Newborn infants are the most heavily transfused population inside intensive care units. The hemoglobin level used to indicate the need of transfusions is not well established. The aim of this study was to evaluate transfusional practices in newborns in the neonatal intensive care units of one specific city.
MethodsRed blood cell transfusion practices of all transfused newborns in all five of the neonatal intensive care units of the city were analyzed. Data are reported as descriptive statistics, including numbers and percentages and means and standard deviation. Univariate analysis, followed by stepwise logistic regression was performed in respect to transfusional data and outcomes.
ResultsA total of 949 patients were admitted to the intensive care units during the 12-month study period with 20.9% receiving at least one transfusion, most (62.4%) of whom received more than one transfusion. The mean number of transfusions per infant was 2.7±2.16; in the liberal transfusion group the mean number was 1.59±1.63 and in the restrictive group it was 1.08±1.51. The mean hemoglobin and hematocrit levels were 9.0g/dL (±1.4g/dL) and 27.4% (±4.3%), respectively. The most common indications for blood transfusions were sepsis and prematurity.
ConclusionThis study shows that the characteristics and the transfusion practices for newborns admitted in the neonatal intensive care units of Juiz de Fora are similar to recent pubications. There was no significant reduction in the number of transfusions per child in the restrictive group compared to the liberal group. Restrictive transfusions are an independent risk factor for peri-intraventricular hemorrhages and death.
According to data for 2011 of the Brazilian National Health Service (SUS), very low birth weight newborns represent 32.0% of all childhood mortality. Cross-sectional studies show that they are the most transfused age group in tertiary care facilities. Forty-five to 85% of premature newborns in a neonatal intensive care unit (NICU) receive at least one blood transfusion during hospital stay, making them the population group that is most at risk to transfusion-related adverse effects and complications.1–6
The fast growth of the newborn infant, the erythropoietin and iron deficiency inherent to this age group, the low erythropoiesis, the shorter life span of fetal hemoglobin, the oxidative hemolysis that occurs due to sepsis and, especially, iatrogenic loss due to frequent blood sampling are the main factors contributing to the need to transfuse.2,7
Despite being a widely used practice, there is still a lack of scientific evidence in regards to the decision of when to transfuse RBCs. Each day more evidence appears about the association of RBC transfusions with morbidity and mortality in the newborn infant, such as changes in cellular immune response, especially T-cell mediated response, necrotizing enterocolitis, retinopathy of the premature infant, bronchopulmonary dysplasia, intraventricular hemorrhage and even death.7–16
The number of papers addressing this issue is increasing with an attempt to compare liberal and restrictive transfusion practices, in order to reduce the frequency of transfusions and, consequently, the occurrence of adverse effects.7,17–19 For this, authors are trying to find clinical variables that may be correlated to the need of RBC transfusions in the neonatal population, as well as risk factors and adverse effects associated with transfusion procedures.5–7
Thus, the aim of this study was to gain knowledge on transfusional practices in the NICUs of the city of Juiz de Fora by evaluating the clinical and transfusional characteristics related to this procedure.
MethodsStudy designA cross-sectional study was performed between January 1st and July 31st 2011 and January 1st and July 31st 2012. All medical records of newborn infants that received RBC transfusions in all five NICUs of the city were reviewed.
The study was submitted to and approved by the Ethics Committee of the Universidade Federal de Juiz de Fora (# 337/2011).
All studied NICUs are referral centers for high-risk pregnancy. Two only provide care for National Healthcare Service patients, two only accept private health insurance patients and the other provides care for both systems. The five units have a total of 70 beds.
The following data were gathered from patient's medical records by filling in a questionnaire designed for this study: number of births in each center, maternal, neonatal, clinical and demographic characteristics of each case, number of newborn infants that received at least one in-hospital RBC transfusion, number of RBC transfusions that were performed on Days 1–14, Days 15–28 and after Day 28 of hospital stay until hospital discharge, volume of blood transfused, volume of blood drawn for laboratory tests, hemoglobin and hematocrit levels before transfusion and the indication that led to the need of transfusion.
