Patient blood management (PBM) programs are associated with better patient outcomes, a reduced number of transfusions and cost-savings The Clinical Decision Support (CDS) systems are valuable tools in this process, but their availability is limited in developing countries This study assesses the feasibility and effectiveness of an adapted CDS system for low-income countries.
MethodsThis was a prospective study of the PBM program implementation, in a 200-bed tertiary hospital, between February 2019 and May 2020. Outcome measures were red blood cell (RBC), fresh frozen plasma (FFP) and platelet unit transfusions, the transfusion of a single unit of red blood cells and an RBC adequacy index (RAI).
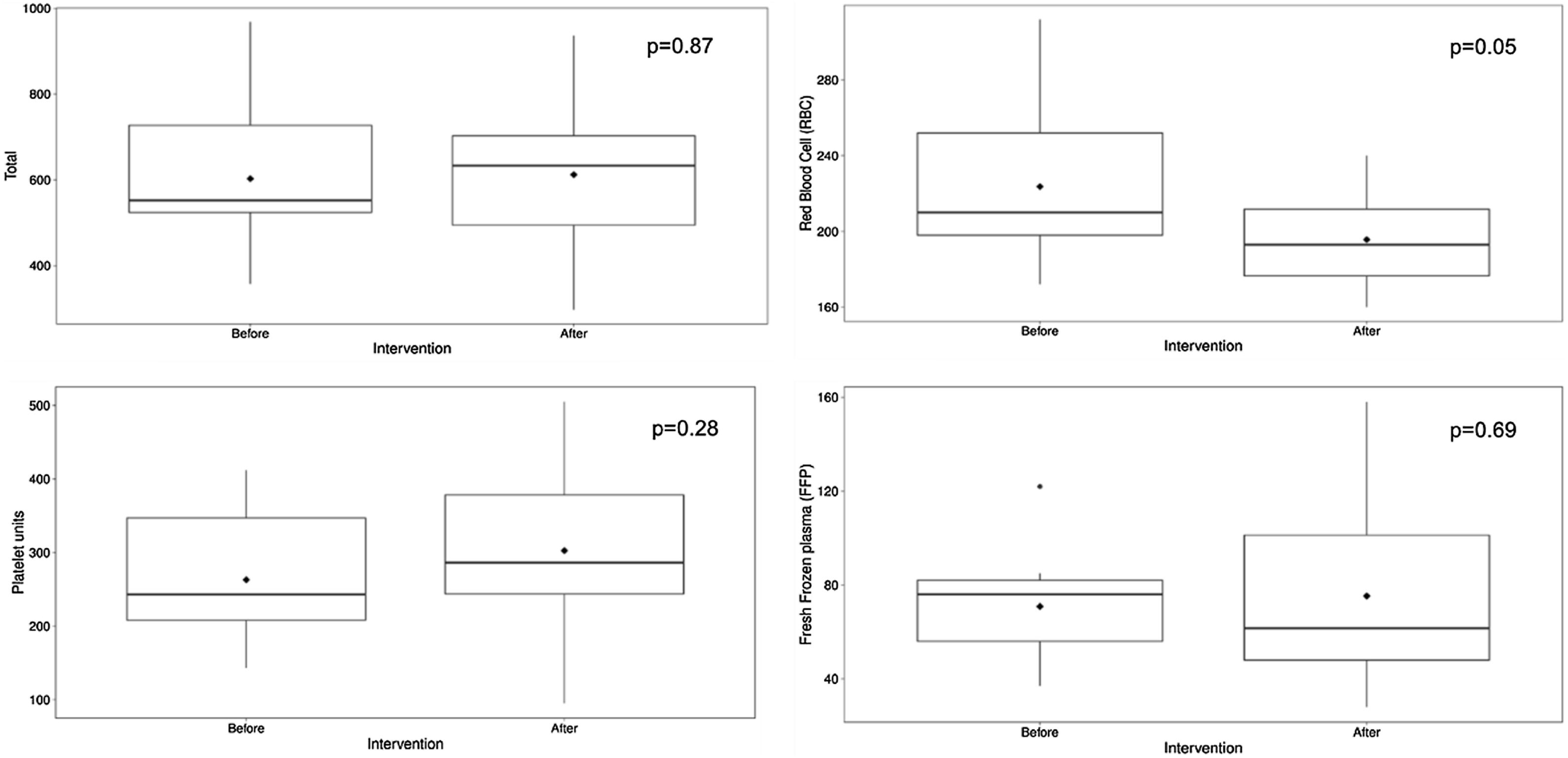
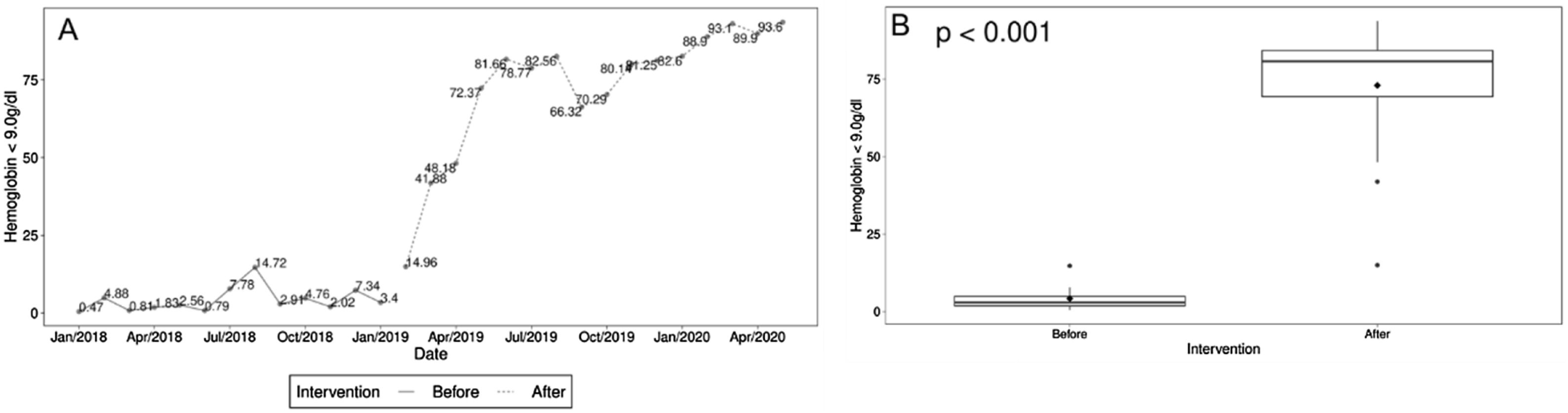
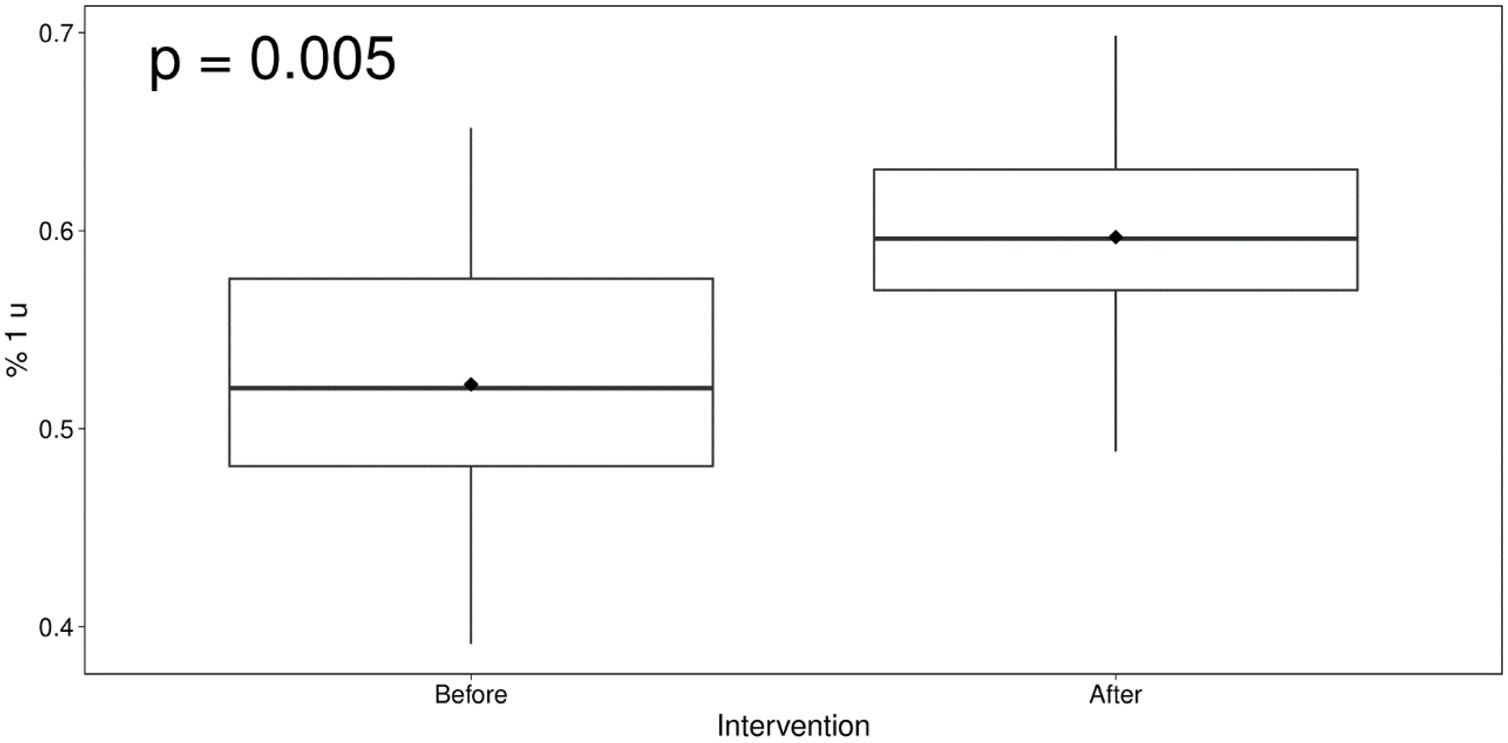
ResultsComparing the post-PBM program era with the pre-PBM system era, there was a decrease in red blood cell transfusions (p=0.05), with an increase in single unit red blood cell transfusions (p=0.005) and RAI (p<0.001).
