A 66-year-old man presented with hematuria. On admission, laboratory test revealed: hemoglobin 132 g/L, leukocytes 15.3 ×109/L, platelets 41 ×109/L, fibrinogen 0,97 g/L (normal range 1.8–4.0 g/L), prothrombin ratio 1.46 (0.8-1.2), D-dimer 26,300ng/mL (<500 ng/mL) and lactate dehydrogenase 4234 U/L (26-245). Peripheral blood smear showed atypical monocytoid cells and 2% of blast cells. With suspicion of acute promyelocytic leukaemia, we started all-transretinoic acid (ATRA) treatment.
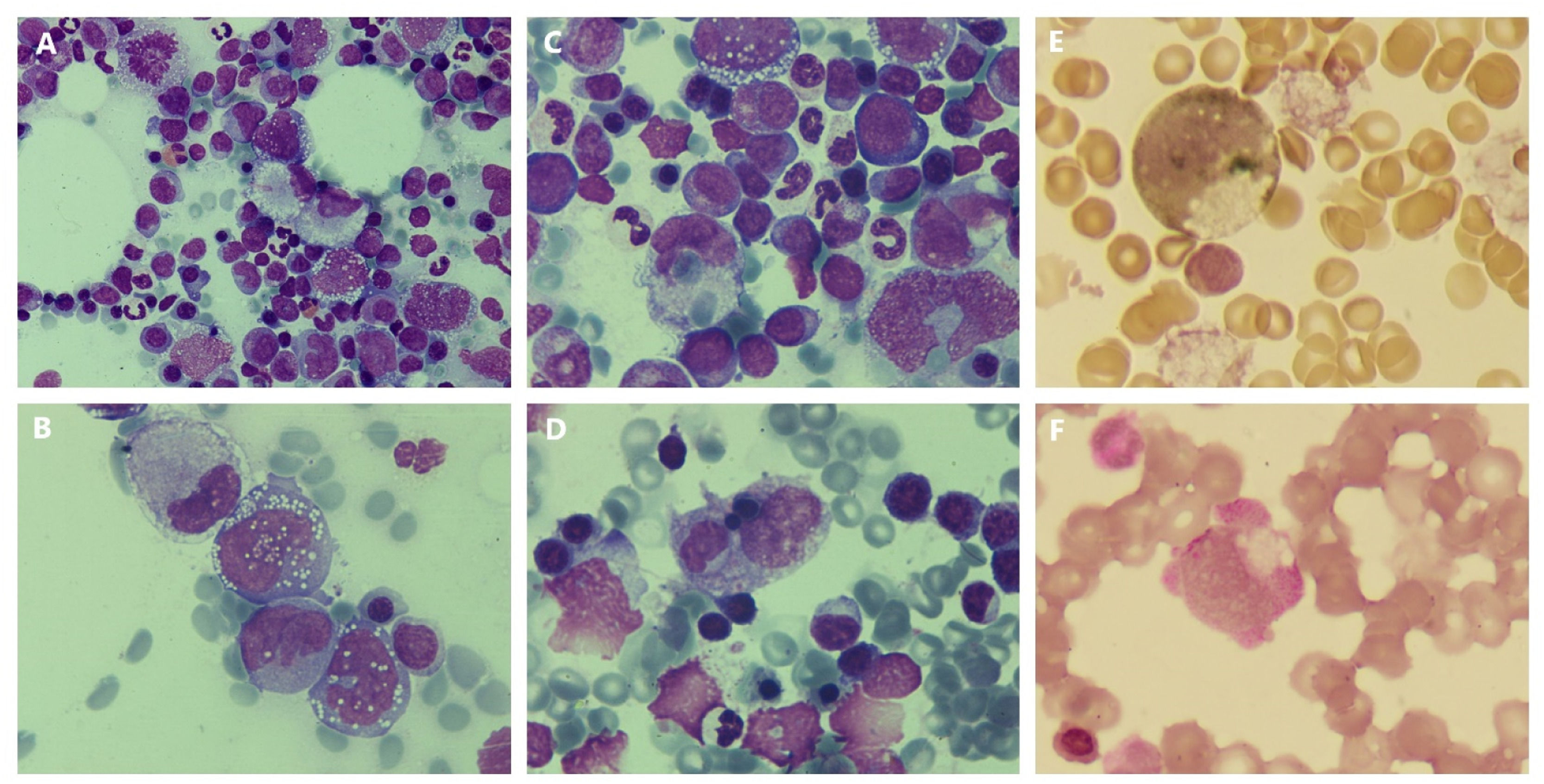
Bone marrow aspirate showed a hypercellular marrow with a heterogeneous blast population: large cells with fine chromatin and irregular basophilic cytoplasm with vacuoles; large cells with foamy cytoplasm, which where compatible with histiocytes; medium size blastic cells including promonocytes and mature monocytes (Figure 1A-B). Figures of mitosis and erythrophagocytosis by leukemic blasts were frequently observed (Figures 1C-D). Cytochemical staining with alpha-naphthyl acetate esterase activity (Figure 1E) and periodic acid-Schiff (Figure 1F) were positive and myeloperoxidase (MPO) was negative. Immunophenotype showed an increase in monocytic population (CD33+,CD13+,CD11b+,CD4+, HLADR+) without aberrancies (CD2-,CD7-,CD56-) and with predominance of mature monocytes (71% CD14++). Bone marrow biopsy was done to confirm the suspicion of a histiocytic component. Pathological analysis showed a massive infiltration by CD68, CD163, CD4, CD15 and lisozyme positive cells, confirming the diagnosis of acute monocytic leukemia. Cytogenetic analysis displayed a normal karyotype and nested RT-PCR to dismiss KAT6A-CREBBP rearrangement was negative.
(A) Hypercellular bone marrow with heterogeneous blast population (May-Grünwald Giemsa x50 objective). (B) Heterogeneity of blasts (MGG x100 objective). (C and D) Phagocytosis by blasts with histiocytic morphology (MGG x100). (E) Large blast with histiocytic morphology positive to alpha-naphthyl acetate esterase (x100 objective). (F) Blast with histiocytic features positive to periodic acid-Schiff (x100 objective).
With these results, we stopped ATRA and we began cytarabine and idarubicin induction chemotherapy but the disease was refractory to induction and also to other salvage treatments. Finally, the patient received azacitidine achieving complete response with ulterior consolidation with a haploidentical hematopoietic stem cell transplantation and remains alive two years after the procedure.
Erythrophagocytosis by leukemic blasts is an extremely rare phenomenon that could be seen in leukemias with monocytic differentiation with rearrangements involving KAT6A gene and sometimes this leukaemia due its clinical course is confused with acute promyelocitic leukemia.1 Hemophagocytosis has also been described in leukemias with histiocytic morphology.2-4
Leukemia with histiocytic differentiation is an unusual morphologic variant of acute monocytic leukemia. The phenotypic markers of these leukemias are CD68, CD11b, CD11c, CD14, CD4, and lysozyme.2,5
This case emphasizes, the importance of integrated diagnosis, were the morphology as well as the cytochemistry continue having a crucial role in the diagnosis of malignant hemopathies.