Lymphoblastic lymphoma (LBL) is a neoplasm of precursor lymphoid cells and term is used to describe predominantly lymph node–based disease; however, because LBL and acute lymphoblastic leukemia (ALL) are known to represent the same disease entity, the World Health Organization (WHO) classification has unified these entities as precursor B-cell and T-cell lymphoblastic leukemia/lymphoma; when the disease is restricted to primary nodal and extranodal sites with minimal involvement of bone marrow (< 20% lymphoblasts in marrow), a diagnosis of LBL is made.1
LBL form approximately 2% of all lymphomas.2 B-cell LBL, form 10 % of all LBL and is a rare type of fast-growing non-Hodgkin's lymphoma (NHL).3,4. The commonest sites of involvement reported in B-cell LBL are lymphnodes, bone and skin (in 75% of cases), with rest occurring in miscellaneous sites such as head and neck (parotid gland and Waldeyer's ring), retroperitonium, breast, ovary, brain and soft tissues.5,6 Primary presentation of epidural LBL is very rare.7,8 Epidural involvement is thought to be from the distant source through lymphatic system or direct invasion from vertebral bodies.9 Up to best of our knowledge only few cases of Primary epidural B -cell LBL are reported so far.7,8,10 In this article we describe a case of 16 year old female who presented to our surgery with long duration low back ache and paraparesis and was finally diagnosed as case of B-cell LBL.
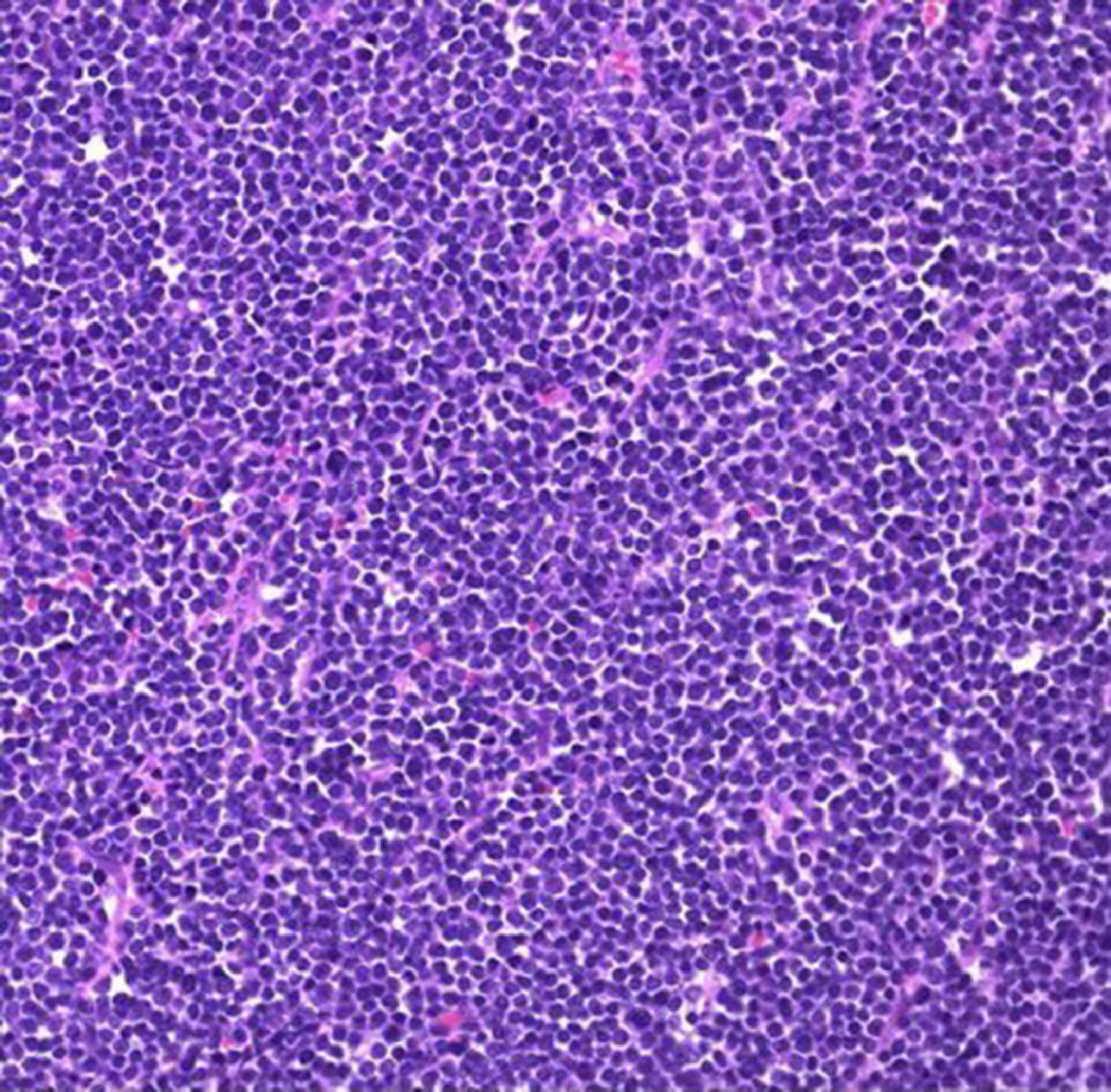
CaseTable 1 shows the timeline of the case. As shown in table -1, a 16 years old female, without any known illness presented to emergency Department of our Institution with a history of low back and both lower limb pain for 6 months, inability to walk for the last 3 weeks and loss of bowel and bladder control for the last 2 days. Patient denied history of fever, night sweats or history of injury or fall. Cranial nerve examination was unremarkable, with only slight decrease in bilateral lower limb power. There was no palpable lymphadenopathy/ hepatosplenomegaly, pallor or icterus. Her peripheral smear, ultrasound of the abdomen, X ray chest and CSF study was unremarkable. Urgent MRI of the lumbosacral spine revealed evidence of a soft tissue mass at the level of L3 vertebra, for which she underwent urgent excision with decompressive laminectomy and pedicle screw fixation. The histopathological examination revealed a small round blue cell tumor (Figure 1).
