High dose chemotherapy followed by autologous stem cell transplantation is still a salvage therapy for those patients having relapsed Wilms’ tumor. The most common stem cell source is peripheral blood especially after 1995’s with the new approaches and advanced technology in peripheral blood stem cell (PBSC) collection in children.1–3 Although PBSC has been used widely for hematopoietic stem cell transplant there are still lack of standardization in cryopreservation or thawing methods.4
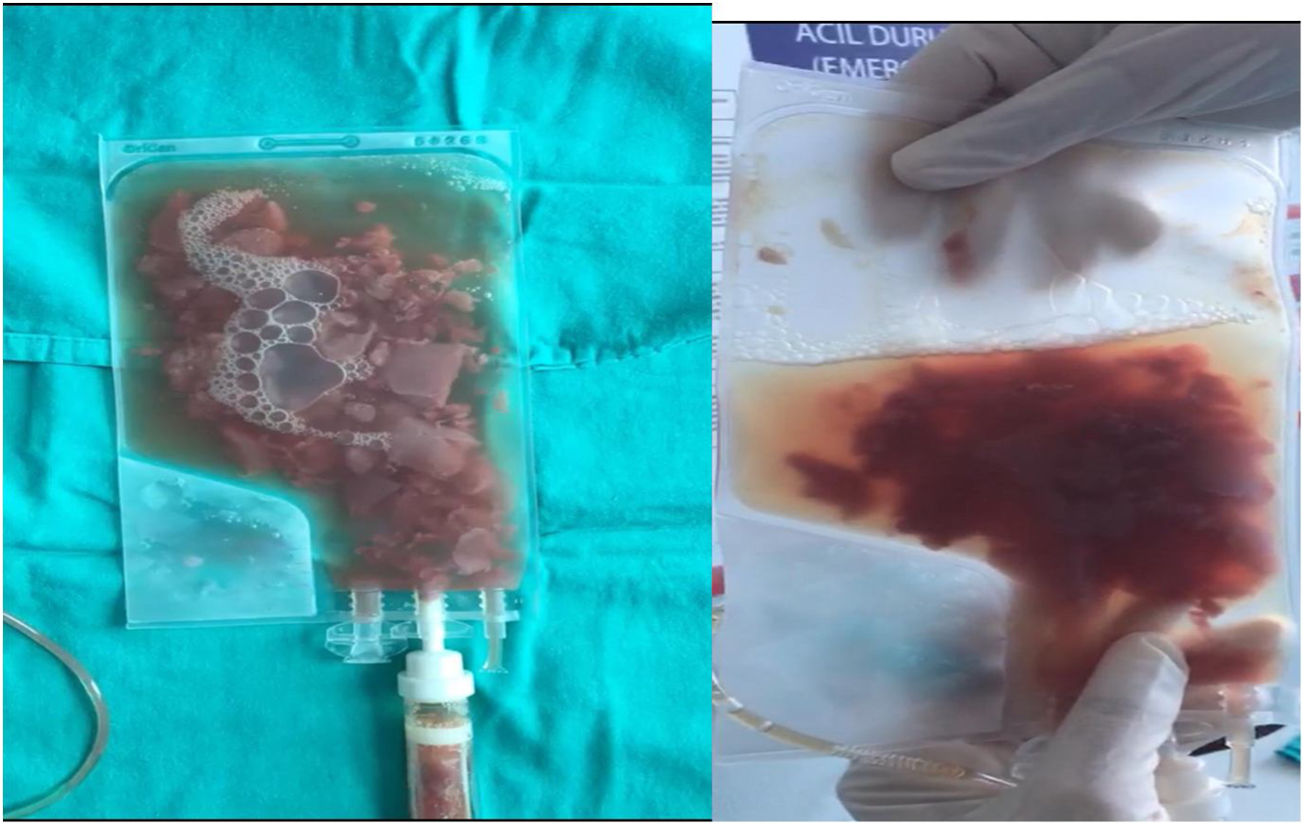
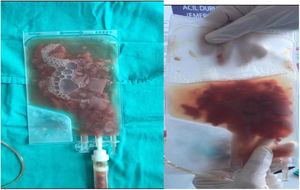
A 3-year-old boy who suffered from relapsed Wilms’ tumor was admitted to hospital on May 2018 to obtain PBSC for autologous stem cell transplant after high dose chemotherapy. The stem cells were mobilized by G-CSF (filgrastim, 10 mcg/kg/day, sc) and CD34+ cell counts were routinely monitored in deciding when to proceed with apheresis. Leukapheresis was performed in one session while enough CD34+ cells were collected by cell separator (Spectra Optia, Terumo BCT, USA). Total CD34+cell count was 1650.64/µL by flowcytometry (BD FACSCalibur, BD Biosciences, USA) in a total volume of 110 ml. PBSC product was diluted with autologous plasma and mixed with cryoprotectant media dimethyl sulfoxide (DMSO %99.9, Origen Biomedical, USA) in a cryopreservation bag (O-wrap bag, Origen Biomedical, USA) with a final volume of 160 ml (max. bag volume 190 ml). Final concentrations of cryoprotectants were %8 DMSO and % 23 autologous plasma. Cryoprotective solutions were mixed with PBSC product under sterile conditions using a laminar hood. The final product was cryopreserved by the way of controlled rate freezing and stored at −196 C in a nitrogenous freezer (LABS-80 K cryogenic freezer, Worthington Industries, USA) which was continuously controlled for temperature by manually and by thermographs for storage till to the date of transplant August 2018 (99 days after collection). At the day of transplant just before the infusion of PBSCs, frozen bags were rapidly immersed in 37 °C sterile water bath for thawing and CD34+count check was done from defrosted product. Immediately after defrost, the product had had a strange formation that was never seen before in our transplant unit. Despite everything being on time sort of clotting has been observed (Figure 1).
The product was immediately infused after being filtered and resampled for CD34+ cells. The new CD34+ cell count was 697/µL by flowcytometry (BD FACSCalibur, BD Biosciences, USA) and no clinical adverse effect had been observed during infusion. Despite a severe loss had been seen on CD34+ cell count, patient had successfully engrafted by neutrophils on thirteenth day by receiving growth factor and on twenty sixth day by platelets in the posttransplant period. The filtered part was examined pathologically whether it is an enormous cell debris and/or clotting. The pathologic results confirmed that specimen is a fibrinoid material containing mostly mononuclear cells. Immunocytochemistry showed %1 CD34+cells, %10 CD20 +, %20 CD3 positive cells.
Fifteen autologous stem cell transplantation out of ninety-eight total was performed in our pediatric transplant unit in 2018 and total 45 cases for five years. This case was the one and only sample which enormous cellular debris was seen in post thaw evaluation, despite up to date technique and equipment had been used to collect and store PBSC. According to literature; presence of cellular debris can cause certain adverse reactions either mild reactions or severe anaphylaxis. It was a risky decision considering probability of undesired reaction but there were no other ways than finishing the infusion, while this was the only product we had and our patient had already in a severe myeloablative situation. Not being able to give enough stem cells to recover hematopoietic system was the other risk, luckily neither posttransplant adverse reactions nor engraftment failure were happened.
Conflicts of interestThe authors declare no conflicts of interest.