Transfusion of platelets (PLTs) with high ABO antibody titres can pose a risk of hemolysis if the unit crosses the ABO type. The PLTs stored in the platelet additive solution (PAS) remove asubstantial fraction of plasma and replace it with an isotonicbuffered solution.We aimed to assess the difference in anti-A/B antibody levels in Groups O, A and B apheresis platelets (APs) suspended in plasma and PAS.
MethodologyApheresis donors are categorized into two groups, Plasma (Group I) and PAS (Group II), each blood group (A, B and O) had 20 samples. The anti-A/B(IgM)antibody levels were recorded from the AP donor (Group II) and from the AP units for both groups. The reduction in the anti-A/B(IgM) antibody levels in the APs suspended in the PAS for each blood group was determined.
ResultsThe median anti-A titres in blood Groups B (p = 0.009) and O (p = 0.005) was significantly lower in Group II. However, the difference in anti-B levels was not significant in the blood groups A (p = 0.057) and O (p = 0.205). The median level of reduction in IgM antibody titres across donor samples and the PAS-stored platelets was two-fold. The regression showed a level of reduction in antibody titres which can be explained by baseline donor antibody titres in blood groups A and B compared to blood group O.
ConclusionThe medianABO antibody titres were lower in APs suspended in PAS than in plasma. Addition of the PAS significantly lowered the IgM antibody titres by twofold, compared to plasma.
Platelet (PLT) units are routinely suspended in donor plasma during storage. The PLT units contain significant amounts of ABO antigen on their surface and anti-A and anti-B antibodies in the plasma.1 The PLT units are transfused ABO-identical if available,1 but if the transfusion is across the blood group, the PLT units with high ABO antibody titres can pose the risk of hemolysis.2 This risk is greater when group O PLTs are transfused to non-O patients.2
As single apheresis platelets (APs) contains 200–400 ml of plasma, multiple methods are employed to limit the risk of hemolysis, such as avoiding transfusion of platelet units with high titre antibodies, limiting quantities of incompatible plasma transfused by plasma reduction and diluting ABO incompatible plasma with Platelet Additive Solution (PAS).3–5 As no guidelines exist for platelet transfusion across blood group in India, most of the centers do not routinely practice the above-mentioned methods to limit the risk of hemolysis. Use of PAS for storing PLTs has gained importance, as they remove a substantial fraction of plasma and replace it with an isotonic buffered solution in a ratio of 65% PAS / 35% Plasma.2 Previous research reported that a reduction in the amount of plasma leads to a concomitant reduction in ABO antibody levels in the PLT unit when stored with PAS.2
As donor specific variables and environmental factors are associated with changing anti-A and anti-B titre levels in donors, a regular survey on ABO antibody levels in the donor population should be performed for each country and ethnic group.6,7 Earlier studies observed the effect of the addition of PAS on ABO antibody levels only in the O blood group.2,3
The aim of the study was to assess the difference in ABO antibody levels in Group O, A and B apheresis platelets suspended in Plasma and PAS. The objective was to further investigate the level of reduction in IgM ABO antibody titres between peripheral blood of donor and PLTs suspended in PAS across O, A and B blood groups.
Materials and methodsThe present study was a cross-sectional study conducted from August 2018 to July 2019 at a tertiary care cancer center of South India. Institutional review board committee approval was obtained for the study.
Study populationApheresis donors, for whom quality control was performed, were categorized into two groups based on PLTs suspended with Plasma (Group I) or PAS (Group II). Within each group 20 donors of blood groups A, B and O were included. The ABO antibody levels were recorded from peripheral blood of the apheresis donor for Group II (PAS) and from the AP units for both Group I (Plasma) and Group II (PAS). The reduction in the level of the ABO antibodies between the donor and AP units suspended in PAS (Group II) for blood groups A, B and O were determined.
Titration procedureAntibody titration was determined on day 1 of the AP collection throughout the study samples. Antibody titration was performed by serial two-fold dilutions for anti-A and anti-B IgM antibody levels by the immediate spin method using the conventional tube technique. The titre was interpreted as the reciprocal of the highest dilution that yielded a 1+ macroscopic reaction. To avoid inter-examiner variation during testing, all testing were performed by the same individual, blinded throughout the study.
Statistical methodsDescriptive data was expressed as the median with the inter-quartile range. The Mann Whitney U test was used to compare the ABO antibody levels in the APs suspended in Plasma (Group I) and PAS (Group II). The reduction in the ABO titer between peripheral blood of the donor and PAS suspended AP units was analyzed using the Wilcoxon Signed Rank test for each ABO Blood group. The Spearman’s rho correlation and simple linear regression model were used to assess the level of variation in the antibody titers before and after the addition of PAS in Group II.
