In Brazil, the blood donor screening for hepatitis B virus (HBV) includes laboratory testing for serological (HBsAg and Anti-HBc) and molecular (HBV DNA) markers. This study aims to correlate serology reactive results with HBV DNA detection among blood donors with at least one HBV infection marker detected in a blood bank in northern Brazil.
MethodA retrospective search for HBV reactive blood donor data from January 2017 to December 2019 was performed. Serological screening was performed by chemiluminescent microparticle immunoassays Architect HBsAg and Architect Anti-HBc, whereas molecular screening was performed by the HBV nucleic acid test (HBV NAT).
Main resultsA total of 556 HBsAg reactive results were detected, between positive (47.66%) and inconclusive (52.34%). A total of 3,658 Anti-HBc reactive results were detected, between positive (83.71%) and inconclusive (16.29%). None of the inconclusive results were associated with HBV DNA detection. The HBV DNA detection rates were 47.55% among HBsAg positive samples and 4.08% among Anti-HBc positive samples. The signal-to-cutoff (S/CO) ratio median of HBV NAT positive samples was superior in comparison to HBV NAT negative samples (p < 0.0001). The thresholds found to optimize sensitivity and specificity were 404.15 for Architect HBsAg and 7.77 for Architect Anti-HBc. Three blood donors were in the window period and 1 occult HBV infection case was detected.
ConclusionHigh S/CO ratios were more predictive of HBV DNA detection. However, a number of HBV NAT positive samples gave low values, while some HBV NAT negative samples showed high values, reaffirming the significance of molecular testing to enhance transfusion safety.
Hepatitis B is one of the most important blood-borne viral infections worldwide. According to the World Health Organization (WHO), 296 million people lived with chronic hepatitis B virus infection in 2019. In regard to the mortality, the estimate was approximately 820,000 annual deaths, mostly from liver cirrhosis and hepatocellular carcinoma.1 In Brazil, from 1999 to 2020, 254,389 hepatitis B confirmed cases were reported, with the highest frequency in the southeastern region (34.2%), followed by the southern (31.8%), northern (14.7%), northeastern (10.3%) and central-western (9.0%). In 2020, the overall detection rate in Brazil was 2.9 per 100,000 inhabitants. By region, the highest rate occurred in the southern (7.5), followed by the northern (5.5), central-western (3.0), southeastern (1.7) and northeastern (1.4).2
The hepatitis B virus (HBV) is a small DNA virus externally surrounded by a lipoprotein envelope containing the HBV surface antigen (HBsAg) and internally surrounded by an icosahedral nucleocapsid composed of the HBV core antigen (HBcAg), the viral genome and the DNA polymerase.3 The HBV is spread through contact of mucous membranes or nonintact skin of uninfected individuals with infected blood or body fluids, such as vaginal secretion, saliva, sweat, semen, urine and feces. The transmission may occur through sharing of contaminated objects such as syringes, needles, razor blades and injection drug equipment; from mother to child at birth; occupational accidents; during sexual intercourse and from blood transfusion.4,5
In this context, the laboratory screening for HBV infection in blood donors is mandatory in Brazil as part of the efforts to improve blood transfusion safety. The screening includes serological testing for detection of the HBsAg and antibody to HBcAg (Anti-HBc – IgG or IgG + IgM) and the nucleic acid test (NAT) for the detection of HBV DNA.6 Worldwide, chemiluminescent immunoassays (CLIA) have been widely used in blood donation serological screening, among other antigen/antibody detection methods, such as enzyme-linked immunosorbent assays (ELISA) and electrochemiluminescence immunoassays (ECLIA).7,8
In Brazil, the molecular screening in public blood banks is performed by the national NAT platform for human immunodeficiency virus (HIV), Hepatitis C virus (HCV) and HBV detection, developed by the Immunobiological Technology Institute of the Oswaldo Cruz Foundation (Bio-Manguinhos/Fiocruz, Rio de Janeiro, Brazil). This test allows for the detection of viral genomes in about 10 to12 days after exposure, in the period of infection when neither HBsAg nor Anti-HBc can be detected in the serum, known as the window period (WP).9 The time between exposure and HBsAg detection in the serum is approximately 30 days, whereas the Anti-HBc can be detected about 30 to 60 days after exposure.10,11
The HBV NAT became mandatory in all Brazilian public blood banks in 2016. At the Foundation Center for Hemotherapy and Hematology of Pará (HEMOPA Foundation), its implementation occurred in 2015.12 For this reason, there is still a limited number of studies that establish a notable correlation between serological testing results with HBV NAT results in deferred blood donors. This comparative analysis is important to define the serological and molecular profile of these donors, as well as to indicate the reactive serological test results more predictive of the HBV DNA detection. Thus, the aim of this study was to correlate serology reactive results with circulating HBV DNA detection among blood donors with HBV infection markers detected by serological and/or molecular screening at the HEMOPA Foundation.
