Anemia is a common issue in surgical patients and has been associated with worse clinical outcomes, such as a higher probability of transfusions and longer hospital stay. Therefore, Patient Blood Management programs are actively aiming to achieve early identification and treatment of anemia, previous to the surgery.
Methods and materialsIn this study, preoperative hemoglobin within the Blood Order Schedule (BOS) at 16 blood centers in several Brazilian regions were retrospectively evaluated. Data regarding hemoglobin, age, gender and Brazilian regions were further analyzed. Results: From the 20,201 BOSs evaluated, the mean age was 55.65 ± 23.52 years old, with an overall prevalence of preoperative anemia of 60.9%. Women had a lower mean preoperative hemoglobin (11.74 ± 2.84 for women and 12.27 ± 3.06 for men) and higher prevalence of anemia than men (66% of females and 52.2% of males). The individuals over 65 years old and under 18 were the most affected by preoperative anemia. All regions had a high prevalence of preoperative anemia, without any direct association with the Human Development Index.
ConclusionIn summary, upon evaluating the BOS, our study showed a high prevalence of preoperative anemia in all Brazilian regions, regardless of the gender and age group, but that women and individuals less than 18 or over 65 years old have an even higher prevalence of preoperative anemia. This information can identify the institutions in which preoperative anemia is a critical issue and in which new strategies, such as preoperative screening clinics, might be helpful.
In recent decades, increased awareness of the risks of transfusion has resulted in initiatives to mitigate those risks through improvements in blood component safety and judicious transfusion practices.1 Although isolated initiatives have been reported previously, significant clinical outcomes improvements were achieved only after implementing Patient Blood Management (PBM) programs.1 The PBM is a patient-centric, evidence-based, integrated, multidisciplinary approach to optimize the clinical outcome by preserving the patient's own blood, mainly by focusing on anemia, coagulopathy and blood loss.1,2
The PBM has been divided into three major pillars: anemia detection and management, optimization of coagulation and minimization of blood loss and boosting of the patient's physiological tolerance of anemia.1,3
Anemia is an independent risk factor associated with adverse patient outcomes and, therefore, its identification and control are considered the first pillar of the program.3–5 It affects 1.95–2.36 billion people worldwide, being one of the most prevalent health issues globally.1,6
The high prevalence and negative impact of anemia in most patients are frequently underrated by surgeons and clinicians. Preoperative anemia (PA) is present in 25–40% of surgical patients.3 These conditions are associated with significantly increased morbidity, mortality, intensive care unit (ICU) occupancy and hospital length of stay.3,6 Therefore, several published recommendations suggest that elective surgery should not be performed on patients with anemia until it be adequately diagnosed and treated.4 As anemia in surgical patients is reported to be more frequent than in the general population and proper diagnosis and treatment may take weeks, early identification during the patient journey is critical.4 In a non-integrated health system, in which patient care is fragmented, anemia detection usually occurs with little time for intervention when the patient is already admitted to the hospital for surgery.
Recent publications argue for a new definition of PA in the setting of high-blood-loss surgery. Although the classic definitions of anemia have distinguished hemoglobin (Hb) levels for males and females, preoperative Hb below 13 g/dL has been reported to increase morbidity, mortality and transfusion, regardless of sex. In summary, in the setting of high-blood-loss surgery, an Hb of 13 g/dL should be used to define preoperative anemia in both men and women.5,7
Another critical issue in PBM programs is the implementation of the maximum Blood Order Schedule (BOS). According to statistics on blood transfusion risk and the number of units transfused, this tool can establish standards for blood crossmatch and preparation for each surgery. In this manner, it can reduce unnecessary transfusions, decrease costs and optimize blood inventory.8 The BOS is especially important in patients undergoing major surgery, which are also the patients most vulnerable to the impact of PA. The BOS is widely available in most hospitals, with easy access to the blood bank database, and can inform the patient status before the surgery.
This study aims to explore the anemia identification in the preoperative setting through the information provided in the BOS.
Material and methodsElectronic medical records of all patients, for whom a BOS was ordered at 16 private blood banks supplying blood for 200 Brazilian hospitals from December 2020 to November 2021, were retrospectively reviewed (n = 37,998). Patients with no Hb information were excluded (n = 17,797). The final cohort for analysis consisted of 20,201 BOSs.
All the blood banks employed the same software (Sistema de Banco de Sangue SBS®, São Paulo, Brazil), with BOS standards being tailored by each institution transfusion history. Every institution's BOS provided the non-obligatory possibility of the insertion of Hb information regarding the surgery or hospital. The age, gender, Hb and hospital region were analyzed. Preoperative anemia was defined as an Hb below 13.0 g/dl, regardless of gender.
A descriptive statistical analysis was performed, continuous data were presented as the mean ± standard deviation and comparisons were made using an independent t-test. Categorical data were presented as the number and percentage of individuals in each category. Statistical significance was set at p ≤ 0.05. Data were analyzed using the NCSS 2020 Statistical Software (NCSS, LLC. Kaysville, Utah, USA, ncss.com/software/ncss).
