Intravascular large B-cell lymphoma is a rare, peculiar extra-nodal variant of Non-Hodgkin's lymphoma (NHL), considered a sub-type of diffuse large B-cell lymphoma (DLBCL), as classified by the World Health Organization. It is defined as a proliferation of mature B cells (and rarely T cells), confined within the lumen of small–medium vessels.1 Plegger and Tappeiner described IVL in 1959 as ‘Angioendotheliomatosis proliferans systemista’ reflecting their opinion that IVL arose from the endothelial cells. With the advent of Immunohistochemistry (IHC) and molecular studies, the lymphoid origin of the neoplastic cells in IVL was established.2 Since then, more than 100 cases of IVL have been reported most of them involving the Central Nervous System (CNS) and skin.3
Fever of unknown origin (FUO) is defined by Petersdorf as “a fever of 38.3°C or more lasting for at least three weeks for which no cause can be identified after three or more out- patient visits. One of the reasons for FUO is lymphomas, primarily in form of atypical clinical manifestations, like in absence of lymphadenopathies and/or splenomegaly.4 Central nervous system (CNS) and skin involvement are most common; however, it is virtually present in other viscera. Lymphadenopathy and organomegaly are very rare.5
It is difficult to diagnose IVLBCL because of the rarity of diagnosis, non-specific symptoms and absence of radiologically characteristic features as many of the cases present in advanced stage and with atypical presentation and are diagnosed mostly in autopsy.6 However, most recently imaging techniques, such as fluorodeoxyglucose (FDG) Positron Emission Tomography (PET-CT) fusion images can render a simple and rapid clue to the diagnosis. Bone marrow involvement is rarely reported in IVLBCL, but whenever present usually presents with cytopenias. We herein describe a case of primary bone marrow IVLBCL in a 69 years old male patient who presented with FUO. Bone marrow biopsy was done as indicated for FUO and involvement by IVLBCL was suggested and further confirmed by Immunohistochemistry (IHC) studies.
Case reportA 69-year-old man was admitted to the hospital with a history of fever for the past 1 month with no other systemic complaints. No focal symptoms or organomegaly were observed. No relevant family history was obtained.
On investigation, Complete blood count (CBC) revealed slightly high Normal White blood cells (WBC) with monocytosis (12.90%), Absolute neutrophil count (ANC): 7310/ul and mild anemia (9.6 g/dl) LDH was elevated 6330 U/L, increased serum fibrinogen level (639 mg/dl) and raised C-reactive protein. The peripheral blood smear showed occasional nucleated red blood cells, monocytosis, and adequate platelet counts with no abnormal cells.
