Safety in Transfusion Medicine is subject to regulations and government legislation within a total quality framework. The aim of this study was to evaluate the impact of seroprevalence and indeterminate results on lost units and cost per donation.
MethodsA prospective cross-sectional study was performed in the Blood Bank and Transfusion Therapy Department of the Hospital Central de la Policia Nacional del Perú in Lima, Peru. All completed donations (replacement/voluntary) without complications were included in this study. Every donation met the institutional requirements and quality criteria of Programa Nacional de Hemoterapia y Bancos de Sangre (PRONAHEBAS). Data analysis was achieved using the Statistical Package for the Social Sciences.
ResultsA total of 7723 donations were evaluated during 2014 and 2015 with 493 being seropositive (overall prevalence 5.25%) and 502 having indeterminate results (overall prevalence 5.35%). Thus total loss was 995units, 437.8L of blood and 49,750 US dollars. The most common seropositive infectious markers were the core antibody of hepatitis B virus (2.82%) and syphilis (1.02%), and the most common indeterminate results were Chagas disease (1.27%) and the core antibody of hepatitis B virus (1.26%). There was no significant change in the prevalence of seropositivity (p-value=0.243) or indeterminate results (p-value=0.227) over the two-year period of the study. A statistical correlation was found between the cost per lost donation and the most prevalent markers (rho=0.848; p-value=<0.001).
ConclusionSeroprevalence was lower than the regional mean, but the prevalence of indeterminate results was elevated causing a great impact on blood supply and economic losses to this institution.
Safety in Transfusion Medicine is subject to regulations and government legislation within a total quality framework. Safety in transfusion therapy and during donation is an ethical issue in blood banks that must have protective mechanisms that detect noxae and diminish risk, making the transfusion practice efficient, safe and individualized for each patient with donations being free of adverse-reaction events. Nevertheless, new difficulties affect blood supply safety, such as strict donor selection questions, an affordable blood supply, seroconversion periods and emergent agents, among others.1,2
The relative risk from donations is considerable and changing, the reason for which its estimation and its extrapolation to other communities are frequently hindered. In undeveloped countries, the relative risk from donations is heterogeneous due to geographic diversity, the habitat and population groups, as well as to the socioeconomic and educational conditions, and access to healthcare resources.3 Donations in Peru require screening for at least five infectious markers: surface antigen (HBsAg) and the core antibody of hepatitis B virus (HBcAb), antibodies against human immunodeficiency virus (HIV) type 1 and 2 (anti-HIV 1 and/or anti-HIV 2), antibodies against hepatitis C virus (HCV) and anti-Treponema pallidum (syphilis).4 Additionally, antibodies against human lymphotropic viruses (anti-HTLV-1/2) and markers for Chagas–Mazza disease are tested in endemic zones.5,6 The number of tests is not the same in each country because of different socio-sanitary conditions and based on sero-epidemiological data. Additional tests are included for Chagas disease in South America, Canada, Mexico, and some Western Pacific countries, for anti-human T-lymphotropic virus (HTLV)-1/2 in Portugal, France, Taiwan, Japan and Greece, but not in Turkey, for Creutzfeldt–Jacob disease variant (vCJD) in the United Kingdom, Germany, Chile, Portugal and Austria, for West Nile Virus (WNV) in United States, Canada, Australia and India and for anti-plasmodium in Benin.7–13
The effect usually associated to seropositive units is the loss of blood units (biological and economical costs). During the last fifteen years, the reduced blood supply to the Blood Banking Service of a Hospital specialized in maternal care at Lima, Peru, and the great economic impact of discarded blood components was 457.2L of blood and 61,893 US dollars, with limitations in the donation chain. This is also affected by the high-risk of transfusion-transmitted infections in non-healthy populations.6 The prevalences of infectious markers were 0.23%, 4.19%, 0.56%, 1.19% and 0.5% for HIV, hepatitis B virus (HBV), HCV, syphilis and Chagas disease, respectively in units of blood screened in Peru; the overall prevalence was higher than for other countries in the region.6,14–16
Thus, behavioral risk factors, donor quality and geographical endemism generate variable factors that complicate the functioning of blood banks where screening for infectious markers constitutes an invaluable measure to eliminate unsafe blood and avoid adverse transfusion reactions.17
The aim of this study was to evaluate the impact of seroprevalence and the cost per donation in the Blood Bank and Transfusion Service of the Hospital Central de la Policia Nacional del Perú in Lima, Peru during 2014 and 2015.