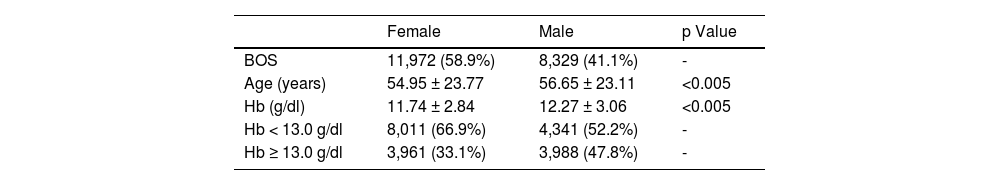
ResultsFrom the 20,201 BOSs included in the study, 58.9% (11,972) were for female patients and 41.1% (8,329), for males. The mean age was 55.65 ± 23.52 years old (54.95 ± 23.77 women and 56.65 ± 23.11 men; p < 0.005). Women had a lower mean Hb than men, 11.74 ± 2.84 versus 12.27 ± 3.06, respectively (p < 0.005). Preoperative anemia was present in 66% (8,011) of the women and 52.2% (4,341) of the men (Table 1).
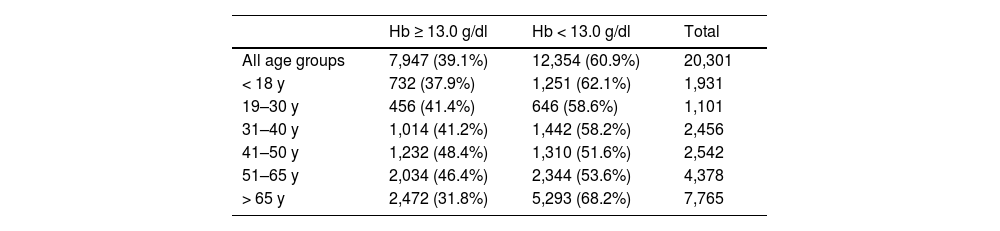
The overall prevalence of PA was 60.9% (12,354). Patients over 65 were the most affected (68.2%), followed by those under 18 years old (62.1%). Adults between 19 and 65 had a prevalence of PA from 51.6 to 58.6% (Table 2).
Preoperative anemia prevalence according to Blood Order Schedule (BOS) Hb and age group.
Hb = Hemoglobin; y = years-old.
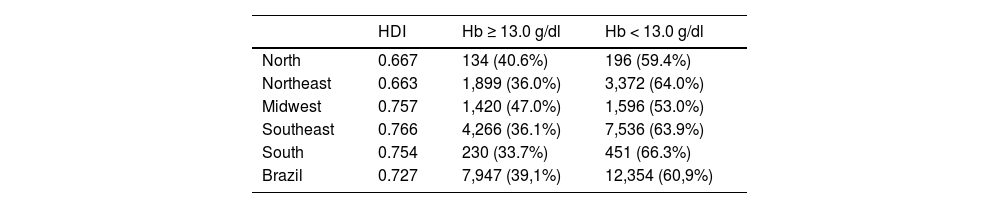
Table 3 shows the prevalence of PA according to the Brazilian region and its Human Development Index (HDI). The less developed areas, such as the northeastern (PA 64%; HDI 0.663) region, had similar PA prevalence to the more developed areas, such as the southern (PA 66.3%; HDI 0.754) and the southeastern (PA 63.9%; HDI 0.766) regions.
Patient characteristics per Brazilian region.
Hb = Hemoglobin; HDI = Human Development Index.
The high prevalence of anemia is an old problem that still impacts billions of people, mainly in non-developed countries. The main etiologies are well known, such as iron deficiency and chronic inflammation.
Anemia definitions have been discussed and a recently renewed version was proposed in the perioperative setting. It has been advocated that, as female patients have a lower circulating blood volume and a similar amount of blood loss by procedure, they are at risk of losing a more significant proportion of their red cell mass than male patients. As a result, a female with the same baseline Hb as a male has a higher risk of developing anemia.5,7 Hence, for a lower hemoglobin threshold (e.g., male 13 g/dl and female 12 g/dl), female patients would be at even higher risk of dismal outcomes. Rosenthal et al. reported that 1388 women who underwent surgery showed that even non-anemic borderline hemoglobin (Hb 12.0 – 12.9 g/dL) was associated with increased red cell transfusion and prolonged hospital stay, compared to higher Hb levels (Hb ≥ 13 g/dL).9
The prevalence of anemia has been reported to be higher in preschool-aged children (47.4%); women of childbearing age (41.8% for pregnant, versus 30.2% for non-pregnant, females); school-aged children (25.4%), and; in individuals over 65 years of age (23.9%).6 The prevalence tends to be lower in men (12.7%).6 In our report, we found that most of the individuals presented with PA, regardless of the sex and age group. Although the definition of anemia used in this study is different from the classic description, we found an important prevalence of PA among women and in individuals under 18 or over 65 years old. In our report, the prevalence of PA in men is higher than the anemia prevalence previous described in the literature. This study corroborates previous reports that found a higher prevalence of anemia in the preoperative setting than in the general population.