Bone marrow aspiration and biopsy were indicated for fever of unknown origin.
Bone marrow aspirate was done and showed hypercellularity with predominant (46%) atypical plasmacytoid cells scattered singly with binucleated, multinucleated forms and bizarre morphology, some of them were having vacuolated cytoplasm. A diagnosis of poorly differentiated malignancy was suggested on aspirate. Myeloma workup and PET-CT were also advised.
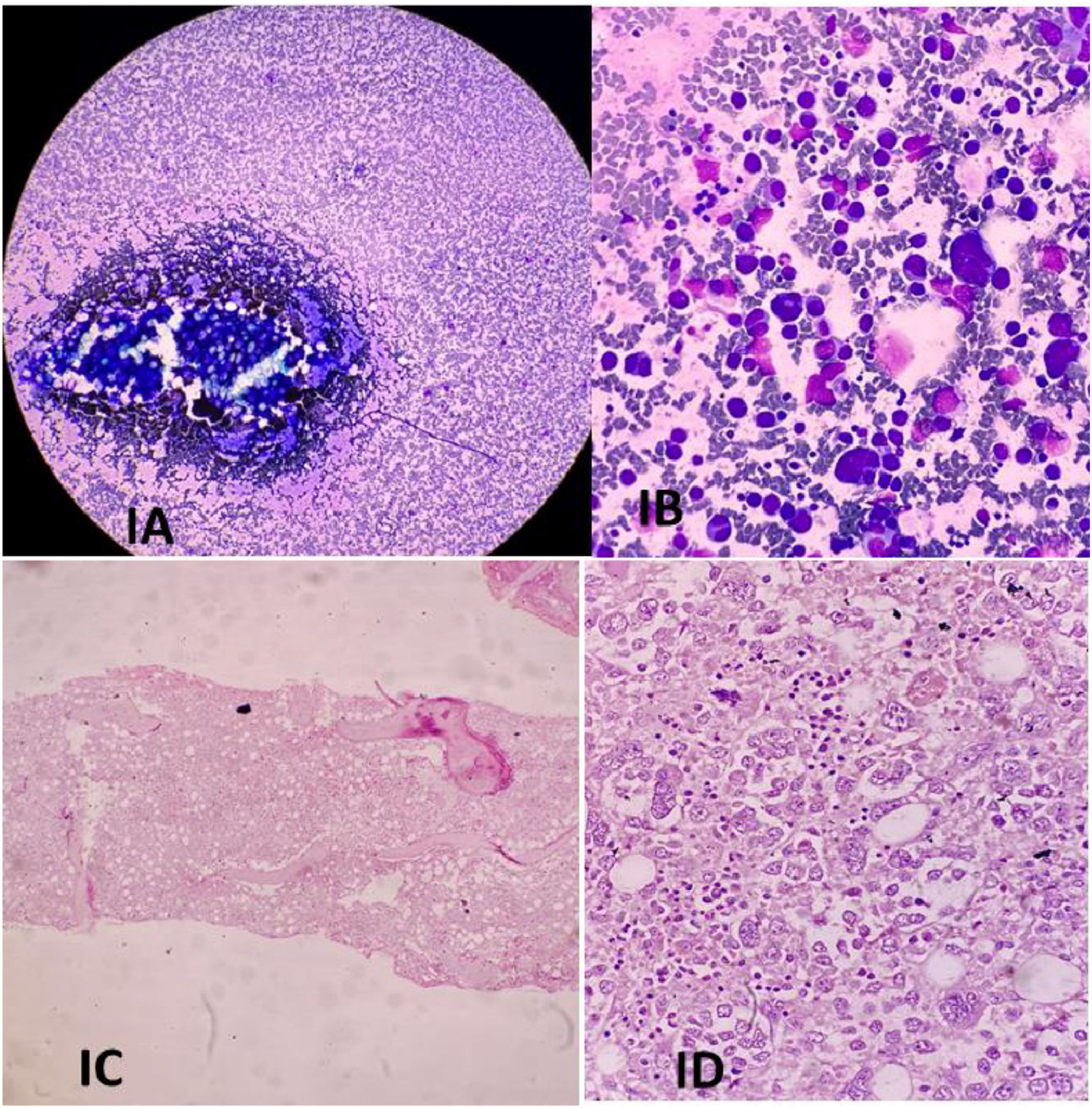
PET-CT scan showed increased uptake in bone marrow, liver, and spleen, however, no focal lesions were seen. Subsequent histological examination of bone marrow biopsy revealed hypercellularity, with extensive infiltration by neoplastic cells predominantly involving the sinusoids. Tumour cells were large and almost filled the dilated sinuses (discohesive pattern), showing nucleomegaly, vesicular chromatin, 1-2 prominent nucleoli, and a moderate amount of basophilic cytoplasm. Some of the tumour cells were very large, with multi-lobated nuclei, and some binucleated cells were seen(Figure 1). Morphological differentials considered were Metastatic malignancy, Non-Hodgkin Lymphoma, and Plasma cell myeloma.
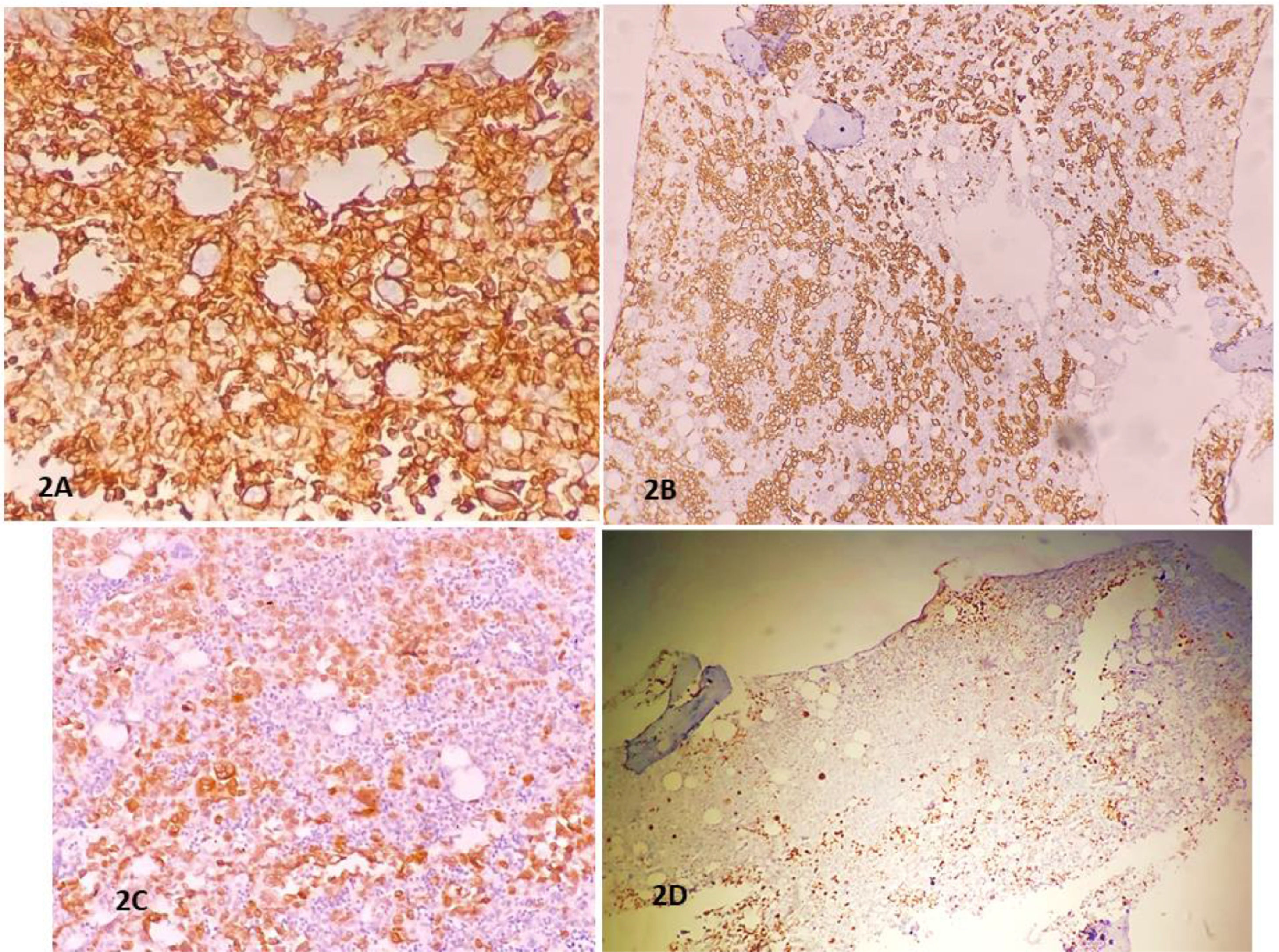
A primary panel of Immunohistochemistry (IHC) was applied, tumor cells were immunoreactive for Leukocyte common antigen (LCA), and not immunoreactive with Cytokeratin (CK), Placental like alkaline phosphatase (PLAP), Human melanoma black (HMB-45), Cluster differentiation (CD) CD30, CD34, CD138.
A secondary panel of IHC showed immunoreactivity of tumour cells for CD79a, CD20, MUM1 (>30%) and no immunoreactivity for CD10, CD5, BCL-6. Ki index was 50-60% in tumour cells (Figure 2) With collective investigation and findings, finally, a diagnosis of IVBCL with primary involvement of bone marrow was confirmed.
DiscussionIVLBL is a very rare Non-Hodgkin lymphoma. The age at presentation ranges from 39 to 88 years with a median age of 61 years.7 The reported case is 69 years old male. Murase et al. studied 96 cases of IVLBCL and found that the incidence of IVLBCL was equal in males and females.8
The most common site of involvement in 96 cases discussed by Murase et al was bone marrow in 54 cases followed by the liver in 14 cases, spleen in 13 cases, skin in 6 cases, and lung in 5 cases, and lymph nodes in 3 cases.8 In the reported case the primary site of involvement was bone marrow.
