Nasopharyngeal carcinoma is an Epstein Barr virus (EBV) driven malignancy. It is uncommonly seen in young adults in the 15-25 years age group. Its annual incidence in Asian countries is more compared to its Western counterparts.1 Nasopharyngeal carcinoma rarely comes to medical attention before it has spread to regional lymph nodes. Enlargement and extension of the tumour in the nasopharynx may result in symptoms of nasal obstruction, changes in hearing and cranial nerve palsies, though the most common physical findings are neck mass consisting of painless, firm lymph node enlargement. The most common nodes involved are the jugulodigastric and upper and middle jugular nodes in the anterior cervical chain. According to the World Health Organization(WHO), nasopharyngeal carcinoma is classified into three subtypes namely, keratinizing squamous cell carcinoma, nonkeratinizing squamous cell carcinoma and undifferentiated or poorly differentiated carcinoma including lymphoepithelioma and anaplastic variant.2 Nasopharyngeal carcinoma is positive for pan-cytokeratin, EMA and EBV-LMP and usually positive for markers of squamous differentiation like p40 and p63.
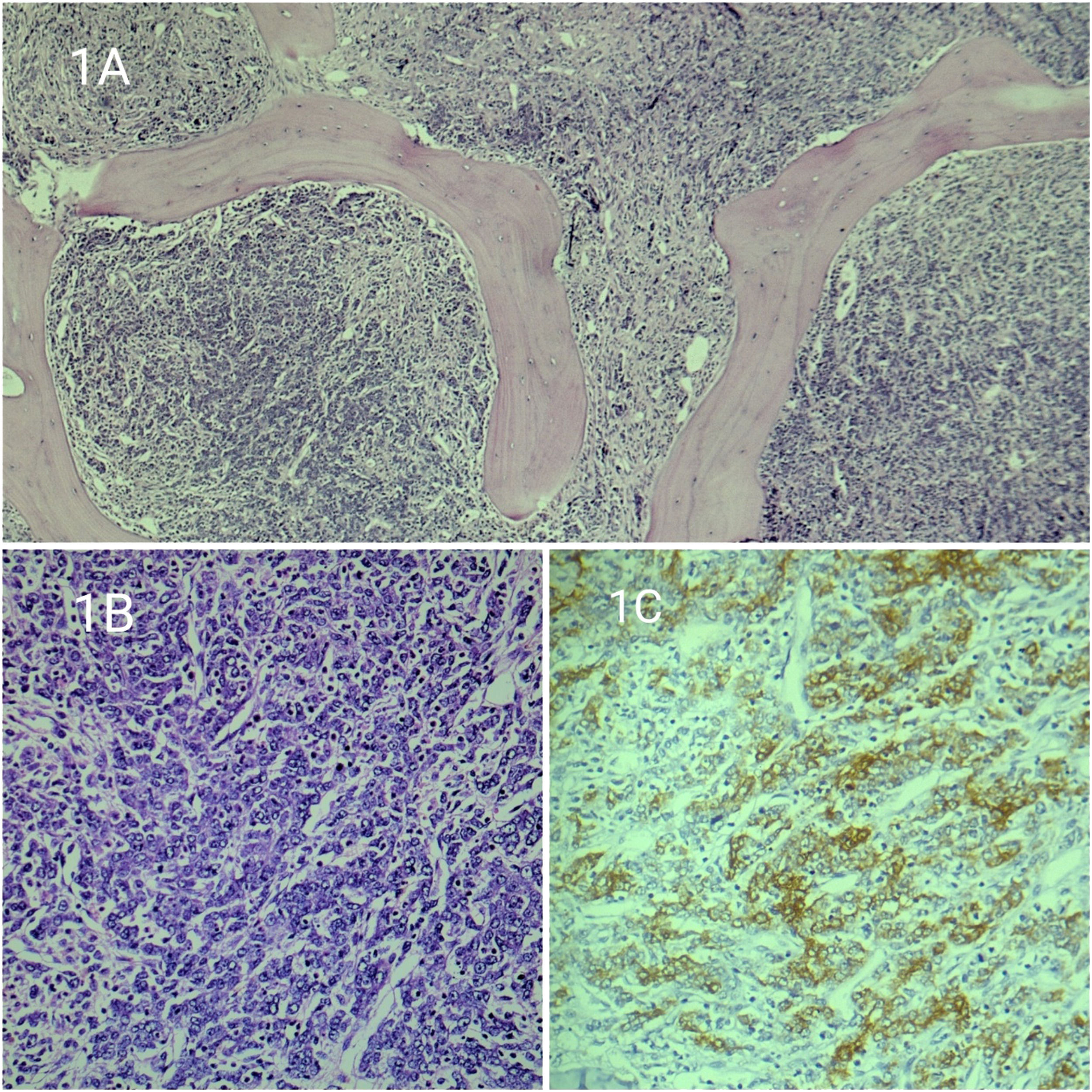
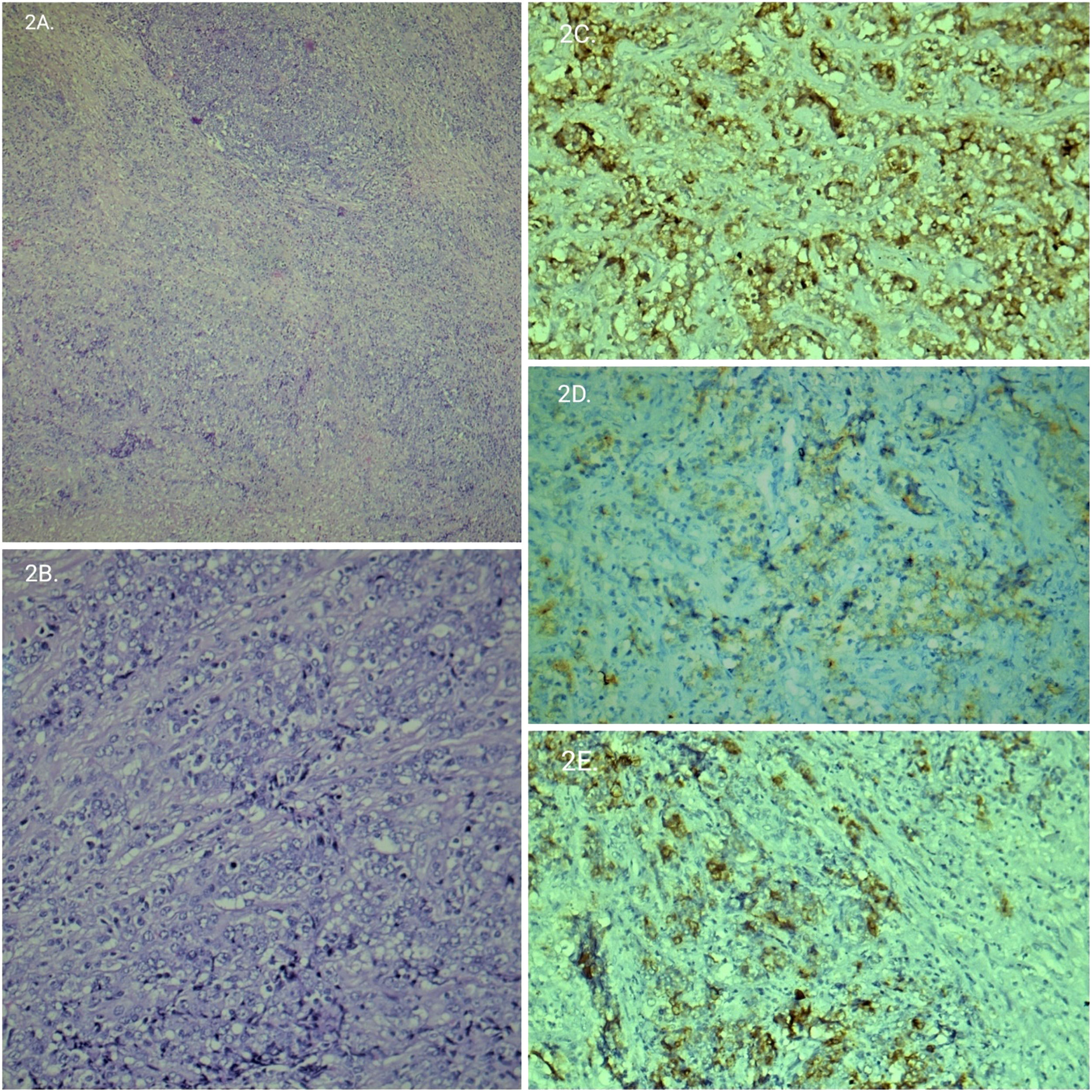
CaseA 22-year-old male presented with fever, generalised lymphadenopathy, left knee swelling and left pleural effusion for 4 months. Clinical examination revealed generalised lymphadenopathy and hepatosplenomegaly. Peripheral blood examination showed microcytic hypochromic anaemia, neutrophilic leucocytosis with left shift (Total leucocyte count:42,670/ cu.mm, differential count: myelocytes:05, metamyelocytes:02, neutrophils:85, lymphocytes:03, monocytes:05) and mildly reduced platelets (80,000/cu.mm). CT thorax and abdomen showed mediastinal, abdominal, axillary and cervical lymphadenopathy, bilateral pleural deposits, anterior chest wall lesion, hepatosplenomegaly and multiple deposits in the liver, spleen and bilateral kidneys. Sclerotic bony metastasis in manubrium sterni, thoracic and lumbar vertebrae were identified. Imaging findings were suggestive of disseminated lymphoma and clinical differential diagnosis were lymphoma, metastatic carcinoma and metastatic germ cell tumour. Excisional cervical lymph-node biopsy, bone marrow aspiration and trephine biopsy were performed. Bone marrow imprint smear showed infiltration