ConclusionsThe PBM programs, including electronic transfusion guidelines with pre-transfusion medical auditing, was associated with improved transfusion practices and reduced product acquisition-related costs.
The blood transfusion is a very useful tool in the management of a wide spectrum of diseases, being performed in approximately 10–15% of all hospitalizations worldwide.1 Although a lot of improvements have been achieved over the last decades, transfusions are still associated with inexorable risks. In addition, several studies have shown that this tool is frequently used inappropriately Patient Blood Management (PBM) programs are increasingly gaining importance in this scenario PBM stands for a multidisciplinary evidence-based patient-centric approach and can promote better patient care, avoid inadequate use of blood units and optimize clinical outcomes and costs. One of the most important pillars of PBM is the avoidance of unnecessary transfusions.2
Implementation of clinical guidelines to promote education among the physicians is an essential, but insufficient, measure to guarantee its correct use. The requests audit is an important tool to assess the implementation of these protocols. A post-transfusion, retrospective audit can provide information for further education of the clinical staff, but does not prevent the occurrence of inadequate transfusion. A pre-transfusion, concurrent audit is effective in preventing the unwanted blood transfusion, but is a laborious and time-consuming task.
The development of Clinical Decision Support (CDS) systems, in which the clinical guidelines are associated with the electronic prescription software may help in alerting the prescribing physician, based on the available laboratory results, radiology tests and clinical information, to verify if the requested transfusion is compliant with the best practices or should be reviewed. This approach avoids unnecessary use of blood components, promoting a decrease of up to 20% in the volume of red blood cells (RBCs) transfused.3 The CDS system is spreading in the developed world, but there are still some hurdles to overcome in its use in the developing countries. Fragmented health care systems, lack of a national patient medical records and existence of different software modes not integrated in the patient care structure hinder its wide use.