Patient populationAll newborn infants that were admitted to one of the five NICUs and that received at least one RBC transfusion were included in this study. However, infants with the following conditions were excluded: death within the first 24h. after birth, newborns submitted to an exchange transfusion protocol, hemolytic disease of any etiology and major congenital anomalies.
Data collectionStatistical analysis was performed using data derived from the research protocol, with the aim of identifying clinical conditions related to RBC transfusions within the target population. Demographic and clinical variables were reported as descriptive statistics. Continuous variables were described by means and standard deviation and categorical variables as numbers and percentages, as appropriate.
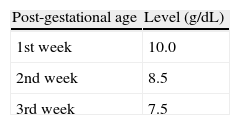
Cut-off hemoglobin levels, believed to be safe for transfusions, were established to evaluate transfusional practices based on the 2011 Cochrane Database for Systematic Reviews (Table 1).18 Infants receiving transfusions when their hemoglobin was above the cut-off level were allocated to the liberal group and those receiving transfusions when their hemoglobin was below the cut-off level were allocated to the restrictive group. The mean numbers of transfusions per newborn in each group were calculated.
Univariate analysis was then performed comparing the liberal and restrictive groups in respect to transfusion variables (mean hemoglobin level, mean hematocrit level, mean number of transfusions per infant) and relevant neonatal outcomes (mechanical ventilation, intra-ventricular hemorrhage, bronchopulmonary dysplasia, necrotizing enterocolitis, retinopathy of the premature and death). Correlations were identified using the chi-square test for categorical variables and t-test for continuous variables. Statistically relevant variables were submitted to a stepwise logistic regression model to show which transfusional variables are independently related to these outcomes.
Data analysis was performed using the Statistical Package for Social Sciences computer software (version 15.0) for Windows (SPSS, Inc., Chicago, IL). Differences were considered significant when p-values were less than 0.05.
ResultsDuring the study period, 949 newborn infants were admitted into the five NICUs of the city. Of these, 200 received RBC transfusions. Fifty-four newborn infants were excluded from the study: one because of hemolytic disease, five were submitted to exchange transfusion, five were syndromic patients (3 Down Syndromes and 2 Edwards Syndrome), 42 had major congenital anomalies (4 severe congenital heart defects, 29 congenital gastro-intestinal abnormalities, 4 myelomeningoceles and 5 others), and one was considered an outlier (169 days of hospital stay, 21 RBC transfusions, birth weight 500 grams and 24 weeks gestational age). The medical records of 13 patients were not found or incomplete, which represents a loss to study of 9.0%. Therefore, 133 met the inclusion criteria and were analyzed in this study. The mean gestational age was 30.3 weeks (range: 23–40 weeks) and the mean birth weight was 1424.5±677.7g (range: 386–3620g).
Analysis of the maternal characteristics showed that the deliveries of 87 (65.4%) newborn infants were by cesarean section, seven (5.2%) mothers had diabetes, 31 (23.3%) has hypertension, 55 (41.3%) received antenatal corticosteroids and 15 (11.2%) had a history of premature (over 18h) rupture of the membrane. Ninety-four infants (74.4%) were born in the National Healthcare System. Seventy-four were male (55.6%) and 56 were female (42.1%). Three Medical Records did not report the gender of the newborn infant.
