A reduced platelet count (PLT) is a frequent post-operative finding in orthopedic surgery patients. Despite its prevalence, the characteristics of post-surgical thrombocytopenia have not been well described.
MethodsA retrospective chart review was conducted on patients who underwent a knee or hip replacement from 2012 to 2015. Patients who received heparin were excluded.
ResultsA total of 56 patients were analyzed on post-operative days 0 to 4. By day 1, 90.9% of the patients experienced a reduction in their platelet counts. The lowest mean platelet count (nadir) occurred on day 2 (201.3 × 109/L). The average decrease in the platelet count from the baseline was 24% (95%CI: 20.6 - 27.2). The change in the platelet count from the baseline ranged from a 49.6% drop to a 14.2% increase. A substantial portion of patients experienced thrombocytopenia, with 28% occurring on day 2. Platelet counts less than 100 × 109/L occurred only once. The percent decrease in the platelet count from the baseline to any other time point was significantly larger in patients aged > 65 years, compared to patients aged ≤ 65 years (p = 0.007). Specifically, the average drop in the platelet count at the nadir (day 2) relative to the baseline was 27.8% in patients aged > 65 years, compared to 19.5% in patients aged ≤ 65 years.
ConclusionsA reduction in the platelet count is a frequent post-operative finding in orthopedic surgery patients, even after removing confounding factors, such as heparin exposure, but clinical thrombocytopenia is uncommon. Alternative etiologies should be considered when the platelet count is less than 100 × 109/L. Vigilance should also be considered regarding elderly patients.
Thrombocytopenia has been reported to occur after a variety of surgical procedures and has been termed “post-operative thrombocytopenia."1 Platelet (PLT) nadirs reportedly occur during the first four post-operative days. The characteristics of this phenomenon have not been well described. Hemodilution and increased platelet consumption have been proposed as mechanisms for the decreased platelet count.2,3 Due to the considerable risk of venous thromboembolism (VTE) in orthopedic surgery patients, the use of heparin and low-molecular weight heparin (LMWH) in the peri‑operative setting has become routine.4,5 This confounds the interpretation of the reported data because it raises the possibility of heparin-induced thrombocytopenia as an alternative cause. More recently, the use of the new direct oral anticoagulants (DOACs) and a renewed interest in aspirin for VTE prevention has led to a decreased exposure to heparin in this patient population.6-8 Given the increase in non-heparin or LMWH based DVT prophylaxis, post-operative platelet trends can now be evaluated in patients who have not been exposed to heparin.
We evaluated the platelet count in post-operative orthopedic surgery patients who were not exposed to heparin or LMWH. The patients in our study received DVT prophylaxis via aspirin, DOACs or sequential compression devices.
MethodsThe current study is a retrospective observational study that was approved by the Institutional Review Board of Northwell Health. We identified all the cases of patients who underwent a knee or hip replacement from 2012 to 2015 by searching our electronic medical record system. Data items collected included: age, sex, length of stay, type of surgical procedure (knee versus hip replacement) and laboratory data (complete blood count) (see Table 2). We excluded patients who were less than 18 years of age, had a pre-operative platelet count greater than 400 × 103/uL or less than 150 × 103/uL, or who were exposed to heparin peri‑operatively. All other patients who received a knee or hip replacement during the aforementioned time period were included in the study.
Statistical analysisThe analysis of the platelet count over time was accomplished by using a repeated measures linear regression model in which the change in the log (PLT) from the baseline was expressed as a function of time, potential factors (age, type of surgery and sex) and their potential pairwise interactions with time. Backward elimination was used to select model terms that were significantly associated with the outcome. A similar approach was used to analyze the white blood cell (WBC) count over time. For comparisons of change in the log (PLT) or log (WBC) counts between multiple time points, p-values were adjusted using Tukey's method for multiple comparisons. The Spearman correlation coefficient was used to assess the association between the change in the platelet count from the baseline to day 1 and the change in the WBC count between the baseline and day 1.
Unless otherwise specified, a result was considered statistically significant at the p < 0.05 level of significance. All analyses were performed using the SAS version 9.4 (SAS Institute, Cary, NC).
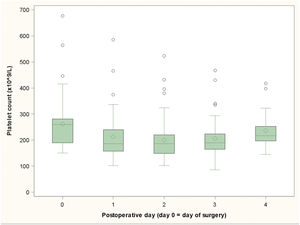
ResultsFifty-six patients were analyzed from one day pre-operatively (day 1) to the day of discharge. One patient had missing data at day 1 and was not included in the final analysis. On day 1, 50 patients experienced a reduction in their platelet counts (90.9%). After day 1, no additional patients had a drop in their platelet counts. The lowest mean platelet count (nadir) occurred at day 2 (mean = 201.3 × 109/L). In the repeated measures model of the platelet count on days 0 to 4, the mean platelet count at nadir (day 2) differed significantly from the baseline mean count (p < 0.0001), from the day 1 mean count (p = 0.03) and the day 4 mean count (p < 0.0001). The average decrease in the platelet count between the baseline and nadir was 24% (95%CI: 20.6 - 27.2). The change in the platelet count between the baseline and nadir ranged from a 49.6% drop to a 14.2% increase (since five patients had a rise in their platelet counts) (see Figure 1).
