagnosis. Immunohistochemical staining of CD38, CD138, Kappa/Lambda were applied to lysine coated slides. CD20 expression was determined by immunohistochemical staining of bone marrow biopsies. Immunohistochemical analysis was performed by the avidin–biotin complex method. B lymphocytes were evaluated comparing immunohistochemical analysis of CD20 with hematoxylin–eosin stain. The patients were evaluated for CD20 positivity using a cut-off value of 10%. We could not compare immunohistochemistry with flow cytometry to detect CD20 in myeloma cells. Statistical analysis (Mann–Whitney U and chi-square tests) was performed using the Statistical Package for the Social Sciences and a p-value <0.05 was accepted as statistically significant.
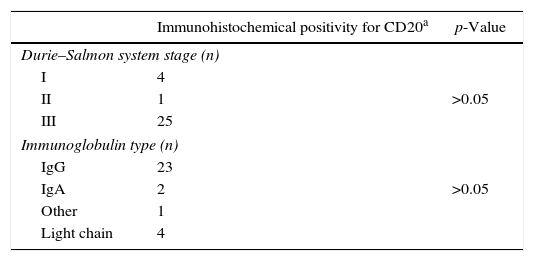
ResultsThe immunoglobulin type was IgG heavy chain for 38 (62.3%) patients with no patients having IgM myeloma. Forty-three patients (70.5%) were stage 3 according to the Durie–Salmon staging system and 11 patients had medical histories of autologous hematopoietic stem cell transplantation. Thirty patients (49.2%) had positive scores for CD20 with the distribution pattern being most likely interstitial in 55.6%. Although the cut-off value for CD20 positivity was 10%, CD20 expression was detected in 28.7% of all cases using a cut-off value of 20%. The clustered pattern of CD20 positive myeloma cells is shown in Figure 1. The characteristic features of patients with multiple myeloma are shown in Table 1. There was no statistically significant difference between immunohistochemical positivity for CD20 of myeloma cells, immunoglobulin type, and the stage of disease (p-value>0.05) (Table 2).
Characteristic features of patients with multiple myeloma (n=61).
| Variable | |
|---|---|
| Gender (M/F) | 30/31 |
| Mean age (years) | 64±11 |
| Durie–Salmon system stage (n) | |
| I | 14 |
| II | 4 |
| III | 43 |
| Immunoglobulin type (n) | |
| IgG | 38 |
| IgA | 9 |
| Other | 6 |
| Light chain | 8 |
| CD20 positivitya(n) | 30 |
Association between immunohistochemical positivity for CD20 of myeloma cells and immunoglobulin type and the stage of disease.
| Immunohistochemical positivity for CD20a | p-Value | |
|---|---|---|
| Durie–Salmon system stage (n) | ||
| I | 4 | |
| II | 1 | >0.05 |
| III | 25 | |
| Immunoglobulin type (n) | ||
| IgG | 23 | |
| IgA | 2 | >0.05 |
| Other | 1 | |
| Light chain | 4 | |
Different stages of differentiation of the neoplastic clone may cause heterogeneity in MM. Cell surface antigens may be helpful to determine the antigenic phenotype. Similar results have been reported for the heterogeneity of antigenic expression of plasma cells using two techniques (immunofluorescence and immunohistochemistry) with the results drawing attention to the antigenic heterogeneity.6 The antigen expression of myeloma cells is heterogeneous, and immunophenotype impacts on clinical outcome in MM.7
CD20 is a transmembrane phosphoprotein that acts as a calcium ion channel in the cell membrane, and plays a role in B lymphocyte activation and its differentiation to plasma cells. The importance of this B-cell antigen for plasma cells is still unknown.8
Flow cytometry is an easy and commonly used method to determine cell surface antigens. A panel including CD20 is recommended by the International Consensus Group to determine plasma cell immunophenotype.9 The European Myeloma Network recommends a minimal panel including CD19, and CD56 but prefers a panel that includes CD20, CD117, CD28, CD27 to detect abnormal plasma cells.10 Robillard et al.2 reported CD20 expression in 12 of 66 patients with MM. CD10, CD20 and HLA-DR were weakly positive in less than one-third of patients in a study consisting of 112 untreated MM patients.6 Ngo et al.7 evaluated 107 MM patients and reported the clinical impact of immunohistochemical markers in bone marrow biopsy samples with 32% of them being positive for CD20. Loss of CD20 expression during the disease course correlates with significant worsening both of overall survival and event-free survival compared to the time of diagnosis.7 Grigoriadis et al.11 analyzed newly diagnosed plasma cell myeloma with an aim of identifying clinicopathological features of CD20 in this disease and found that CD20+ plasma cells are not a unique subset in myeloma. CD20 positivity was reported in 17% of all multiple myeloma patients.5 In the current study, 48.9% of the patients had positive scores for CD20 with a cut-off value of 10% and 28.7% of the patients with a cut-off value of 20%.
Cell morphology may be associated with CD20 positivity. Histological type of plasma cells and prognosis were evaluated in 674 patients with MM. A significant relationship was reported between CD20 phenotype and mature cells, more importantly with small plasma cells (lymphoplasmacytic).12 Both morphologies are characterized by low-grade malignancy. A correlation has also been reported between small mature plasma cells, CD20 and t(11.14) in patients with MM.2 In addition, there were statistically significant differences in the expression of CD20 between plasma cell leukemia and MM with CD20 displaying higher reactivity in plasma cell leukemia8; none of the patients in the current study had the latter disease.
The CD20 antigen is a suitable target in the treatment of lymphoma patients, but the use of monoclonal antibodies to treat MM is still controversial. The differences between these two malignancies are the heterogeneity and the weak expression of CD20 on plasma cells. Thus, CD20 positive MM and Non-Hodgkin's lymphoma with plasmacytoid differentiation should be treated as separate entities.
The patients in this study had a M-protein peak in the gamma zone by serum protein electrophoresis. There was no splenomegaly or organomegaly. Some studies have reported that about half the plasma cells have a morphologically lymphoplasmacytic appearance. Immunohistochemical studies may be helpful in these cases. Cytoplasmic immunoglobulin is usually positive, but not CD20 on plasma cells.13 The association between CD20 expression and small mature plasma cell morphology was reported in the study of Robillard et al.2 The significance of CD20 expression in MM patients is not well understood yet.
The CD20 antigen is associated with shorter survival, and may be a poor prognostic factor for MM.4,6,14 According to Grigoriadis et al.,11 CD20+ plasma cell myeloma cases represent a heterogeneous disease and not a unique clinicopathological entity. However, the prognostic significance of CD20 expression in MM alone is unclear. The effect of other markers of the disease is not known clearly.4,6
CD20+ MM cells occurred in three patterns in the study by Quinn et al.4; the patterns were reported as follows: diffuse (63%), interstitial (33%), and clustered (4%). The relationship between pattern, isotype in bone marrow and CD20 positivity has been reported in the literature.4 According to this study, 24 cases were positive for CD20, 62.5% with IgG heavy chain and ten cases with lambda light chain. In the current study 38 (62.2%) patients had IgG heavy chain MM but no patients had IgM myeloma. Moreover there was a higher positivity for CD20 expression compared to the literature; according to the cut-off value of 20%, 28.7% of the patients were positive.
The limitations of this study were the small number of cases and the use of only one methodology, immunohistochemical analysis, to evaluate CD20 expression. The prognostic significance of CD20 positivity might be better evaluated by combining flow cytometry and immunohistochemical analysis in larger cohorts.
Conflicts of interestThe authors declare no conflicts of interest.