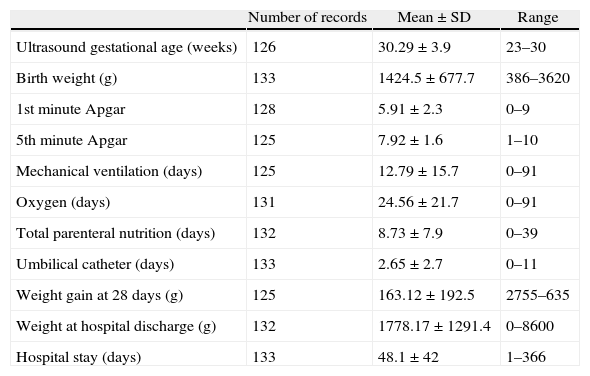
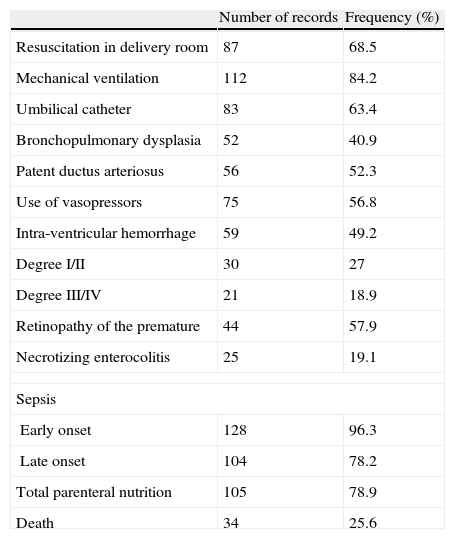
The clinical characteristics and complications of the newborn infants are shown in Tables 2 and 3.
Clinical data of the newborn infants.
| Number of records | Mean±SD | Range | |
| Ultrasound gestational age (weeks) | 126 | 30.29±3.9 | 23–30 |
| Birth weight (g) | 133 | 1424.5±677.7 | 386–3620 |
| 1st minute Apgar | 128 | 5.91±2.3 | 0–9 |
| 5th minute Apgar | 125 | 7.92±1.6 | 1–10 |
| Mechanical ventilation (days) | 125 | 12.79±15.7 | 0–91 |
| Oxygen (days) | 131 | 24.56±21.7 | 0–91 |
| Total parenteral nutrition (days) | 132 | 8.73±7.9 | 0–39 |
| Umbilical catheter (days) | 133 | 2.65±2.7 | 0–11 |
| Weight gain at 28 days (g) | 125 | 163.12±192.5 | 2755–635 |
| Weight at hospital discharge (g) | 132 | 1778.17±1291.4 | 0–8600 |
| Hospital stay (days) | 133 | 48.1±42 | 1–366 |
Data were missing from some patient records.
Complications of the newborn infants.
| Number of records | Frequency (%) | |
| Resuscitation in delivery room | 87 | 68.5 |
| Mechanical ventilation | 112 | 84.2 |
| Umbilical catheter | 83 | 63.4 |
| Bronchopulmonary dysplasia | 52 | 40.9 |
| Patent ductus arteriosus | 56 | 52.3 |
| Use of vasopressors | 75 | 56.8 |
| Intra-ventricular hemorrhage | 59 | 49.2 |
| Degree I/II | 30 | 27 |
| Degree III/IV | 21 | 18.9 |
| Retinopathy of the premature | 44 | 57.9 |
| Necrotizing enterocolitis | 25 | 19.1 |
| Sepsis | ||
| Early onset | 128 | 96.3 |
| Late onset | 104 | 78.2 |
| Total parenteral nutrition | 105 | 78.9 |
| Death | 34 | 25.6 |
Data were missing from some patient records.