As mentioned, over ninety percent of the patients had a decline in their platelet counts from their baselines, with 28% experiencing thrombocytopenia (defined as less than 150 × 109/L), as shown in Table 1. A more severe thrombocytopenia with a platelet count of less than 100 × 109/L occurred in only one patient.
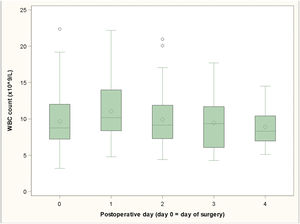
The highest mean WBC count occurred on day 1 (mean = 11.0 × 109/L), with an average increase of 16.1% (95%CI: 5.8 - 27.6) relative to the baseline. The mean WBC count significantly increased from day 0 to day 1 (p = 0.003). There was not enough evidence to conclude that the mean WBC count differed from the baseline on any other post-op day (see Figure 2).
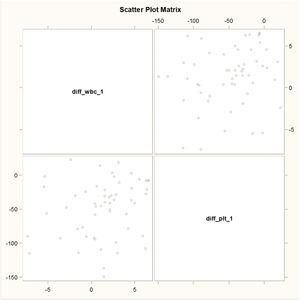
There was a significant positive relationship between the change in the WBC count from the baseline to day 1 and the change in the platelet count from the baseline to day 1 (Spearman's rho = 0.29, p = 0.03): relatively larger WBC increases were associated with relatively smaller platelet count drops and relatively smaller WBC increases were associated with relatively greater platelet count drops (see Figure 3).
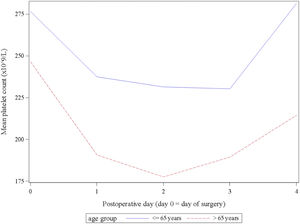
We analyzed the association between the platelet count and other collected data. The percent decrease in the platelet count from the baseline to any other time point (day 1 to day 4) was significantly larger in patients aged > 65 years, compared to patients aged ≤ 65 years (p = 0.007). Specifically, the average drop in the platelet count at the nadir (day 2) relative to the baseline was 27.8% in patients aged > 65 years, compared to 19.5% in patients aged ≤ 65 years (see Figure 4).
There was no significant difference in the mean platelet count between the types of procedure (knee versus hip replacement) (p = 0.143) or between sexes (p = 0.175).
DiscussionThrombocytopenia after surgical procedures is a common impetus for hematologic consultation. The differential diagnosis for the etiology of thrombocytopenia is broad. Post-operative thrombocytopenia should be considered among these causes. However, there is little recent published data on this phenomenon. It is reported that platelet counts decline approximately 30% to 70% after major surgery.9-13 This was proposed to be due to hemodilution, as well as increased platelet consumption related to the effects of surgery, which helps to explain why the post-surgery platelet count usually continues to decline over the next 1 to 3 days, with the nadir usually occurring at a median of post-operative day 2 (range, 1 - 4).2,9
Our data demonstrate that a reduction in the platelet count occurs frequently after orthopedic surgery in a non-heparinized population. This drop was seen in the majority of patients (90.9%) with the nadir occurring on day 2, as previously published.2,9 However, only 28% of the patients were actually thrombocytopenic. In addition, five patients had an increase in their platelet counts by day 1 without any significant drop below the baseline thereafter. There was no significant association with regards to age, sex, or type of surgery to explain this rise in the platelet count.
This study also demonstrated a previously unrecognized relationship with age. There was a significant difference in platelet count reductions in patients > 65 years, compared to those ≤ 65 years (24.8 × 109/L), suggesting that advanced age increases the risk of thrombocytopenia, requiring closer monitoring.
The etiology for the decreased platelet count has not been elucidated. Bone marrow suppression is an unlikely explanation, as there was no concordant decrease in the WBC count. The rise in the WBC count suggests a stress response that should have been reflected in a secondary thrombocytosis.10,12-14 This discrepancy is unexplained. Interestingly, it was found that relatively larger WBC increases were associated with relatively smaller platelet count drops and relatively smaller WBC increases were associated with relatively greater platelet count drops, suggesting that the post-operative stress response may mitigate the trend toward thrombocytopenia.
Lastly, although 28% of the patients experienced thrombocytopenia by day 2, the nadir remained > 100 × 109 and only one patient had a platelet count below that level. Therefore, alternative causes of thrombocytopenia (infection, medication-induced, immune-related, etc.) should be considered in patients who experience severe thrombocytopenia post-operatively (defined as a platelet nadir < 100 × 109), as this was a rare finding in our study. Additional studies will be needed to confirm our findings in other surgical populations.
ConclusionThe reduction in the platelet count is a frequent post-operative finding in orthopedic surgery patients, even after removing confounding factors, such as heparin exposure, but clinical thrombocytopenia is uncommon. Nadirs typically occur by day 2. Alternative etiologies should be considered when the platelet count is < 100 × 109/L. Vigilance should also be considered in regard to elderly patients, as age > 65 was associated with a more significant drop in the post-operative platelet count.