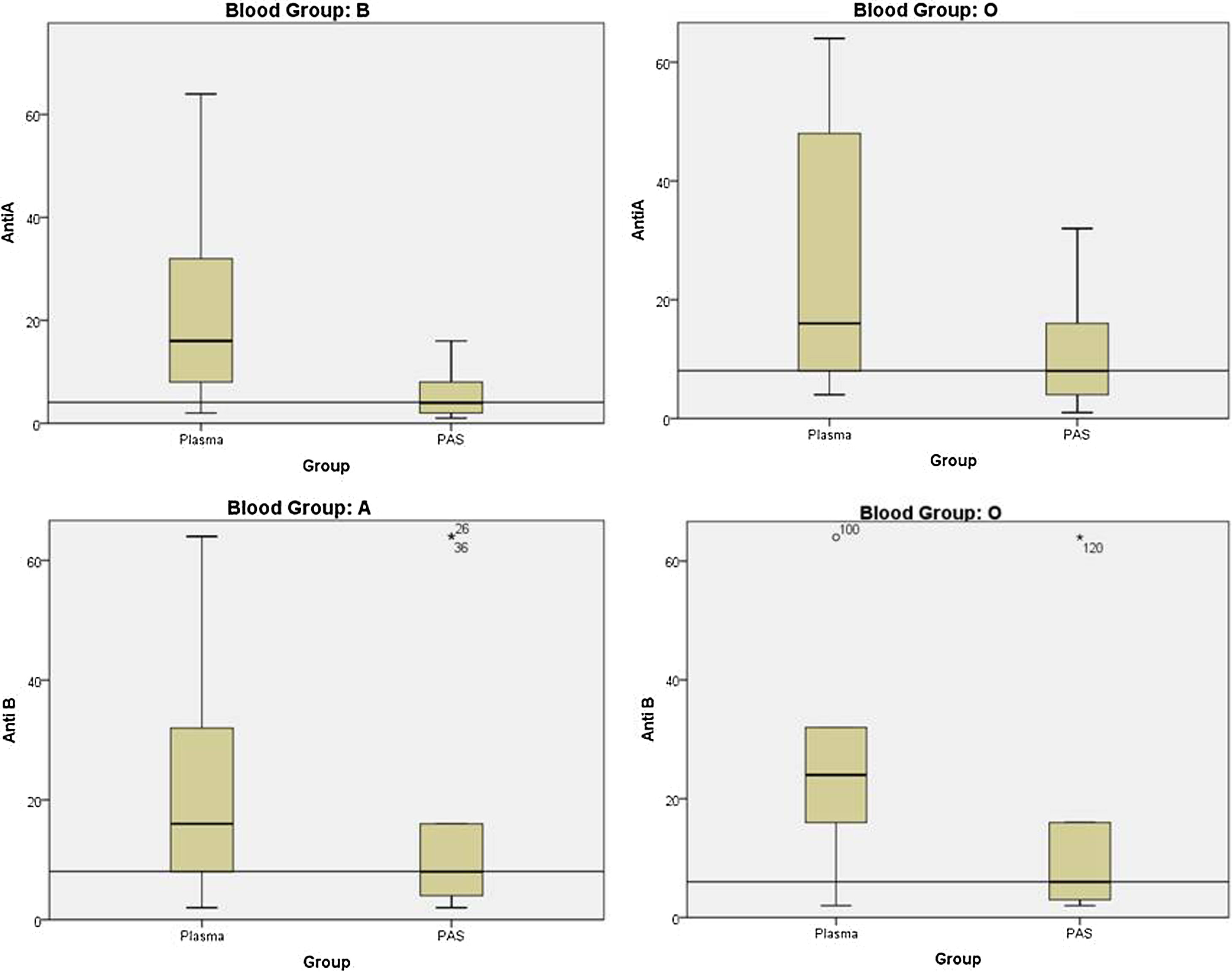
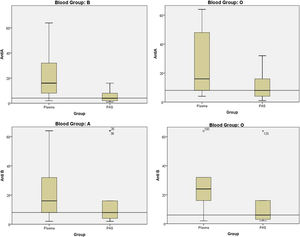
ResultsA total of 120 samples were included in this study. Each blood group (A, B and O) had 20 samples between group I (Plasma) and Group II (PAS). The median Anti-A and Anti-B titre in blood groups A, B and O is shown in the Table 1. The median Anti-A antibody titre level in blood group B (p = 0.009) and O (p = 0.005) was significantly lower in Group II (PAS), as compared to Group I (Plasma). Even though there was a reduction in the Anti-B antibody titre level in blood groups A and O between Group I (Plasma) and II (PAS), the difference was not statistically significant [group A (p = 0.057) and O (p = 0.205)]. (Figure 1) The median level of reduction in the IgM antibody titres across Groups A, B and O between peripheral blood of the apheresis donor and the APs suspended in PAS was twofold.