Material and methodsStudy design, location and populationThis was a retrospective, cross-sectional, descriptive and quantitative study approved by the Integrated School Brazil Amazon (FIBRA) Research Ethics Committee, under protocol number 4.369.836 (CAAE: 15214919.5.0000.8187) and conducted in the Laboratory of Cellular and Molecular Biology of the HEMOPA Foundation, Northern Brazil. This study included data on blood donors’ samples with at least one serological and/or molecular HBV infection marker detected in the laboratory screening of the HEMOPA Foundation, from January 2017 to December 2019.
Donor databaseQualitative and quantitative serological testing results and qualitative HBV NAT results of the study population were collected from the HEMOPA Foundation systems databases (SBS Web and Progress), which store data on blood donors from all 11 blood donation centers in the State of Pará. Data was filed in research protocols for posterior statistical analysis.
Serological screeningIn the study period, the HEMOPA Foundation performed HBV serological screening using chemiluminescent microparticle immunoassays (CMIA) Architect HBsAg and Architect Anti-HBc (Abbott Laboratories) for qualitative detection and quantification of HBsAg and Anti-HBc (IgG + IgM), respectively. The chemiluminescent reactions were detected by the Architect System optics as relative light units (RLU), which have a direct relationship with the amount of HBsAg or Anti-HBc in the sample. The quantitative results were expressed as the sample-to-cutoff ratio (S/CO), meaning the ratio of RLU detected in the sample to the cutoff RLU defined by the manufacturer (CO ≥ 1), previously established in the active calibration curve. Following the HEMOPA Foundation determinations, samples with S/CO > 1.2 were considered positive; 0.8 ≤ S/CO ≤ 1.2 samples were inconclusive (under gray zone - S/CO within 20% above or below the cutoff), and; S/CO < 0.8 samples were negative. According to the technical regulations for blood establishments determined by the Ministry of Health,6 positive and inconclusive results are considered reactive results and lead to the discard of the blood bags and blood donor deferral.
Molecular screeningMolecular screening for HBV was performed using the NAT Kit manufactured by Bio-Manguinhos/Fiocruz, a real-time polymerase chain reaction-based test (qPCR) with the detection limit of 50 IU/mL. The test was performed in minipools of 6 plasma samples (MP NAT) prepared in the JANUS® automated workstation (Perkin Elmer®). From the pool, viral nucleic acid was extracted and purified in the BioRobot MDx platform (Qiagen). The presence of HBV was detected through specific and discriminatory amplification using fluorescence-labeled probes in the 7500 Real Time PCR System (Thermo Fisher Scientific), which allows for the detection of PCR products in real time. In the case of positive MP NAT results, all 6 samples were retested individually (ID NAT) to identify the positive ones.
Statistical analysisThe software Statistical Package for Social Sciences (SPSS), version 20.0 (SPSS Inc., Chicago, USA) was used for statistical analysis, considering a confidence interval of 95% (p ≤ 0.05). The Kolmogorov-Smirnov test was applied for the assessment of data normality. Descriptive statistics were used to determine the absolute and relative frequencies of qualitative variables and measures of central tendency (median, minimum and maximum values) for quantitative variables. The Mann-Whitney U test was used for comparison between groups and Receiver Operating Characteristic Curves (ROC Curves) analysis was conducted to define thresholds based on diagnostic accuracy.