MethodsAn analytical-correlational cross-sectional prospective study was performed in the Blood Bank and Transfusion Service of the Hospital Central de la Policia Nacional del Perú in Lima. The group of blood donors included in this study was chosen based on all donations with positive and indeterminate results for one or more of the seven infectious markers: HBsAg, HBcAb, HIV 1–2, HCV, Chagas disease, syphilis and HTLV-1/2. The overall prevalences of these infectious markers in Peru were 0.23% for HIV, 0.38% for HBsAg, 0.56% for HCV, 1.19% for syphilis, 0.5% Chagas disease, 0.88% for HTLV-1/2 and 4.19% for HBcAb.16 The cutoff point was derived from the average of three negative calibrators plus a fixed value; indeterminate results were defined as results within the gray zone established by this institution.
All serological tests were performed in duplicate during separate routines. Only samples that had two positive results in two different runs were classified as positive. These results were notified to the Instituto Nacional de Salud of Peru for confirmation using molecular methods, as defined in the epidemiological evaluation programs for disease and patient follow-up.18
Donated blood units considered in this study were selected respecting the donation criteria established by the Programa Nacional de Hemoterapia y Banco de Sangre (PRONAHEBAS) and standard operational process.6,18,19 The ages of all donors were between 18 and 55 years old, donations that were incomplete due to technical issues, those that were associated to complications or were evidently contaminated, were excluded. All the blood donations (replacement/voluntary) were collected in Terumo quadruple blood bags (Shibuya-ku, Tokyo, Japan). As this project was performed at a hospital for police officers, most donors were officers and their families and thus a population group with important and similar risk behavior factors such as their socioeconomic and educational conditions.
Technical data collection and processing of the sampleData collection was carried out using the register book of the Donation Service where samples were discriminated by seropositivity and data were grouped in months and years. The method used for screening was Architect Chemiluminescent Microparticle Immunoassay (Abbott Park, IL, USA). The serological screening was automated using the Architect i1000sr Immunoassay Analyzer (Abbott Park, Illinois, USA) with an incubator and programmable temperature control regulated by Architect i1000sr Software.
The data from the Data Management System for Blood Banks e-Delphyn® register system (Hemasoft, Singapore) was tabulated into the matrix in Microsoft Excel 2010 for Windows (Redmond, USA) where it was coded and the criteria for the verification of methods was evaluated. Data analysis was performed using the IBM Statistical Program for Social Sciences v21.0 (Armonk, USA). KMO and Bartlett's test of sphericity was employed to correlate variables and Varimax Rotation was used for factorial analysis. The Chi-square test was used to assess differences in prevalence between the years of study. Seroprevalence was calculated as the mean, standard error and 95% confidence interval (95% CI) and a p-value <0.05 was considered statistically significant.
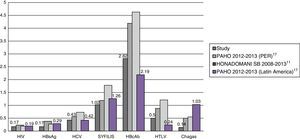
ResultsA total of 9388 donations were evaluated during 2014 and 2015, with 493 having seropositive results (Table 1) giving an overall prevalence was 5.25%. The infectious marker with the most positive results was HBcAb (n=265; 2.82%), followed by syphilis (n=96; 1.02%) and HTLV-1/2 (n=47; 0.50%; p-value <0.01 – Table 1). Five hundred and two units (5.35%) had indeterminate results (gray zone), where Chagas disease (n=119; 1.27%) and HIV (n=28; 0.30%) were the most and least prevalent, respectively (p-value <0.05 – Table 2). There was no significant change in the prevalence of seropositivity (p-value=0.243) or indeterminate results (p-value=0.227) over the two year period of the study. Figure 1 shows the prevalence in this study compared with the regional and national prevalences.
Percentage of seropositive donations for seven infectious markers (n=493).
| Year | HIV | HBsAg | HCV | Syphilis | HBcAb | HTLV | Chagas disease | Total |
|---|---|---|---|---|---|---|---|---|
| 2014 | 0.22 | 0.15 | 0.42 | 0.90 | 2.80 | 0.42 | 0.13 | 5.05 |
| 2015 | 0.12 | 0.19 | 0.43 | 1.13 | 2.84 | 0.58 | 0.14 | 5.44 |
| Of both years | 0.17 | 0.17 | 0.43 | 1.02 | 2.82 | 0.50 | 0.14 | 5.25 |
χ2=0.96; p-value=0.243 (non-significant).