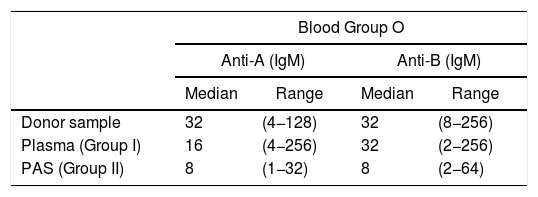
ABO antibody titre in donor sample, plasma-stored platelets and PAS-stored platelets among blood groups A, B and O.
| Blood Group O | ||||
|---|---|---|---|---|
| Anti-A (IgM) | Anti-B (IgM) | |||
| Median | Range | Median | Range | |
| Donor sample | 32 | (4−128) | 32 | (8−256) |
| Plasma (Group I) | 16 | (4−256) | 32 | (2−256) |
| PAS (Group II) | 8 | (1−32) | 8 | (2−64) |
| Blood Group B | Blood Group A | |||
|---|---|---|---|---|
| Anti-A (IgM) | Anti-B (IgM) | |||
| Median | Range | Median | Range | |
| Donor sample | 16 | (4−128) | 32 | (8−256) |
| Plasma (Group I) | 16 | (2−128) | 16 | (2−64) |
| PAS (Group II) | 4 | (1−16) | 8 | (2−64) |
PAS: platelet additive solution.
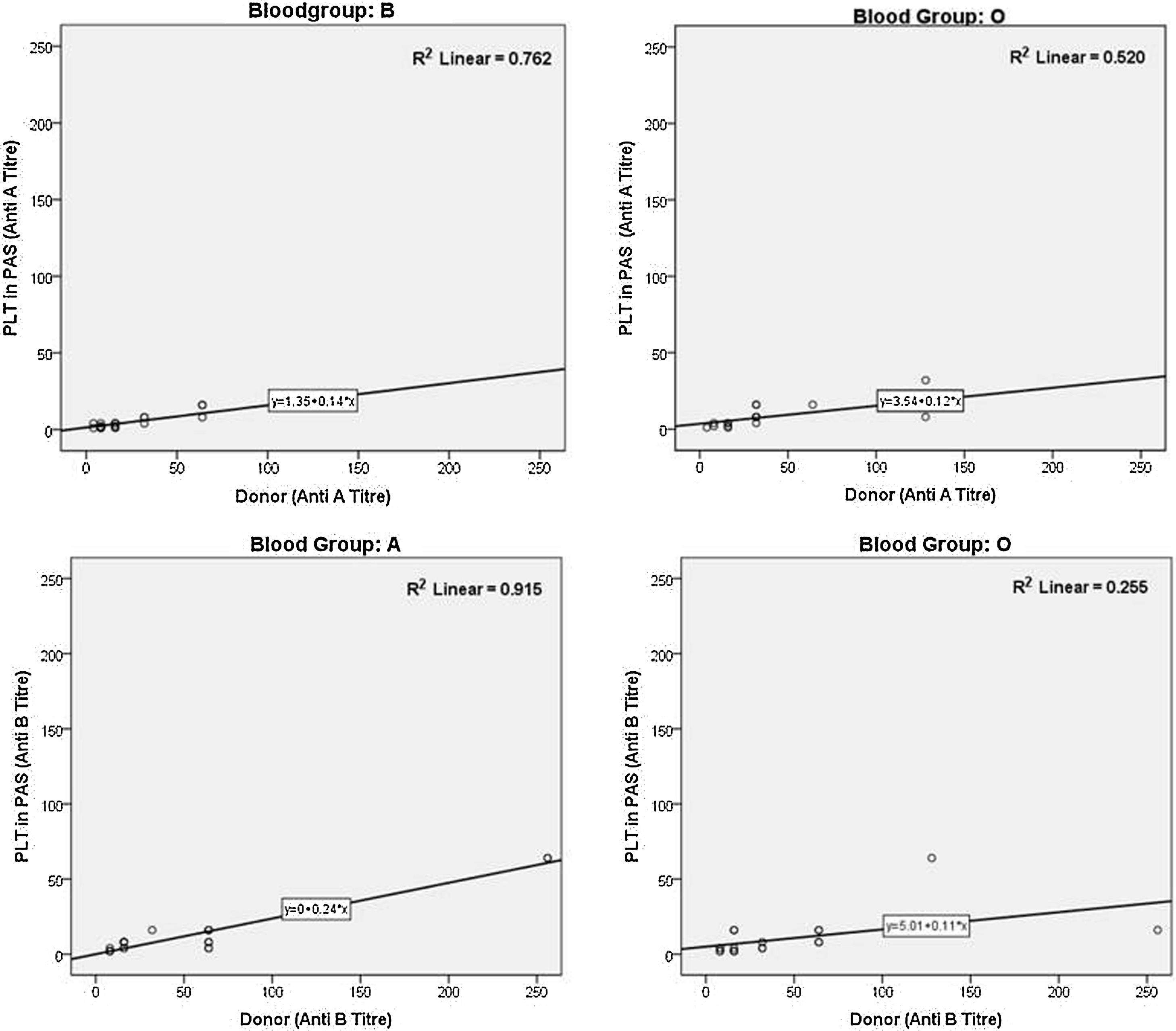
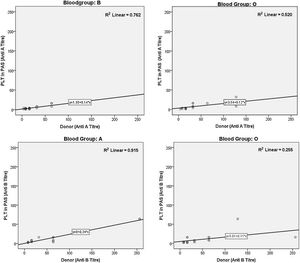
A strong positive correlation was observed with a reduction in the antibody titre between peripheral blood of the apheresis donor and the AP suspended in the PAS in each blood group A (Anti-B, r = 0.755), B (Anti-A, r = 0.779) and O [(Anti-A, r = 0.855) and Anti-B, r = 0.714)] (p-value = 0.00) (Figure 2). A simple linear regression model showed a 91.5% reduction of Anti-B titre levels in the AP suspended in the PAS (Group II) and was explained by baseline donor sample Anti-B titres in blood group A. Similarly, a 76.2% reduction of Anti-A titre levels in PAS stored platelets was explained by baseline donor sample Anti-A titres in blood group B. However, in blood group O, only 52% and 25.5% reductions of Anti-A and Anti-B titre levels in the AP suspended in the PAS (Group II) was explained by baseline donor sample Anti-A and Anti-B titres, respectively.
DiscussionThe present study observed the AP suspended in the PAS (Group II) had median two-fold lower IgM antibody titre levels (in both Anti-A and Anti-B), compared to the AP stored in the plasma for blood groups A, B and O. As predicted, the lower antibody titres in the AP stored in PAS were due to the dilutional effect of 65% replacement of plasma with PAS.
The PLT transfusions are commonly indicated for the prevention and treatment of bleeding in patients with thrombocytopenia or PLT function defects.4 Transfusion of only ABO-compatible PLTs is not always feasible due to the limited shelf-life of PLTs (5 days), limited availability at emergency and the fact that group O PLT donors outnumber the other donors.4
The PLT recovery in ABO-incompatible PLT transfusions may be impaired to some extent, however this is usually not clinically significant.8 This may be due to neutralization of Anti-A or Anti-B antibodies by recipient soluble A and B antigens, along with dilution of incompatible ABO antibodies in the recipient plasma volume. However, potential risk for hemolysis exist when ABO-incompatible units containing high-titre Anti-A and Anti-B antibodies are transfused and the risk is even greater when group O PLTS are transfused out of group in small children. There are considerable differences in the definition of “high titre” in PLT units between centers, but many consider titres, such as 64–128, as critical.4,8
In addition, transfusing ABO-incompatible plasma also leads to the formation of immune complexes which bind and activate the complement and which then bind to platelets, leading to phagocytosis by monocytes/macrophages, carrying unknown potential for morbidity (e.g., proinflammatory predisposition for multi-organ failure and death in cardiac surgery).9
There is no uniform definition of what is considered a safe threshold titre level for ABO-incompatible PLT transfusion. Also, antibody titres do not predict hemolysis in a consistent manner, hence many centers reduce the plasma volume of platelets, not to exceed 100 ml of incompatible plasma.3–5 The AABB standards mention that the blood center should have a policy concerning transfusion of components containing a significant amount of incompatible ABO antibodies.4
As there is no universally accepted standard method or definition for “high titre”, the prevalence varies between the centers. The Finnish Red Cross Blood service observed anti-A and anti-B titres from 139 blood group O platelet apheresis donors by using the direct agglutination method in tubes.9 The median anti-A or anti-B titre ranged from 8 to 16. Only 5.7% of the donors had a titre of >32 and none had a titre of >128.9 Similarly, Harm et al., observed the high titre rate in group A apheresis PLTs between 2.7–9.3% and in group O, 2.3–65.7%.7 In the present study, the maximum Anti-A and Anti-B titre in the plasma group was 256 for both, whereas in the PAS group, the maximum Anti-A and Anti-B titres were 32 and 64, respectively. We observed, relatively higher number of donors with an antibody titre >64 (10% of Group B and 8.8% of Group A) at baseline. None of the PLT units suspended in PAS had an antibody titre >64, while in contrast, 4 out of 60 units suspended in plasma had an antibody titre >64.