According to the Human Development Report, countries are divided, based on the level of the Human Development Index (HDI), into high human development (HDI > 0.8), medium human development (0.5 < HDI < 0.8) and low human development (HDI < 0.5). The numerical value of the HDI is between 0 and 1.10 The HDI measures the mean success of a country in 3 main dimensions of human development: a long and healthy life, access to education and proper living standards.9 Previous reports from the World Health Organization associated the prevalence of anemia with the HDI in all age groups; the higher the HDI, the lower the prevalence of anemia.6 Goodarzi et al. studied the prevalence of anemia in Asian women and reported a significant negative correlation between the prevalence of iron deficiency anemia and mean years of schooling (p < 0.001), life expectancy at birth (p < 0.001), expected years of schooling (p < 0.001) and HDI (p < 0.001).11 In a systematic analysis of national surveys, Moursi et al. reported that a high prevalence of anemia was related to conditions associated with inflammatory exposure (e.g. malaria and infections) among all HDI countries.12 In our report, we evaluated the transfusion requests for patients that have been treated in Brazilian private hospitals. These patients represent mainly the individuals who have access to private health insurance, who are only 22.4% of the Brazilian population.13 This population is associated with a higher income, higher level of education and low prevalence of malnutrition. In summary, the contrast between our study and previous reports can be explained by population selection bias, as the analyzed population in the study does not reflect the HDI of the regions where they are located. Our report uses the BOS order as a tool to identify preoperative anemia. This tool can make a diagnosis of the prevalence of PA at institutions, but is not adequate for individual patient care. The diagnosis of the anemia must be established early in the patient journey towards surgery to improve patient care.14,15 The time for the proper investigation and treatment of anemia is essential for the PA control and better clinical outcomes. Therefore, this initial diagnosis has the objective of increasing awareness of the existing problem so that further measures, such as those taken at preoperative screening clinics, can be further developed.
It is worth noting that this study does not try to explore the correlation between the PA and the patient clinical outcome. However, this has been widely described elsewhere in the literature.3,4,9,13,16 In addition, as the insertion of Hb values in the BOS was not obligatory, a considerable proportion of the medical records had to be excluded from the cohort due to the lack of this information. In this manner, the actual prevalence of anemia in the preoperative setting must be further explored in other studies in which the preoperative Hb value is provided for the entire surgical population. The availability of the Hb information in the preoperative setting is crucial both for the optimal care of the patient, as well as for the blood bank management. From the patient perspective, the early PA diagnosis can promote targeted care, with anemia investigation and treatment, enabling the patient to reach the surgery with better clinical parameters. Moreover, from the blood bank's point of view, the blood supply can be tailored to patient requirements according to the risk of transfusion associated with preoperative anemia. Many centers have adopted electronic medical records to address those issues, the laboratory data being linked to the clinical information, with best practice alerts that permit the physician to rapidly identify the patient at higher risk for a worse outcome. Hence, in some hospitals with more limited resources, the obligatory insertion of the preoperative HB in the BOS could help identify those patients.
Additionally, after identifying the existence of the patient PA, many institutions have created structured processes to diagnose and treat those individuals in an outpatient preoperative anemia clinic setting or even with the education of primary care physicians.5,17 Some of the institutions included in this report have already started their own preoperative anemia clinic, while to others, it is still an on-course task.
ConclusionsIn conclusion, our study demonstrated that the use of a widely available blood bank tool, namely the BOS, enables the diagnosis of the preoperative anemia prevalence in the surgical patient population. Moreover, it also shows that there was a high prevalence of PA in our cohort, regardless of sex, age and HDI. These findings demonstrate the importance of this issue and the need to act. In addition, implementation of PBM programs with preoperative anemia screening, investigation and treatment algorithms can be helpful in this context.
CRediT authorship contribution statementGustavo de Carvalho Duarte: Conceptualization, Formal analysis, Writing – review & editing, Writing – original draft. Glaciano Nogueira Ribeiro: Conceptualization, Formal analysis. Mariangela Moschen: Conceptualization, Formal analysis. Rodrigo Spessotto Morais Toledo: Conceptualization. José Orlando Bordin: Writing – review & editing. Dante Mario : Writing – review & editing.
The authors acknowledge all the blood banks that contributed to this research: Fujisan; Centro de Transfusão e Aférese; Serviço de Transfusão de Salvador; Hemovida Natal; Hemoclínica Distrito Federal; Hemoservice Belo Horizonte; Unihemo Vitória; Hemoserve Vitória; Hemoclínicas Vitória; Hemomed Vitória; Centro de Hemoterapia Celular em Medicina Campinas, Banco de Sangue Paulista; Banco de Sangue de Caxias do Sul; Bioclínica; Serviço de Hemoterapia de São José dos Campos, and; HHemo Hemoterapia Rondônia.