ObjectiveThe main objective of this study was to evaluate the implementation of a PBM program, using a CDS system adapted to the reality of insufficient clinical and laboratory data integration.
MethodsAn institution-validated blood transfusion guideline was integrated in the blood bank software (Table 1). From February 2019 to May 2020, all manually handwritten transfusion requests (regardless of type of surgery and clinical diagnosis) made to the private, tertiary, 200-bed Brazilian hospital, were transcribed by a qualified transfusion technician into the blood bank software, according to the guideline. Orders compliant with the guideline were proceeded to without further delay. The ones that were not possible to classify as adequate were subjected to a concurrent pre-transfusion physician analysis. Inadequate transfusions were discussed with the prescribing physician. In the pre-intervention period, only the mandatory transfusion request data from the legislation was entered into the blood bank software, but there was no systematic pre-transfusion auditing. The data from that time were retrospectively analyzed after the study started.
Blood transfusion guideline inserted into the blood bank software.
| Red Blood cell |
|
|
|
|
|
|
| Platelets |
|
|
|
|
|
|
|
| Fresh Frozen Plasma |
|
|
|
|
| Cryoprecipitate |
|
|
Blood transfusions, RBC transfusions, the rate of single-unit transfusion of RBCs and the RBC Adequacy Index (RAI, percentage of the RBC transfusion requests that had a pre-transfusion hemoglobin available and below 9g/dl)4 were followed prospectively. The parametric variables (total blood transfusion units, RBC transfusions and single-unit RBC transfusion rates were analyzed with the student’s T-test and the nonparametric variables (RAI), with the Wilcoxon test. The data was used to give monthly feedback to the blood bank technicians and auditing physician.
ResultsIn the pre-intervention period, from January 2018 to January 2019, 7,833 blood units were transfused from 3,607 transfusion requests.
In the study period, from February 2019 to May 2020, 9,790 blood units were transfused from 4,555 transfusions requests, of which 3,131 were RBC units. When comparing before and after PBM implementation, there was a statistically significant reduction in RBC transfusions, but not in total blood units, platelets and fresh frozen plasma (FFP), as demonstrated in Figure 1. If the pre-PBM transfusion patterns had remained unchanged, it would be expected that 448 units of RBC would have been transfused during the study.
The RAI is the proportion of the red blood cell transfusions that were performed with a pre-transfusion hemoglobin value available and below 9g/dl. To ensure the reliability of this index, it is necessary to insert all hemoglobin values contained in transfusion requests into the blood bank system. From 2018 to the beginning of the intervention, only a few blood transfusion requests banks had this information, leading to a RAI which reached levels below 5% (Figure 2). With the program implementation, the transfusion orders without hemoglobin or hemoglobin over 9g/dl gradually decreased, promoting increased transfusion adequacy levels, reaching values over 90%, associated with a decrease in the volume of transfused RBCs.
The frequency of single-unit red blood cell transfusions (Figure 3) showed a better performance after intervention, with a significant increase from the pre-PBM era (p=0005).
DiscussionThe blood transfusion has long been known to be accompanied by several risks for recipients. Progress has been made to improve its safety since the implementation of new-generation infectious disease tests, leukoreduction and donor selection criteria, but even so, blood transfusions are still associated with adverse events.5
A patient-centric approach was developed to minimize these risks and promote better care for the individual who might need blood transfusion, named Patient Blood Management (PBM). The PBM programs have been spreading all over the world the concepts of minimizing blood loss, optimizing patient tolerance to anemia and avoiding unnecessary blood transfusion.6
Unnecessary transfusions had already been understood as an important issue, incentivizing the American Hospitals Association to promote it as one of the top five procedures that its hospitals would have to discuss and review.7
In some institutions, up to 76.9% of post-transfusion audit reports found insufficient clinical information to classify transfusions as adequate or not.8 After reviewing 494 published articles and using the RAND/UCLA appropriateness method to determine the appropriateness of allogeneic red blood cell transfusion, based on its expected impact on the outcomes of 450 stable non-bleeding patients, Shander et al. reported that 59% of the red blood cell units transfused were classified as inappropriate.9
The medical review of all blood orders is an expensive and time- consuming task. The use of clinical guidelines and a CDS system that integrate data from the medical records with laboratory results can minimize the unnecessary blood transfusions. In a scenario where there is no integration among all sorts of patient information, implementation of a CDS system is a remote possibility.3,10
The aim of this study was to evaluate the efficacy of a non-integrated CDS system with the medical pre-transfusion review of non-compliant blood orders and educational feedback for the prescribing physicians.