Few studies have shown Anti-B levels higher than those of Anti-A among PLTs suspended in plasma in routine blood donors.6,10 Bazigou et al. observed a level of Anti-A greater than that of Anti-B in plasma stored platelets among Group O plateletpheresis donors.4 This was in agreement with the incidence of hemolytic transfusion reaction due to passively transferred Anti-A than Anti-B as described in literature.5 The present study observed the Anti-A antibody level to be significantly lower in Group II (PAS) than in Group I (Plasma). However, despite reduction in Anti-B titre levels among groups A and O units between Group II (PAS) over Group I (Plasma), the difference was not significant. (Figure 1) With reports of fatal acute hemolytic transfusion reaction due to the transfusion of the Anti-B antibody in the PAS-stored AP, Anti-B levels also needs to be monitored in incompatible transfusions.5
Pagano et al. studied both IgM and IgG levels in the PAS units. They observed a 65% reduction in mean IgM anti-A and anti-B titres for group O PAS, compared to the donor sample, while for IgG, the reduction was 64% in anti-A and 69% in anti-B levels. Similarly for the non-group O PAS, the IgM (anti-A and anti-B) and IgG (anti-A and anti-B) were 62% and 66% lower than the donor mean, respectively.11 From this, it is evident that the reduction of anti-A and anti-B titres of the IgG class would be the same as that observed for the IgM class, so the reduction of IgM titre may be a reliable marker of titre reduction.
There was an overall two-fold reduction in the IgM ABO antibody levels between peripheral blood of donor and their AP suspended in the PAS. This was comparable with Weisberg et al., with a two-fold reduction in median anti-A and four-fold reductions in median anti-B antibody titres in the O group units after addition of PAS.12 Similarly Jain P et al. had reduction in titres levels in units with titre ≥128 to 16 with the PAS substitution, with their geometric mean titre for anti-A and anti-B reducing to 33.8 and 36.1, respectively.13
As majority of the previous publications studied ABO antibody levels in Group O donors, the present study correlates antibody tires between donor samples and the PAS-stored platelets among all three blood groups A, B and O. A strong positive correlation was observed with the reduction in antibody titre between AP suspended in the PAS (Group II) and donor samples in each blood group A, B and O (p-value = 0.00). Likewise, the present study utilizes regression analysis and showed that the level of reduction of the antibody titres is well explained by baseline donor antibody titres in Blood groups A and B, compared to Blood group O (Figure 2).
The use of PAS to store the AP actually reduces the plasma, similar to volume-reduced platelets with reduced risks of hemolytic and allergic reactions.11 A Danish study observed the titres of Anti-A or Anti-B remained stable and there are no large variations in the rate of occurrence in high titre units over time in repeat donors.14 Hence, identifying donors with high titres and the routine use of PAS in such donor units might reduce the risk of hemolytic reactions. The age of the donor population was not analyzed and, as increased age can present a lowered antibody titre level, constitutes one of the limitations in this study.
Overall, the implementation of the PAS-stored platelets is an effective strategy to reduce the ABO-incompatible antibody levels and provides a better inventory management, thereby limiting the wastage of units for want of ABO-compatible AP.
ConclusionThe risk of hemolysis due to passively transfused anti-A and anti-B is small but present and hence, apheresis platelets suspended in the PAS should be considered when a large volume of incompatible plasma is transfused. Addition of the PAS to store apheresis platelets reduces IgM ABO antibody titre levels by two-fold, compared to apheresis platelets suspended in plasma.
Ethical approvalBeing a retrospective study, the Institutional Review Board (IRB) approved the present study without ethical approval through Ref. No: 1616/1RB-SRC/13/MCC/30-5-2019/3, dated July 2, 2019.
Conflicts of interestThe author declares no conflicts of interest.