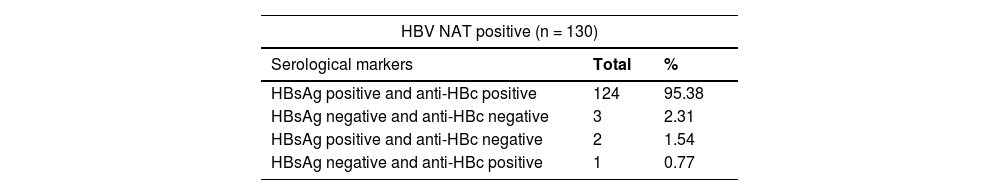
ResultsA total of 286,451 blood donation samples were screened by the HEMOPA Foundation from January 2017 to December 2019. Of these, 4214 (1.47%) reactive results for one or both serological markers were reported, among 556 (0.19%) HBsAg reactive and 3658 (1.28%) Anti-HBc reactive. A total of 156 samples (0.05%) were simultaneously reactive for HBsAg and Anti-HBc. As for the molecular marker, 130/286,451 (0.05%) HBV NAT positive samples were detected, of which 124 (0.04%) were also reactive for both HBsAg and Anti-HBc, 2 (0.0007%) were reactive for HBsAg only and 1 (0.0003%) for Anti-HBc only. Three (0.001%) NAT-only positive samples were reported (0.001%).
There were 265/556 (47.66%) HBsAg reactive results described as positive (S/CO > 1.2) and 291/556 (52.34%) were inconclusive (0.8 ≤ S/CO ≤ 1.2). A total of 3062/3658 (83.71%) Anti-HBc reactive results were positive (S/CO > 1.2) and 596/3658 (16.29%) were inconclusive (0.8 ≤ S/CO ≤ 1.2). All inconclusive/under gray zone samples (0.8 ≤ S/CO ≤ 1.2) for serological markers HBsAg or Anti-HBc were simultaneously negative for HBV NAT. Among HBsAg positive samples, 126/265 (47.55%) were HBV NAT positive and 139/265 (52.45%) were HBV NAT negative. Among Anti-HBc positive cases, 125/3062 (4.08%) were HBV NAT positive and 2937/3062 (95.92%) were HBV NAT negative.
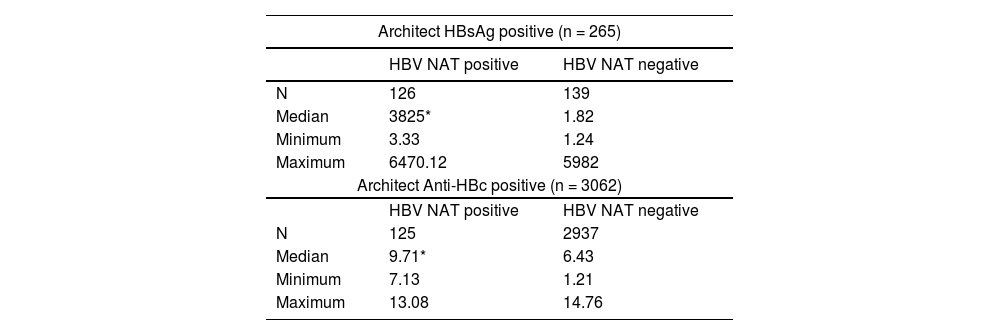
The descriptive statistics of positive S/CO ratios (Table 1) showed medians of 3825 (min-max, 3.33 - 6470.12) for HBsAg positive samples with concomitant DNA detection by HBV NAT and 1.82 (min-max, 1.24 - 5982) for HBsAg positive samples with negative HBV NAT. Among Anti-HBc positive samples, S/CO medians were 9.71 (min-max, 7.13 - 13.08) for those with positive HBV NAT and 6.43 (min-max, 1.21 - 14.76) for those with negative HBV NAT. S/CO values were higher in the HBV NAT positive groups in comparison to HBV NAT negative groups for both HBsAg positive samples (3825 vs. 1.82; Mann-Whitney U = 1086; p < 0.0001) and Anti-HBc positive samples (9.71 vs. 6.43; Mann-Whitney U = 29,174.50; p < 0.0001).
Descriptive statistics of positive S/CO ratios for architect HBsAg and architect anti-HBC positive samples associated with DNA HBV detection by HBV NAT.
| Architect HBsAg positive (n = 265) | ||
|---|---|---|
| HBV NAT positive | HBV NAT negative | |
| N | 126 | 139 |
| Median | 3825* | 1.82 |
| Minimum | 3.33 | 1.24 |
| Maximum | 6470.12 | 5982 |
| Architect Anti-HBc positive (n = 3062) | ||
| HBV NAT positive | HBV NAT negative | |
| N | 125 | 2937 |
| Median | 9.71* | 6.43 |
| Minimum | 7.13 | 1.21 |
| Maximum | 13.08 | 14.76 |
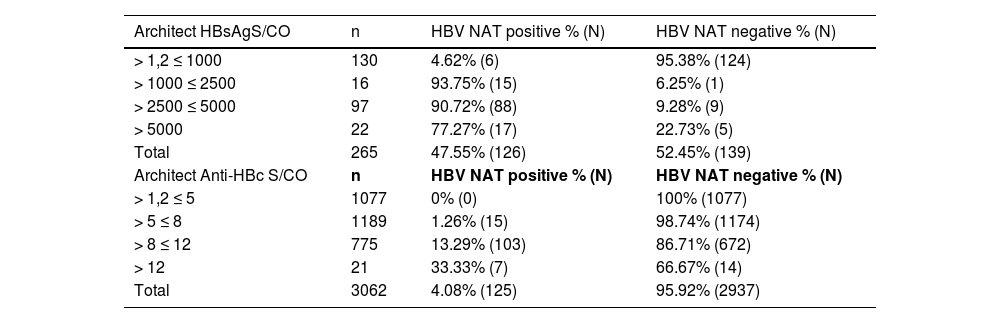
The positive S/CO ratios for Architect HBsAg and Architect Anti-HBc tests were grouped into S/CO ranges based on the overall distribution found for each test (Table 2). The HBsAg positive S/CO ratios distribution varied from 1.24 to 29,114.3. The highest HBV NAT detection rate was found in the range between 1000 and 2500 (93.75%) and the lowest belonged to the S/CO range between 1.2 and 1000 (4.62%). For Anti-HBc positive results, the S/CO ratios distribution varied from 1.21 to 8912. The range with S/CO ratios greater than 12 had the highest HBV NAT detection rate (33.33%), while the S/CO range between 1.2 and 5 showed total absence of HBV NAT detection.
Comparison between S/CO ratio ranges: HBV NAT positive and HBV NAT negative sample.
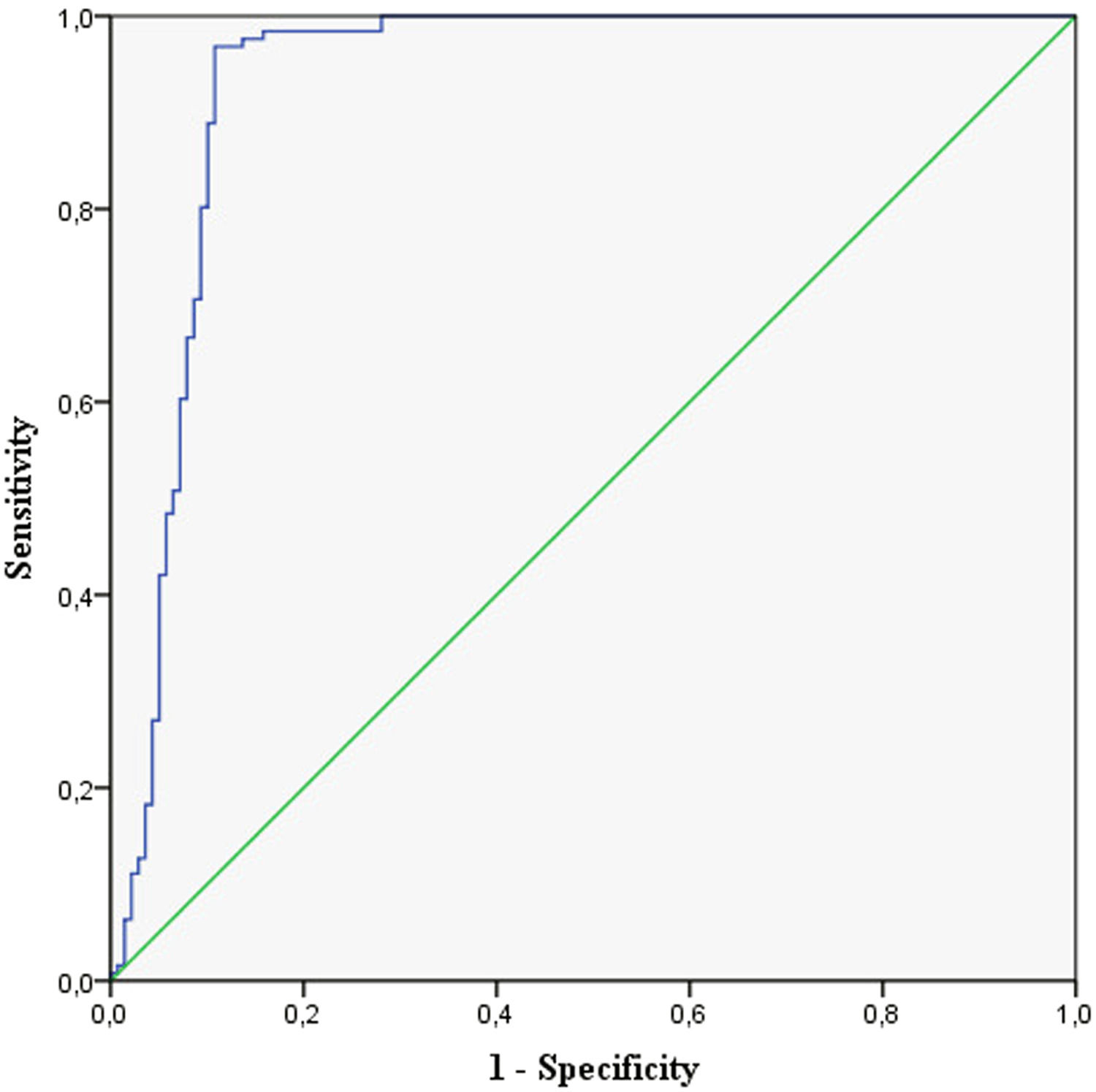
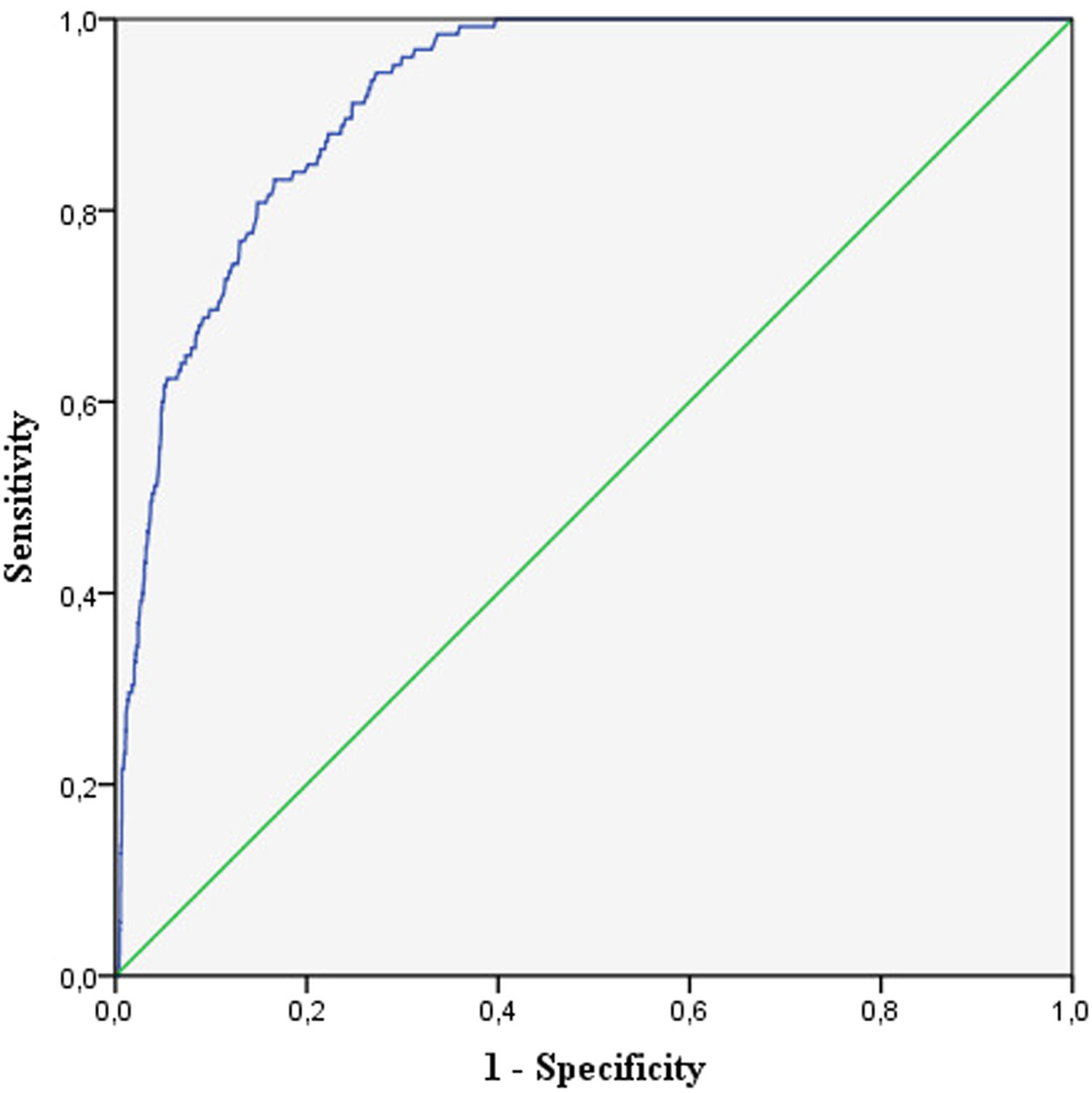
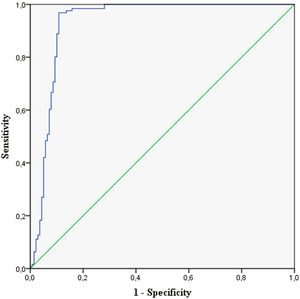
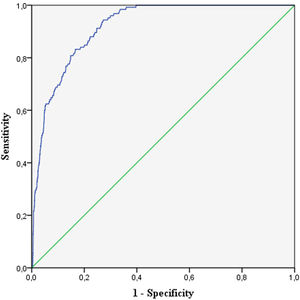
The ROC curves (Figures 1 and 2) were constructed to define thresholds that optimize diagnostic accuracy of the Architect HBsAg and Architect Anti-HBc, considering the variation in sensitivity and specificity of different S/CO ratios of positive HBV NAT samples and negative HBV NAT samples. The results demonstrated statistically significant curves for both the Architect HBsAg (AUC = 0.931, SE = 0.018, p = 0.000; 95% CI = 0.895 – 0.967) and Architect Anti-HBc (AUC = 0.917, SE = 0.009, p = 0.000; 95% CI = 0.900 – 0.935), in which the abbreviation AUC means the area under a curve, SE means the standard error and CI means the confidence interval.
For Architect HBsAg, the threshold with maximized sensitivity and specificity was 404.15 (sensitivity = 96.83% and specificity = 89.21%.), meaning this threshold has greater capacity to discriminate blood donors with circulating HBV DNA (96.83% of probability when S/CO > 404.15) of those with undetectable HBV DNA (89.21% of probability when S/CO < 404.15). The threshold defined for the Architect Anti-HBc was 7.77 (sensitivity = 94.40% and specificity = 72.73%).
The 130/4062 (3.2%) deferred blood donors due to the detection of one or more HBV infection markers in the serological and molecular screening were HBV NAT positive (Table 3). A total of 124 (95.38%) of these donors were simultaneously positive for HBsAg and Anti-HBc (HBV DNA+/HBsAg+/Anti-HBc+); 3 (2.31%) were negative for HBsAg and Anti-HBc (DNA HBV+/HBsAg-/Anti-HBc-); 2 (1.54%) were HBsAg positive and Anti-HBc negative (DNA HBV+/HBsAg+/Anti-HBc-), and; 1 donor (0.77%) was HBsAg negative and Anti-HBc positive (DNA HBV+/HBsAg-/Anti-HBc+).
