Polycythaemia vera patients can present with arterial or venous vascular occlusive events such as thrombosis or cardiovascular disease; disease-related symptoms may significantly impact on the quality of life. The aim of this study was to evaluate the efficacy and safety of erythrocytapheresis compared to phlebotomy in the treatment of polycythaemia patients.
MethodsThis study reports the findings of a retrospective analysis of 40 polycythaemia vera patients diagnosed according to published guidelines and treated either with erythrocytapheresis or phlebotomy over a four-year period. The goal of treatment was to reduce blood volume and red blood cell count to near normal levels as both of which may attenuate the symptoms and complications associated with polycythaemia. Patients were treated by applying a mathematical model.
ResultsUsing the model, 28 erythrocytapheresis procedures were performed. Blood laboratory values (red blood cell count, haemoglobin count and haematocrit level) were significantly reduced in patients treated with erythrocytapheresis. Moreover, among treated patients, erythrocytapheresis resulted in less work absenteeism and reduced costs due to lost production, with a lower overall procedure cost in comparison to phlebotomy.
ConclusionThis model can assist in selecting the proper treatment modality for individual patients. Especially for those with high blood volumes and high achievable haematocrit levels (delta), erythrocytapheresis offers a more efficient method in red blood cell depletion compared to phlebotomy thereby, potentially reducing the number of treatment procedures required for the induction of polycythaemia vera patients as well as the interval between procedures during the maintenance phase.
Polycythaemia vera (PV) manifests at a median age of 60 years. Patients can present with arterial or venous vascular occlusive events such as thrombosis or cardiovascular disease. Disease-related PV symptoms, such as microvascular disorders, pruritus (which may be excruciating), migraine-type headache and fatigue, may significantly impact on the quality of life.6 However, patients occasionally can present with haemorrhages or may be asymptomatic at presentation. Mortality is chiefly related to thromboembolic events with the principal aim of therapy being to reduce the risk. Thus the goals of treatment are to reduce complications and improve survival. The target for Haematocrit (Hct) control in PV was originally based on data from assessments of numbers of vascular events for different Hct levels. It was estimated that a target below 0.45 should be maintained.6 This target has now been validated in a randomised clinical trial by cytoreductive therapy in PV with investigators assessing the impact of stringent Hct reduction to <0–45 compared to a more liberal target range of 0.45–0.50.6 Patients with a Hct target of < 0.45 had significantly lower rates of cardiovascular death and major thrombosis than those with a target of 0.45–0.50.6
Randomised trial data supports that venesection of 200–500 mL blood at intervals, depending on patient size and tolerability, should be used to achieve and maintain a Hct of < 0.45.1 Regular venesection requirements have been reported to be associated with higher thrombosis risk, especially in patients requiring three or more venesections per year. When frequent venesection is needed to achieve this target, an alternative approach may need to be considered. The Italian Societies of hematology and Blood Transfusion recently issued recommendations for phlebotomy in PV to obtain a target haematocrit <45%. Selective red blood cell (RBC) apheresis (erythrocytapheresis - ECP) is recommended as an alternative to phlebotomy only when a rapid attainment of the target haematocrit level is needed, such as in the occurrence of severe vascular complications, or before emergency surgery.1
ECP is an extracorporeal blood separation method whereby whole blood is extracted from a donor or patient, the red blood cells are separated, and the remaining blood is returned to the circulation. The use of ECP as a therapeutic option has advantages over traditional methods.5 It has been suggested that 4–5 exsanguinations would be necessary to match the effectiveness of a single cycle of ECP. Moreover, ECP could therefore have clinical and economic benefits. In order to obtain better results in the daily practice, optimizing ECP and selecting the proper treatment modality for individual patients could be advantageous.
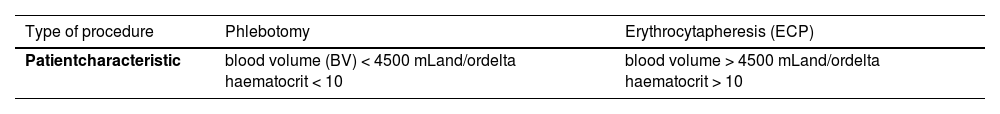
Materials and methodsThis study reports the findings of a retrospective analysis of 40 patients with PV. Patients were diagnosed according to published guidelines and treated with ECP or phlebotomy over a four-year period. Patient baseline demographics and clinical characteristics were similar between treatment groups. Age, gender, polycythaemia, and most clinical symptoms were not significantly different between treatment modalities. ECP procedures were carried out using a continuous flow automatic centrifugal 16-gauge cell separator accessed in two cubital veins of the forearm. The instrument has software that is based on the required apheresis volume needed to achieve the required Hct level. The efficiency of ECP was compared to phlebotomy by determining the volume of RBCs that were extracted by ECP and by phlebotomy as related to the patient's blood volume (BV) and to the delta haematocrit, the latter being the difference in Hct before and after the ECP procedure. BV values were estimated using the Nadler method. The goal of treatment was to reduce blood volume, RBC count, haemoglobin count and HCT level to near normal levels, as these may attenuate the symptoms and complications associated with polycythaemia. To optimize the proper treatment modality, we treated patients applying the model presented in Table 1 adapted for the individual patient.
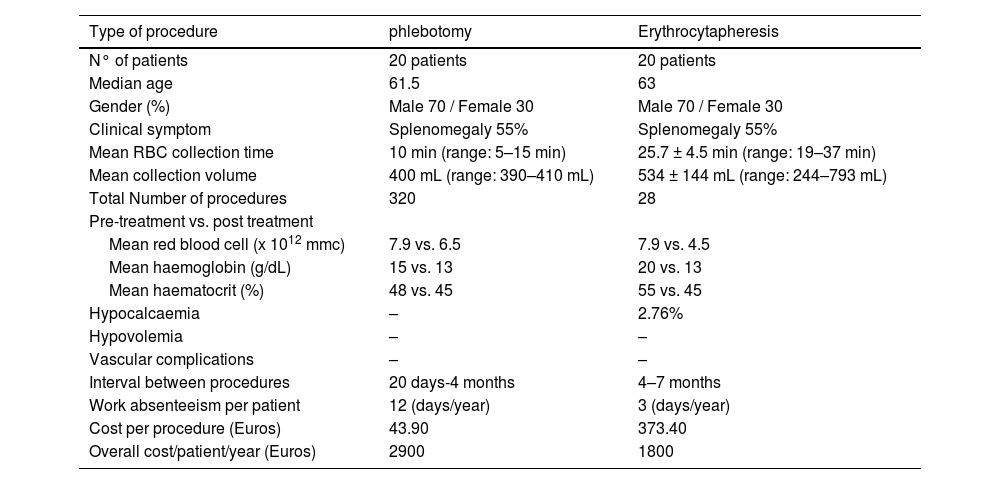
ResultsUsing the model described above a total of 28 ECP procedures were performed with the mean RBC collection time being 25.7 ± 4.5 min (range: 19–37 min) and the mean collection volume being 773.5 ± 129.3 mL (range: 600–100 mL). Blood laboratory values, RBC count, haemoglobin count and HCT level were significantly reduced in patients treated with ECP (pre-treatment vs. post treatment - Table 2). After ECP, symptoms associated with polycythaemia, such as discoloured/purple face and palms, mucosal congestion, fatigue, dizziness and headache, were relieved immediately and dramatically. Hypocalcaemia was identified in 2.76% of treated patients and was associated with numbness around the mouth, fingers and toes. For prevention, all patients received oral or IV administration of 10% calcium gluconate solution (20 mL) before ECP. No patients developed symptoms of hypovolemia. The interval between procedures is reported to be longer after ECP: 20 days-4 months after phlebotomy and 4–7 months after ECP. ECP is more expensive than phlebotomy, either due to the higher cost of devices or because of indirect costs owing to the longer time employed by specialized personnel; the difference in the total costs is only partially mitigated by the longer interval for ECP. However, among treated patients, ECP results in the less work absenteeism and reduced lost production costs, with an overall procedure cost lower in comparison to phlebotomy.
Characteristics of the patients submitted to phlebotomy and erythrocytapheresis between 2018 and 2021.
The current retrospective analysis demonstrates that ECP treatment significantly reduced the mean number of RBCs, mean haemoglobin and mean Hct in patients with polycythaemia. The symptoms related to hyperviscosity were dramatically improved after ECP. The RBC count was generally reduced together with a reduced loss of white blood cells and platelets. The time required for ECP was under 30 min and was associated with few adverse side effects. Overall, ECP was considered to be a safe procedure. This mathematical model can assist in selecting the proper treatment modality for individual patients, especially for those with high BVs and high achievable Hct (delta). ECP offers a more efficient method of RBC depletion compared to phlebotomy and thus potentially reduces the number of treatment procedures required in the induction of PV patients as well as the interval between procedures during the maintenance phase.
It has been demonstrated that ECP is associated with cost savings resulting from a lower number of treatment procedures and lower productivity loss for ECP-treated patients.2-5
Rombout-Sestrienkova et al. reported that the total number of procedures needed and the duration of each were reduced by approximately 70% in patients treated with ECP vs. phlebotomy.7 The total cost per ECP procedure is 373.40 Euros, which includes the indwelling needle, special catheter and corresponding drugs. Comparatively, phlebotomy costs approximately 43.90 Euros which includes costs associated with blood collection. Although the per procedure costs were higher using ECP, the total costs for ECP treatment were comparable or less expensive than phlebotomy.
Rombout-Sestrienkova et al. recently demonstrated no significant difference in total treatment costs between ECP-treated patients compared with those treated with phlebotomy.7 However, the costs resulting from work absenteeism were significantly lower for the ECP group with an estimated cost saving of about 1000 Euros.
ECP can rapidly reduce RBC count, haemoglobin and Hct, and improve clinical symptoms. ECP in combination with pharmacotherapy may offer additional benefits. Considering the indications for ECP, including PV, hereditary polycythaemia, haemoglobin disease, and secondary polycythaemia, the therapeutic implications for ECP are widespread. In total, ECP has distinct advantages over conventional therapy and should be considered when choosing a treatment plan for patients with polycythaemia.