The most common presentation of IVLBCL comprises fever (90%) along with cytopenias (90%) and confusion (up to 50%). Hemophagocytic lymphohistiocytosis (HLH) is a rare presentation for patients with IVLBCL that can be potentially life-threatening. This presentation is characterized by fever, cytopenia, hepatosplenomegaly, hemophagocytosis, hypertriglyceridemia, hyper-ferritinemia, elevated soluble CD25, and low Natural killer cell activity.7]The reported case presented with nonspecific fever of unknown origin with monocytosis. However, it did not meet the criteria for HLH. In a Japanese study, Hepato-splenomegaly and bone marrow involvement were 77% and 75%, respectively.8 Liver, spleen, and bone marrow involvement was discussed in a Korean study and were 70%, 75%, and 50%, respectively.9
The immunohistochemistry in the case series reported by Murase et al. showed that CD5 was immunoreactive in tumour cells in up to 36 of 96 patients (38%). They also discussed that there were no significant differences in the immunophenotypic features between the CD5 not reactive and CD5 reactive groups. Epstein-Barr virus has not been seen to be associated in any case.8 The reported case was not immunoreactive for CD5.
The possible reason for the poor prognosis of IVLBCL as suggested by most of the studies is, its late diagnosis followed by its aggressive nature. The reported case was diagnosed within 1 month of presentation as bone marrow examination was done fairly early. Some studies suggested that early diagnosis and prompt treatment with Rituximab improve prognosis.7 Kato et al. studied and showed up to 100% response rates in patients treated with R-CHOP (Rituximab, Cyclophosphamide, Hydroxydaunorubicin hydrochloride, Oncovin, and Prednisone) followed by autologous hematopoietic stem cell transplant.10
The unique feature in our case was that the primary diagnosis of IVLBCL was made with a bone marrow examination. Our case also showed the importance of bone marrow examination in patients of PUO as it may help us reach the diagnosis of rare and occult lymphomas at an earlier stage, which could improve the overall prognosis of these patients.
In conclusion, fever of unknown origin with cytopenia should be evaluated by bone marrow aspiration and biopsy. FDG-PET could also be helpful to detect non-nodal lymphomas like IVLBCL and to rule out secondary marrow involvement by a nodal lymphoma. An early diagnosis of this lymphoma may contribute to a better prognosis as these clinically occult lymphomas involve bone marrow quite commonly.
Ethical standardsThis study is based on data compilation and analysis of routine diagnostic reported patient data. No direct patient interaction or additional sampling was needed.