The CDS system implementation, combined with the prospective medical review, was associated with a significant reduction in red blood cell transfusion rates. As stated in previous reports, there is a higher prevalence of inadequate transfusion of RBCs than platelets and FFP. The latter are associated with fewer guideline deviations, by a more highly transfusion-educated physician and frequently after a discussion with the blood bank team. The RBC transfusions are ordered by any physician, with a higher propensity for out-of-protocol requests11
In our study, the implementation of the program was not associated with a change in total blood units, platelets and FFP transfusions. They were considered appropriate by the CDS-driven guidelines or audited by the blood bank physician before proceeding to transfusion. Goodnough et al. reported that the implementation of integrated models of CDS systems with electronic prescriptions and best practice alerts had a primary impact on RBC transfusions.3,10
The effectiveness of the program was also demonstrated by the increase in the red blood cell adequacy index and by the single-unit transfusion ratio. The RAI has been validated in previous studies as a useful tool for real-time blood transfusions management.4 It not only provides information related to the existence of laboratory tests that support the transfusion indication, but is also a qualitative measure related to transfusion thresholds It should be validated at each institution, according to the hospital profile (eg, surgery and obstetrics) and its prospective follow-up can be of great value.12,13
Historically, 2 units of RBCs were ordered when a patient needed a transfusion in the last decade, studies have shown that the adoption of restrictive strategies can be as safe as liberal strategies with lower adverse events and costs.14 As transfusion-related mortality and morbidity is also known to be dose-dependent, the best practices support using the fewest number of units needed to treat the patient.15 Bowman et al. reported that, in hematological patients with similar baseline hemoglobin, the adoption of a single-unit RBC policy resulted in a 29% reduction in RBC utilization, with no significant differences in length of stay, or 30-day mortality.16 Since 2014, the American Medical Association, in partnership with the American Association of Blood Banks, is promoting the policy of single-unit transfusion of RBCs for stable non-bleeding patients as part of the Choosing Wisely Campaign.15
In our study, the single-unit ratio showed a statistical increase, supporting the hypothesis of the CDS system effectiveness, associated with a pre-transfusion medical audit.
In addition to the well-known possible adverse events, the clinical waste of blood units is associated with a high cost. Costs of transfusions have been underestimated in the past by many institutions. If no interventions were made and the annual rate of transfusion remained at baseline levels, an additional 448 RBC units would have been transfused over the study period.
Based on the product acquisition cost, the estimated savings from this reduction during the study is US$ 158,336 (Hierarchical Brazilian Classification of Medical Procedure parameters). The real cost of blood transfusion is reportedly threefold to fivefold times higher than acquisition costs, as it includes indirect costs and costs related to the treatment of adverse events, which might lead to an estimated savings of US$ 445,008 to US$ 791,680 in the sixteen-month intervention period.6
In addition to the possible financial impact, the program could promote more availability of blood, where and when it is needed. The promoting of blood availability is of great importance because an aging population and decreasing number of blood donor candidates generate a dangerous imbalance between the transfusion needs and blood inventory.17
ConclusionsFor the PBM program to reach its full potential, a broader approach is needed, with continuing medical education, pre-operative anemia management, bleeding-adapted surgical techniques, multidisciplinary peri-operative team and an integrated CDS system with best practice alerts. While this integrated model is not something tangible, models using medical auditing, associated with transfusion protocols and physician feedback, can improve care practices and thereby optimize patient clinical outcomes and minimize clinical wastage.
Further studies should be performed, enabling a more detailed financial impact assessment, as well as correlating transfusion data with the epidemiological profile attended at the institution.
Conflicts of interestThe authors declare no conflicts of interest.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors