Autoimmune hemolytic anemia (AIHA) is a condition in which self-antibodies bound to antigens on the membranes of red blood cells initiate their destruction (hemolysis) via the complement and reticuloendothelial systems. Multiple myeloma (MM), on the other hand, is characterized by a clonal expansion of plasma cells in bone marrow, causing bone tissue destruction, renal failure and hematopoietic suppression. Although the association of MM and anemia is common, AIHA as the anemic manifestation of MM is rare.1
Case reportHerein we report on the case of a 69-year-old, black patient under treatment with prednisone and methotrexate for rheumatoid arthritis over the ten years leading up to this report. Six years ago, the patient was investigated by the hematology department due to an unstable leukopenia (2.86×103/μL), without the involvement of any other series. Since the beginning of treatment for rheumatoid arthritis, the leukocyte count of the patient was controlled, with variations being attributed to the rheumatoid arthritis itself.
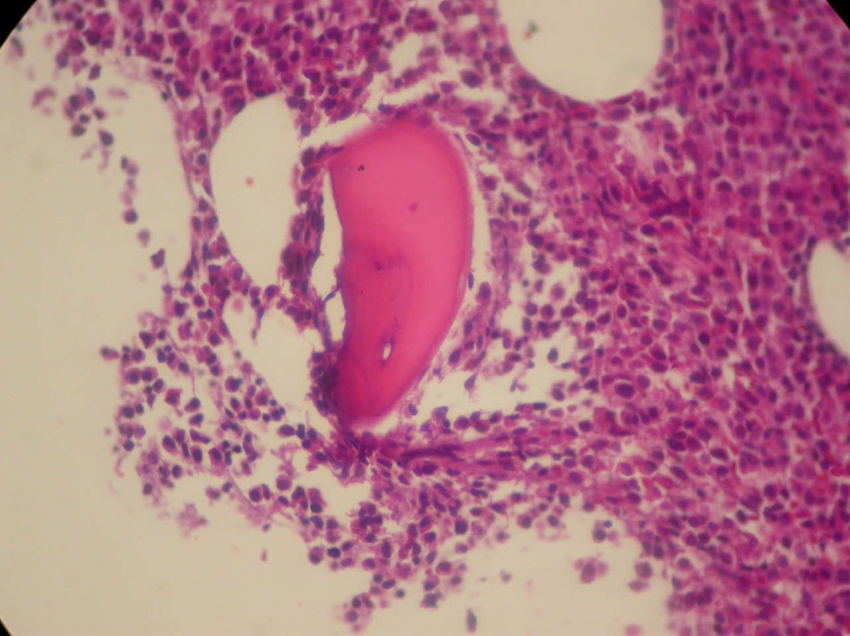
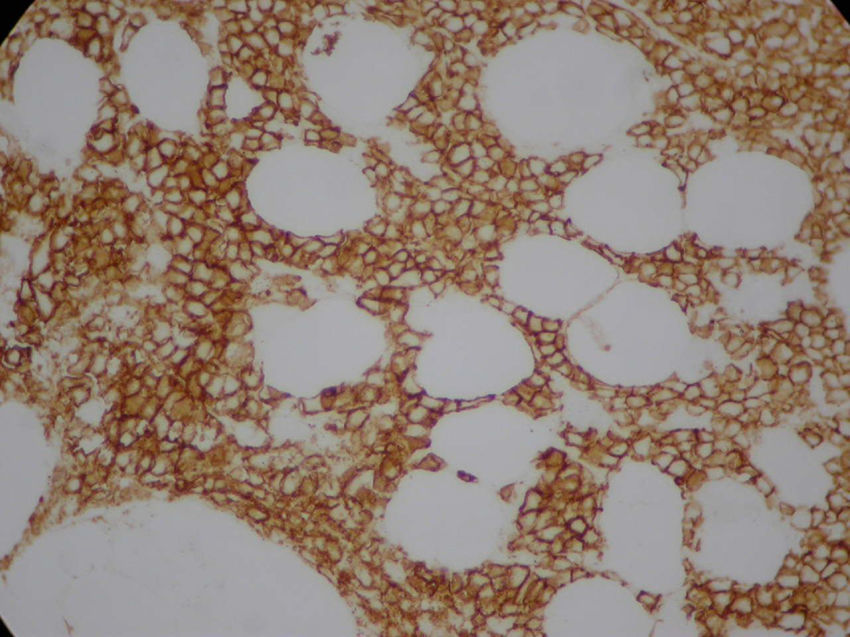
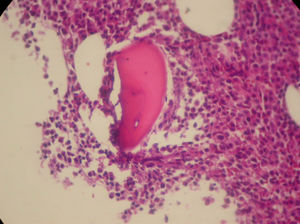
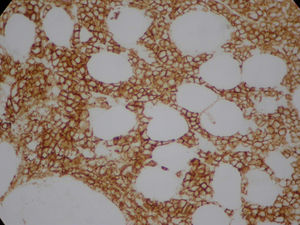
However, other alterations were found during a routine appointment in the Rheumatology Department including anemia (hemoglobin: 7.2g/dL), low hematocrit (22.6%), high ferritin levels (732mg/dL), positive direct coombs test, and elevated total and indirect bilirubin. By protein electrophoresis, the total protein was elevated (11.8g/dL), the albumin/globulin ratio was low (0.50), the albumin was low (3.94g/dL) and the gamma globulin was high (6.25g/dL) with a monoclonal component. The patient was referred back to the hematology department and diagnosed with hypergammaglobulinemia and AIHA at which time a bone marrow biopsy was performed that identified MM (Figures 1 and 2).
Normocytic and normochromic anemia, with multifactorial origin, such as a red cell series maturation disorder, iron deficiency, decreased erythropoietin response or erythropoietin deficiency, is a frequent finding in patients with MM.2 AIHA is often associated with B cell lymphoproliferative disorders. It can be observed in approximately 8–15% of patients with chronic lymphocytic leukemia (CLL),3 as well as in other pathologies such as non-Hodgkin lymphoma including