DiscussionThis study described a prevalence of 1.47% for HBV serologically reactive results, with higher rates for Anti-HBc (1.28%) in comparison to HBsAg (0.19%) and a prevalence of 0.05% of samples reactive for both serological markers. The same pattern was found in a study conducted with Brazilian blood donors by Calegaro et al.13, in which the prevalences were 1.08% for HBV serologically reactive results, 0.94% for Anti-HBc, 0.12% for HBsAg and 0.02% for HBsAg and Anti-HBc together. In regard to the HBV NAT, 0.02% NAT positive samples were described, all of them reactive for HBsAg and Anti-HBC. This prevalence was close to the one found in our study (0.05%). However, despite the highest rate of HBV DNA+/HBsAg+/Anti-HBc+ (0.04%) among HBV NAT positive samples, different patterns were reported as well.
The relative frequencies observed for HBV serological infection markers were in accordance with the results reported by Bitencourt14 at a blood bank in northern Brazil. From the total of reactive results in HBV serological screening, 12.37% (35/283) were reactive for the Architect HBsAg and 87.63% (248/283) were reactive for the Architect Anti-HBc, similar to the values found in our study.
The cases of positive results for HBsAg or Anti-HBc with concomitant HBV DNA detection by HBV NAT were less frequent in comparison to those with undetectable HBV DNA. Lelie et al.15 inferred the proportions of HBsAg positive blood donation samples using chemiluminescent immunoassay (CLIA) associated with HBV DNA detection at blood establishments worldwide grouped into 6 regions (North and Central Europe, Mediterranean, Egypt, South Africa, Southeast Asia and Oceania). The detection rates ranged from 90.2% to 96.3%, considerably higher proportions than those of our findings (47.55%). In Western India, the HBV DNA detection rate among HBsAg reactive blood donors by the ELISA was 65%.16 According to a study by Manzini et al.17, conducted in northwestern Italy, the HBV DNA detection rate among Anti-HBc positive blood donors using CMIA was 4.86%, similar to our study (4.08%). In eastern Libya, the proportion of Anti-HBc positive blood donors using the ELISA with simultaneous HBV DNA detection was 9.5%.18
The discrepant detection rates reported in the studies may be related to differences concerning HBV infection endemicity among regions due to variable implementation of childhood and birth-dose vaccination programs, prevalence of injection drug use and education initiatives.19 According to the WHO,1 the burden of the hepatitis B infection is highest in the Western Pacific Region, where 116 million people are chronically infected, followed by the African (81 million), Eastern Mediterranean (60 million), Southeast Asia (18 million) and European (14 million) Regions. The Region of the Americas, that includes Brazil, contain the lowest number of HBV-infected individuals (5 million). Moreover, strong decreases in the HBV prevalence have been observed in the southern region of the Americas (Argentina, Brazil, Peru, Venezuela) in recent years.20 Candotti et al.21 suggest that discrepant results in blood donation screening for multiple HBV markers are difficult to evaluate, as they largely depend on the performance of the assays used, considering factors such as sensitivity and specificity.
The present study has found that 100% of the cases with inconclusive results (0.8 ≤ S/CO ≤ 1.2) in serological screening for HBsAg or Anti-HBc were HBV NAT negative. At the HEMOPA Foundation, inconclusive results belong to the gray zone, which encompass S/CO ratios within 20% above or below the cutoff (CO = 1), as a manner in which to enhance blood transfusion safety. Bhardwarj et al.22 also found that none of the samples with gray zone results in the screening for transfusion transmissible infection (TTI) markers in blood bank, HBsAg included, proved to be positive in confirmatory testing. These findings suggest the limited value of inconclusive results to predict confirmed positive results.
A study by Kiely et al.23 evaluated the capacity of chemiluminescent immunoassays for detection of HBsAg and other TTI markers to discriminate between biologic false-reactive (BFR) and confirmed positive results in blood donation screening. It was found that high S/CO ratios were predictive of confirmed positive results, in line with our findings, that showed higher S/CO ratios for HBV NAT positive groups in comparison to HBV NAT negative groups (p < 0.0001). However, it must be highlighted that some HBV NAT positive samples gave low values, while some HBV NAT negative samples showed high values.