Timeline.
Following this patient was referred to us at Medical Oncology Department. On examination her Eastern Cooperative Oncology Group Performance Score (ECOG –PS) was 3. Immunohistochemistry of tumor tissue was done on Ventana BenchMark GX system (Ventana Medical Sytems Inc, Arizona, USA, Roche Diagnostics) using primary antibodies from Ventana Medical Systems Inc, Roche Diagnostic corporation, Indianapolis, Indiana). The immunohistochemistry revealed CD45, CD19, PAX5, CD10 (B-cell markers), Terminal deoxynucleotidyl transferase (Tdt) positive tumor; which was negative for CD3, CD7, CD5 (T- cell markers), CD99, CD34, BCL6 and Desmin. Whole body FDG PET –CT scan was ordered which showed an FDG avid lesion at the L3 vertebra with inter and paraspinal extension (Figure 2). Bone marrow aspiration and biopsy showed normocellular marrow with normal trilineage hematopoiesis, without any infiltration hence flowcytometry was not done. On basis of the results a diagnosis of B-cell LBL was made and she was started on the BFM 2002 protocol.
A repeat whole body PET scan done after completion of the induction phase-2, showed the resolution of the L3 vertebral lesion (Figure 3). Patient gradually recovered neurologically with normal bowel and bladder control and lower limb power. She completed consolidation and re-induction chemotherapy and the maintenance therapy well, with no residual clinically evident disease and remains symptom free as of now three /years since diagnosis.
DiscussionNHL is a heterogeneous collection of lymphoproliferative malignancies with more than 40 different NHL histologies.11 LBL, including B- cell LBL and T-cell LBL are uncommon (2% of all NHL). Of these B-cell LBL is even rarer accounting for only 10% of all LBLs and occurs most frequently in children. The commonest sites of involvement reported in B-cell LBL are lymphnodes, bone and skin (in 75% of cases), with rest occurring in miscellaneous sites such as head and neck (parotid gland and Waldeyer's ring),retroperitonium, breast, ovary, brain and soft tissues.5,6 An epidural location for lymphoma is observed in 0.1 -6.5% of cases of previously undiagnosed NHL. Primary spinal epidural Lymphoma (PSEL) is a subset of these when there is no other recognizable site of disease at the time of diagnosis as in our case.
As our patient presented with back pain, paraparesis and pain in lower limbs, loss of bladder and bowel control and paraspinal mass, and no lymphadenopathy, at presentation the differential diagnosis included metastasis, epidural abscess/ hematoma, meningioma, neurofibroma, malignant peripheral nerve sheath tumors, tuberculosis, parasitosis, herniated discs or tumors. The diagnosis of Spinal Epidural B-cell LBL in this case was clinched on the basis of initial pointer by histopathology results and confirmed by Immunohistochemistry results and FDG-PET CT, absence of bone marrow and peripheral blood involvement. Since at the time of diagnosis there was no other recognizable site of disease diagnosis of Primary Spinal Epidural B-LBL (PSE B-LBL) was made. PSE B-LBL is very rare with only few case reports.7,8,10Table 2 shows the comparison of cases available in literature with case presented in the study.PSE NHL is an uncommon disease, accounting for 9% of epidural spinal tumors. Most PSE NHL are diffuse large B-cell lymphomas and thoracic spine is the most common site of involvement.4,12 The diagnosis of a small round cell tumor on histology is difficult, particularly in children, because the clinical, radiographic, histological and immunophenotypic features overlap.6 The differential diagnosis includes Ewing's Sarcoma, neuroblastoma, mantle cell lymphoma, Burkitts lymphoma, rhabdomyosarcoma, Follicular lymphoma, T-LBL.13 The diagnosis of small round cell tumors can be made precisely by applying clinicopathologic criteria as well as a panel of IHC markers or genetic studies so as to facilitate prompt and accurate diagnosis and treatment (Table 3).