Waldenstrom's macroglobulinemia,4 but its connection with MM has not yet been well elucidated. A review by Pirofsky 40 years ago showed that only 4% of AIHA cases were due to MM.5 There are less than a dozen reported cases,6 with none being Brazilian, but recently a prospective study was carried out that showed that 10.6% of patients with MM had their pathology complicated by AHAI.4 Despite this, an acceptable conclusion has not yet been reached about the pathogenesis that relates these two conditions. The fact that MM is a B cell disease, similar to CLL, which is more associated with AHAI, is being taken into account to conduct some studies.7 One of the hypotheses is the development of autoantibody-producing clones against the surface antigens of red blood cells, originating from the significant immune disorder caused by MM.7 However, no study has been able to prove that the monoclonal protein, of which very high levels are seen in MM, is the antibody responsible for AHAI and the pathogenesis of this progression is still unclear.8 Moreover, due to the lack of concrete data, the possibility of this pathogenesis, that is, AHAI as the cause of MM cannot be ruled out.8 The involvement of immunosuppressants, such as interferon-alpha, which are used in the treatment of MM and other lymphoproliferative disorders, may also play an important role in the development of AHAI, an autoimmune phenomenon similar to Evans-like syndrome.9 The number of reported cases is extremely low, which restricts the progress of research.
ConclusionThis case describes a rare condition, AIHA associated with MM. The low number of reported cases and consequently the few studies on this association hinders our understanding. However, ongoing studies should clarify both the pathogenesis and the intimacy of the relationship between the two entities in the future, thereby allowing earlier diagnosis and treatment that is more effective. The medical community should consider the diagnosis of AHAI in the presence of MM as well as vice versa, in order to make earlier diagnoses and treatments that are more effective. In addition, new cases need to be reported to support research related to these two pathologies, so that through a larger analysis, science can reach a coherent and effective conclusion.
Conflicts of interestThe authors declare no conflicts of interest.