Except for Anti-HBc positive cases with S/CO ratio ranging from 1.2 to 5 (total absence of HBV DNA detection), HBV NAT positive and HBV NAT negative results were observed for each S/CO ratio range of HBsAg positive and Anti-HBc positive samples. Kiely et al.23 also reported overlaps in S/CO ratio distributions of BFR and confirmed positive samples for all assays evaluated, emphasizing the need for molecular screening and serological confirmatory testing to define a final donor status.
The thresholds with maximized intersection of sensitivity and specificity for the Architect HBsAg (404.15; sensitivity = 96.83% and specificity = 89.21%) and the Architect Anti-HBc (7.77; sensitivity = 94.40% and specificity = 72.73%) reinforced that high S/CO ratios are more likely to discriminate between viremic donors and nonviremic donors. The ROC curves were statistically significant, as reported by Sommese et al.24, when the optimized threshold for CMIA HBsAg reactive blood donor samples submitted to the HBsAg neutralization confirmatory assay was 100 (sensitivity = 94.7% and specificity = 94.6%).
Corrêa et al.25 found that the HBV NAT implementation at the HEMOPA Foundation has improved blood transfusion safety by reducing the residual risk (RR) of transfusion-transmitted HBV infection and, furthermore, enabled the HBV detection in 3 WP donations and 6 occult HBV infection (OBI) cases from 2015 to 2016. In the present study, out of 130 confirmed HBV-infected donors, 3 (2.31%) HBV DNA+/HBsAg-/Anti-HBc- were considered WP cases, with a prevalence of 0.001%, and 1 (0.77%) HBV DNA+/HBsAg-/Anti-HBc+ was considered an OBI case, with a prevalence of 0.0003%.
Internationally, several studies have reported a reduction in the HBV WP and RR with the implementation of the HBV NAT at blood banks, owing to the detection of the HBV DNA in the early stages of infection, before the development of the HBsAg and Anti-HBc in the donor blood.26,27 However, the rate of detection of NAT-only positive donations varies according to several factors, such as the regional HBV prevalence and whether Anti-HBc testing has been included. It also depends on the selected pool size in terms of the MP NAT.28 Roth et al.29 described NAT-only detection rates that varied among different world regions from 2.17 to 105.34 per million, considering a total of approximately 114 million donations between 1998 and 2008.
As observed in this study, the HBV DNA testing also allows for the detection of the HBV DNA in individuals who test negative for the HBsAg and positive for the Anti-HBc, the pattern of HBV chronic infection known as OBI. Among HBV-infected blood donors, the median prevalence of the OBI detection is approximately 1%, but it is dependent on the epidemiology of the studied population and the sensitivity of the HBV DNA test.28 In Brazil, the OBI prevalence rates have ranged from 2.7% (North and Northeast) to 3.3% (South).30 The profile HBV DNA+/HBsAg+/Anti-HBc- found in 2 (1.54%) HBV-infected donors, with a prevalence of 0.0007%, may be suggestive of recent infection, in the acute period before the appearance of the Anti-HBc in the serum due to the natural course of hepatitis B.10 Another possible explanation would be a weak immune response of these donors, compromising an effective production of antibodies.
The serological profiles of HBV NAT positive donors described in this study (Table 3), were comparable to the ones described in the large-scale multi-regional study by Lelie et al.15, in which 84% of the HBV-infected donors, confirmed by means of the HBV DNA detection, were simultaneously positive for the HBsAg and Anti-HBc (HBV DNA+/HBsAg+/Anti-HBc+); 2.65% were considered WP cases (HBV DNA+/HBsAg-/Anti-HBc-) and 5.9%, OBI cases (DNA HBV+/HBsAg-/Anti-HBc+).
ConclusionsIn summary, high positive S/CO ratios showed more association with the circulating HBV DNA detection by the HBV NAT. Gray zone results were specially less predictive of viremia, given the total absence of the HBV DNA detection in serologically inconclusive samples. However, this study reaffirmed the importance of enhancing blood transfusion safety through molecular screening, since a number of HBV NAT positive samples gave low S/CO ratios in serological screening and below the thresholds defined by the ROC curve analysis. Moreover, the HBV NAT enabled the detection of 2 WP donations and 1 OBI case in the study period.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.