Percentage of indeterminate results in blood donations (n=502).
| Year | HIV | HBsAg | HCV | Syphilis | HBcAb | HTLV | Chagas disease | Total |
|---|---|---|---|---|---|---|---|---|
| 2014 | 0.13 | 0.57 | 1.10 | 0.64 | 1.15 | 0.31 | 0.49 | 4.39 |
| 2015 | 0.45 | 0.60 | 0.82 | 0.66 | 1.36 | 0.35 | 2.01 | 6.24 |
| Of both years | 0.30 | 0.59 | 0.96 | 0.65 | 1.26 | 0.33 | 1.27 | 5.35 |
χ2=0.07; p-value=0.227 (non-significant).
When seropositive and indeterminate losses were compared, the number of seropositive units with a loss of 216.9L of blood (493units) was lower than the indeterminate results (220.9L, 502units); moreover, there was a 24.5% increase in lost blood from 2014 to 2015 (Table 3). Similarly, when the direct cost of seropositive and indeterminate units was analyzed, there was a higher cost related to indeterminate units (25,100USD) compared to seropositive units (24,650USD – Table 3).
Blood loss and cost for seropositive and indeterminate donations (n=995).
| 2014 | 2015 | Total | |
|---|---|---|---|
| Total seropositive units – n | 229 | 264 | 493 |
| Total indeterminate units – n | 199 | 303 | 502 |
| Discarded units – n | 428 | 567 | 995 |
| Lost blood – L | 188.3 | 249.5 | 437.8 |
| Total cost – US $a | 21,400.00 | 28,350.00 | 49,750.00 |
A statistical correlation was found between the cost per lost donation and the most prevalent markers (rho=0.848; p-value=<0.001). Factorial analysis of the seropositive results showed four components that explain the variance: first, the association between HBsAg and HBcAb; second the association between HTLV-1/2 and HIV 1–2; third, the association between Chagas disease and HCV; and the solitary component syphilis (p-value=<0.001). For the indeterminate results, three components were found: First the association between HBcAb, HCV and syphilis; second, between Chagas disease, HTLV-1/2 and HBsAg; and finally HIV alone (p-value >0.004).
DiscussionThis study evaluated the prevalence of infectious markers in police offers and their families who donated blood during the study period and the association with the loss and supply of blood. In Latin American countries, the indicators of safety and supply of blood showed 100% of screening units for infectious markers that determined an overall prevalence of 1.13%.16 Nevertheless, there are few studies about indeterminate, gray zone results and the implications to transfusion medicine and processes of quality assurance.
In the last report, the Pan-American Health Organization (PAHO) reported prevalences of 0.29%, 2.19%, 1.26%, 0.24%, 1.03%, 0.42% and 0.19% for HBsAg, HBcAb, syphilis, HTLV-1/2, Chagas disease, HCV and HIV in Latin American countries, respectively.16 In Peru, only syphilis (1.19%) and Chagas disease (0.5%) are below the regional averages; the values far exceeded the averages for all the others markers, such as HBcAb (4.19%), HIV (0.23%) and dramatically for HTLV-1/2 (0.88%) (Figure 1). In this study we report low prevalences for Chagas disease, HIV and HBsAg, and high prevalences for syphilis and HBcAb in comparison with the last report of the PAHO. It is noteworthy that the overall prevalence of seropositive results increased considerably since the start of the study (0.39%) with values under the regional and national means,6,16 but far below the recent report.20 Furthermore, on comparing the prevalence observed in this study with a previous report in a Mother and Child Hospital which belongs to the Peruvian Ministry of Health (MINSA), all the results were low (half of the previous reported values) similar to the evaluation performed by the PAHO for blood supply in Peru16 (Figure 1). In principle, this suggests that the prevalences of infectious markers in this donor group are correct for this population group of police officers and their families, all of whom had similar risk behavior factors and other conditions.