by large atypical cells with focal clustering and a possibility of lymphoma infiltration was considered in correlation with clinical and radiological findings. Bone marrow trephine biopsy showed focal clusters, nests and scattered individual tumour cells with moderate cytoplasm, pleomorphic nuclei, vesicular chromatin and prominent nucleoli in a densely fibrotic marrow. There was no sinusoidal pattern of involvement. Morphologically, the differential diagnosis (DD) considered were metastatic carcinoma and anaplastic large cell lymphoma. On immunohistochemistry (IHC), these tumour cells were positive for pan-Cytokeratin, negative for Leucocyte common antigen (LCA) and CD30. So, the final diagnosis was given as bone marrow involvement by metastatic carcinoma. Cervical lymph node biopsy showed completely effaced lymph node architecture with nests of large atypical cells having similar cytological features as on trephine biopsy along with brisk mitotic figures and prominent desmoplastic reaction. On the further extended panel of IHC markers, these tumour cells were positive for epithelial membrane antigen (EMA), Epstein Barr virus latent membrane protein (EBV-LMP) and negative for CD2, CD20, ALK, p40, CD117, synaptophysin and chromogranin (Figures 1 and 2). CD117 and EMA were done to rule out clinical DD of metastatic germ cell tumours. The other metastatic epithelial malignancies which are negative for p40 and p63 include sinonasal undifferentiated carcinoma which usually presents with mass lesion and malignancy in older individuals and is not associated with EBV. Another close DD is midline NUT carcinoma which was initially described in children and almost always shows abrupt squamous differentiation and is positive for p40 and p63 and not associated with EBV. Negativity for neural markers and absence of typical dot like cytokeratin positivity ruled out neuroendocrine differentiation. The final diagnosis was a metastasis from nasopharyngeal carcinoma undifferentiated type due to absence of mass lesion and no detectable primary lesion and EBV-LMP positivity.
A: Low power image of a lymph node shows diffuse effacement of the lymph node architecture with nest of tumour cells with desmoplastic reaction. Figure 2B: Tumour cells showing similar morphology as bone marrow. Figure 2C, 2D, 2E: Tumour cells are positive for EMA, EBV-LMP, and Pan-Cytokeratin respectively.