Comparison of case with available literature of Primary spinal B- cell LBL cases.
| Reference | No of patients/ histological Diagnosis | Age /Gender | Primary involvement site | Presenting features | Management | Outcome |
|---|---|---|---|---|---|---|
| Liu H7B-cell LBL | One/B-cell LBL | 16 years/Female | Lumbar spinal epidural | H/O pain in lower back and lower limbs for seven days, weakness of left leg for four days and urinary retention for two days | L3-L5 laminectomy and complete tumor resection followed by systemic chemotherapy with VDCLP | Relieved of urinary incontinence and pain after two months follow up. |
| Nambiar8 | One/ B- cell LBL | 19years/Male | Thoracic Spinal epidural | Weight loss, worsening back pain, b/L lower limb weakness | Partial Laminectomy,Hyper CVAD protocol with CNS prophylaxis (Intrathecal Methotrxate) | Radiological remission on MRI after first cycle.Patient on maintenance therapy at the time of reporting. |
| Awwad10 | One/ B- cell LBL | 6 years/Male | Epidural | Unsteady gait and B/L foot numbness x 3 days (Rapid onset)Urinary incontinence | T1-T6 decompressive Laminectomy and removal of mass, AALL0232 chemotherapy protocol | Recovering 2 months post surgery |
| Present Case report | One/ B-cell LBL | 16 years/ Female | Lumbar spinal Epidural | Lower back and both lower limb pain for six months, inability to walk for three weeks and loss of bowel, bladder control for two dayspain and | Excision biopsy, laminectomy and pedicle screw fixationChemotherapy with BFM-2002 Protocol | Regained bowel bladder control, ability to walk and normal PET CT post induction phase 2,Disease free now three years since diagnosis |
B-cell LBL- B cell Lymphoblastic Lymphoma, VDCLP- Vincristine, daunorubicin, cyclophosphamide, L-asparaginase and prednisone.
CVAD - Cyclophosphamide, vincristine, Adriamycin and dexamethasone.
Histological differential diagnosis of B-cell lymphoblastic lymphoma with the used Panel.
| Lesions | Differentiating feature |
|---|---|
| Ewing's sarcoma | CD99 and CD45- positiveTdT* and B-cell markers negativeCytogenetic studies (t[11,22] with EWS/FLI-1 fusion) |
| Neuroblastoma | Common in abdomen, thorax, pelvis (rare in head and neck)Negative lymphoid markers |
| Blastoff variant of mantle cell lymphoma | Older people- 6th or 7th decadesTdT negative |
| Burkitt's lymphoma | TdT negative |
| Rhabdomyosarcoma | Myogenin- positiveLymphoid markers negative |
| Follicular lymphoma | TdT negative, t (14,18) |
| T-LBL | Mediastinal mass in 50-65% as compared to 4% in B-LBL, absent B cell markers, Positive T cell markers. |
Since our patient presented with symptoms of spinal compression confirmed by MRI, decompression laminectomy along with mass removal was done. In cases of PSEL in whom diagnosis at the time of presentation is not known, surgical decompression in the form of partial/total removal of the tumor mass and /or decompression laminectomy is indicated to alleviate the spinal cord compression and establishment of correct histological diagnosis.14
Post operatively our patient was treated with chemotherapy alone with BFM-2002 protocol. Most authors have preferred chemotherapy with radiotherapy. Oviatt el al15 have reported to have successfully treated two patients with epidural NHL by chemotherapy alone. This case report underlines the need for a certain degree of suspicion towards such an atypical presentation of B cell LBL besides other common causes of such presentation as early diagnosis and aggressive treatment is usually associated with better outcome.
ContributionsConceptualization: Dr. Rajesh Patidar, Dr. Aditya Elhence.
Data Curation: Dr Aditya Elhence, Dr S P Shrivastava, Dr Vikas Asati.
Formal Analysis: Dr. Aditya Elhence, Dr. S P Shrivastava, Dr. Col. P G Chitalkar.
Funding acquisition: NA.
Investigation: Dr Vikas Asati, Dr. Rajesh Patidar, Dr. Aditya Elhence.
Methodology: Dr. Aditya Elhence, Dr. Vikas Asati, Dr S P Shrivastava.
Project Administration: NA as case study.
Resources: Dr Col. P G Chitalkar.
Software: NA as case study.
Supervision: Dr Col. P G Chitalkar, Dr Vikas Asati, Dr Rajesh Patidar.
Validation: Dr. Vikas Asati.
Visulaization: Dr aditya Elhence, Dr Vikas Asati.
Writing original draft: Dr. Aditya Elhence, Dr S P Shrivastava, Dr. Vikas Asati.
Writing-Review & Editing: Dr. Aditya Elhence, Dr Rajesh Patidar, Dr. Vikas Asati, Dr. Col. P G Chitalkar.