Similarly, when the overall prevalence of indeterminate results was assessed, most results in the gray zone were related to Chagas disease, HBcAb, HCV and syphilis (Table 2). Two of these diseases are considered endemic in Peru and other countries of Latin America. The risk for Chagas disease constitutes an important problem for transfusion medicine as the screening in blood banks is commonly affected by different factors such as the high prevalence in donors, lack of sensitivity and specificity of the assays, lack of confirmatory tests and cross-reactions. All these factors increase the number of indeterminate results and require the use of techniques that diagnose inconclusive units.14,21,22
In a previous report, 5% of indeterminate results were found for HCV, a percentage far above the regional mean (0.42%).14,16,23 With HCV, approximately 7% of indeterminate units resulted in negative confirmatory tests using a second sample. Thus, we believe that it is necessary to use a confirmatory test and to follow-up these indeterminate donors to demonstrate possible seroconversion which would result in a significant impact on blood banks.23 The high proportion of indeterminate results for HBcAb and syphilis is because the majority of donors have common risk factors for these conditions with a substantial consequence on serological screening in blood banks.13,16,24,25 A 10.6% overall prevalence of seropositive and indeterminate results was estimated. This points to a low quality of donors, high prevalence of infectious markers, the failure of interviews, organizational problems in the blood bank and poor sanitary-epidemiological control of transfusion-transmitted infections in this population.16,20,26
We found a low prevalence for HIV, HBsAg and HTLV-1/2; this rate was similar to several previous reports.27 The current study shows that the risk of HIV- or HTLV-contaminated transfusions is an important difficulty in blood banks due to the characteristics of the life cycles of these viruses. HTLV causes serious leukemoid reactions and chronic myelopathy that has been poorly clarified hitherto.28,29 This disease is characterized by geographic grouping placing Peru at the top of the ranking in Latin America,16 a situation that may explain why the values in this population were less than half those of other studies.6,16 Furthermore, as the infections produced by HIV have increased considerably during the last two decades, and due to advances in technology, molecular tests with enhancements in the detection of pathogens have been developed, but without complete standardization of blood bank laboratories in the community. It is for this reason that the screening for this marker is being improved using conventional tests in order to obtain safe blood.14,25,30–32 The mean rate for HIV-positive blood samples in this study was coincident with previous reports.6,16,27
In addition, in Latin American countries, 29% of discarded blood is related to seropositivity or units reactive for transfusion-transmitted infections, without considering indeterminate units; these results undoubtedly, differ significantly to blood banks in developed countries.33–35 In respect to blood loss for seroprevalence of infectious markers, our results are very low (216.9L per year) compared to a study carried out in a Hospital in Lima where 457.2L of blood of 9560 blood units were discarded over five years, and reports from the Instituto Superior de Medicina Militar in La Habana.6,36 The majority of these discarded units were fresh plasma and red blood cells as mentioned in the last report of PAHO. Our results (10.6%) are also consistent with this report about discarded units (11.3%) (Table 3).16 On the other hand, the values are very different for indeterminate units; in a previous study we reported that in one year 1977 indeterminate (gray zone) units tested using ELISA were discarded in the Hospital of the Seguro Social de Salud del Perú (EsSalud) generating a blood loss of 863.9L.20 The difference with this study is clear as only 220.8L of blood were discarded in one year, 25.4% of that reported in EsSalud. This is due to the 50% of gray zone in screening the institution established for its population of donors (police officers and their families), as a measure to prevent unsafe blood transfusions, but points to a need for standardization of the size of the gray zone for each marker in different populations with different risks and prevalent diseases.
The principal consequence of the discard of units with positive or indeterminate (gray area) results is the quasi-immeasurable economic impact and the limitations in chain donations, principally, in the supply of blood components for institutions. In previous reports on the cost of seropositive-eliminated donations in Peru, 61,893USD were lost in a quinquennium.6 Here, in two years of evaluation, 24,650USD were lost by discarding seropositive units.6,16,36 This varies considerably in the case of indeterminate units, which in the present study corresponds to 25,100USD lost, a relatively low value compared to a study by EsSalud where in only one year 92,640USD were lost, a result that surpasses previous reports about reactive and positive donations.16,20,36,37 These results show a great economic, social and sanitary impact for blood banks attempting to guarantee quality and transfusion safety.
We believe that guaranteeing quality in an initial step could improve processes in all stages of donation and transfusion,2,38–41 through a more efficient process that prevents errors, reduces costs, and satisfies users, etc. This, with the application of good practices in Transfusion Medicine, the promotion of voluntary donations and the implementation of new screening strategies in the health care system will increase safe donations that will save lives.
ConclusionTo conclude, in principle, seropositivity is diminishing compared to the overall prevalence in the region where testing for prevalent diseases is maintained. For indeterminate results, Chagas disease and HbcAb infectious markers are high with the overall prevalence being higher than for positive results. These results depleted the blood supply (discarded units) with a high economic impact.
Conflicts of interestThe authors declare no conflicts of interest.
We are grateful to Dr. José Girard Clavo, Ronald Torres-Matinez, O.R., and to Hospital Central de Policia Nacional del Peru for all their support in this study.