Almost 85% of nasopharyngeal carcinoma presents with cervical lymph nodes metastases from an occult primary and almost 25% have bilateral lymph nodes.3 The nasopharynx may have a normal appearance or may show fullness and surface granularity or an overt mass on radiological examination. In a patient with a normal appearing nasopharynx, random biopsies produce diagnostic tissue in about 70% of cases whereas the others may require a re-biopsy.4 Nasopharyngeal carcinoma predominantly occurs in the 40–60 year age group, though it can be seen in children.2 The association between EBV infection and undifferentiated nasopharyngeal carcinoma is well documented5 and EBV genomic RNA has been repeatedly demonstrated in malignant cells. Morphological characteristics of the undifferentiated type consist of uniform cells with ovoid vesicular nuclei, prominent nucleoli, and indistinct cell borders arranged in a syncytial pattern. There are two morphologic patterns seen. In Regaud's pattern, the neoplastic cells form well-defined, cohesive cell nests and cords separated by lymphocytes and plasma cells. In Schmincke's pattern, the inflammatory component permeates the cell nests and is impossible to distinguish from lymphoma on morphology. IHC markers are of immense help to distinguish undifferentiated carcinoma from lymphoma. So, an initial panel of markers should include Pan-Cytokeratin and LCA. If pan-cytokeratin comes positive, then next panel should be markers of squamous differentiation like p40 and P63. EBV-LMP can be used in tumours which are negative for p40, and p63. Like in this case, EBV-LMP turned out to be very useful in the undifferentiated type of nasopharyngeal carcinoma, which is found to be p40 negative. CD117, PLAP can be useful, if there is clinical and/or morphological suspicion of germ cell tumour. Synaptophysin and chromogranin help to rule out tumours with neuroendocrine differentiation.
ConclusionNasopharyngeal carcinoma without any typical symptoms and presenting as generalised lymphadenopathy with multiorgan metastasis can mimic lymphoma clinically and radiologically, as seen in this case. So the differential diagnosis of metastasis should always be kept in mind and Pan-Cytokeratin should be done to rule out the same. This case also highlights the importance of using correct IHC panel of markers to arrive at the final diagnosis.