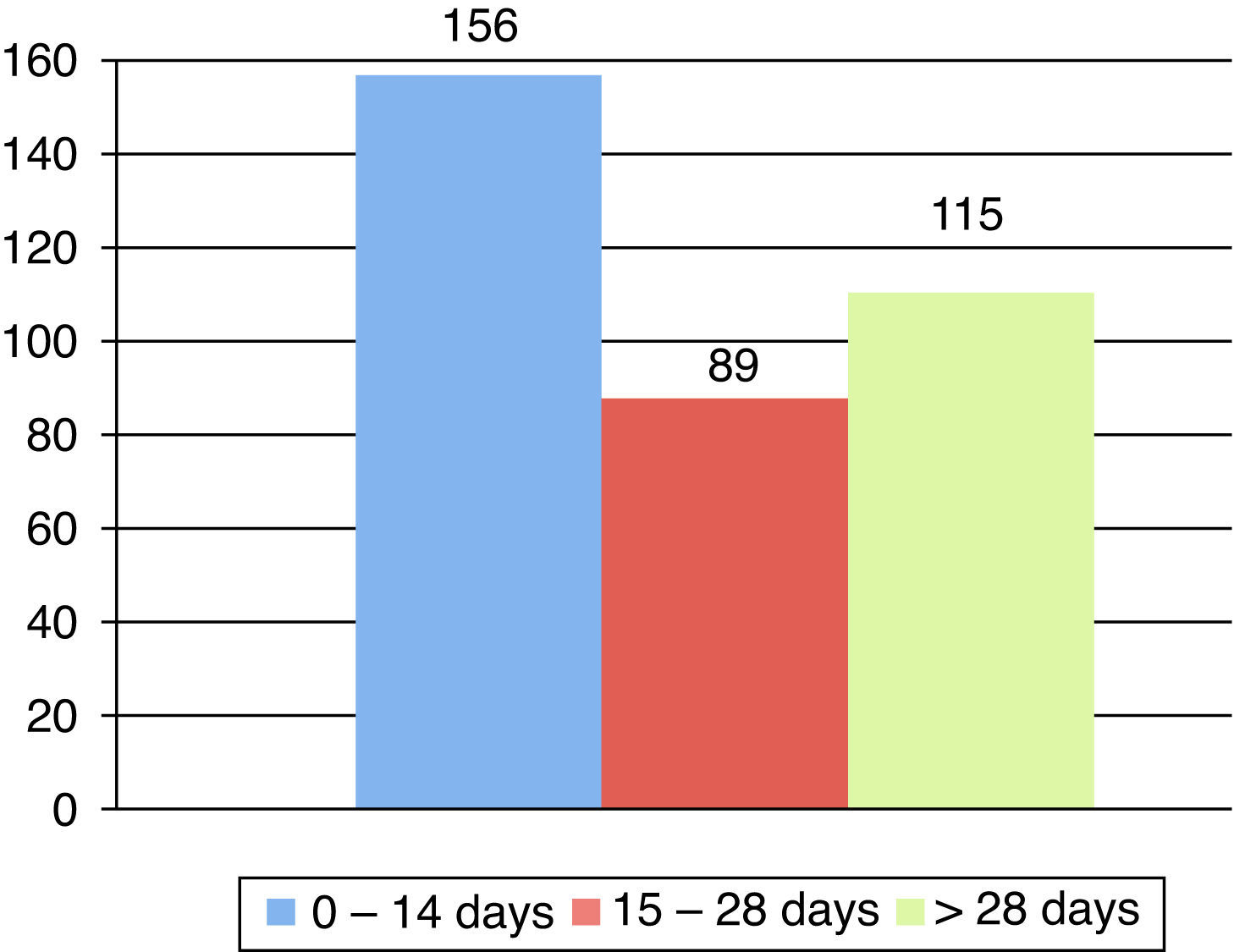
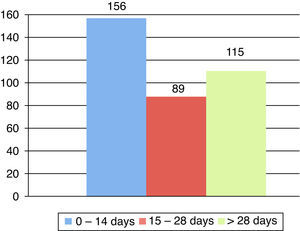
The incidence of transfusions over the studied period was 20.9%. Fifty (37.6%) newborn infants received one transfusion and 83 (62.4%) newborn infants received more than one. Figure 1 shows the distribution of the number of transfusions in the first 14 days of life, 14–28 days and after 28 days until hospital discharge. The mean number of transfusions per newborn during the period was 2.71 (±2.162) and the mean volume transfused was 20mL/kg. The mean hemoglobin and hematocrit levels were 9.0g/dL (±1.4g/dL) and 27.4% (±4.3%), respectively. The mean number of transfusions per newborn in the liberal group was 1.59 (±1.63) and in the restrictive group it was 1.08 (±1.51).
After the final logistic regression model using the transfusion variables (pre-transfusion hemoglobin and hematocrit levels, mean number of transfusions per newborn in the liberal and restrictive groups), the only characteristic that proved to be an independent risk for any of the outcomes was restrictive transfusions. This is a risk factor for the following outcomes: intra-ventricular hemorrhage (ODDs ratio: 2.04; 95% confidence interval: 1.05–3.95; p-value=0.033) and death (ODDs ratio: 2.57; 95% confidence interval: 1.30–5.09; p-value=0.007).
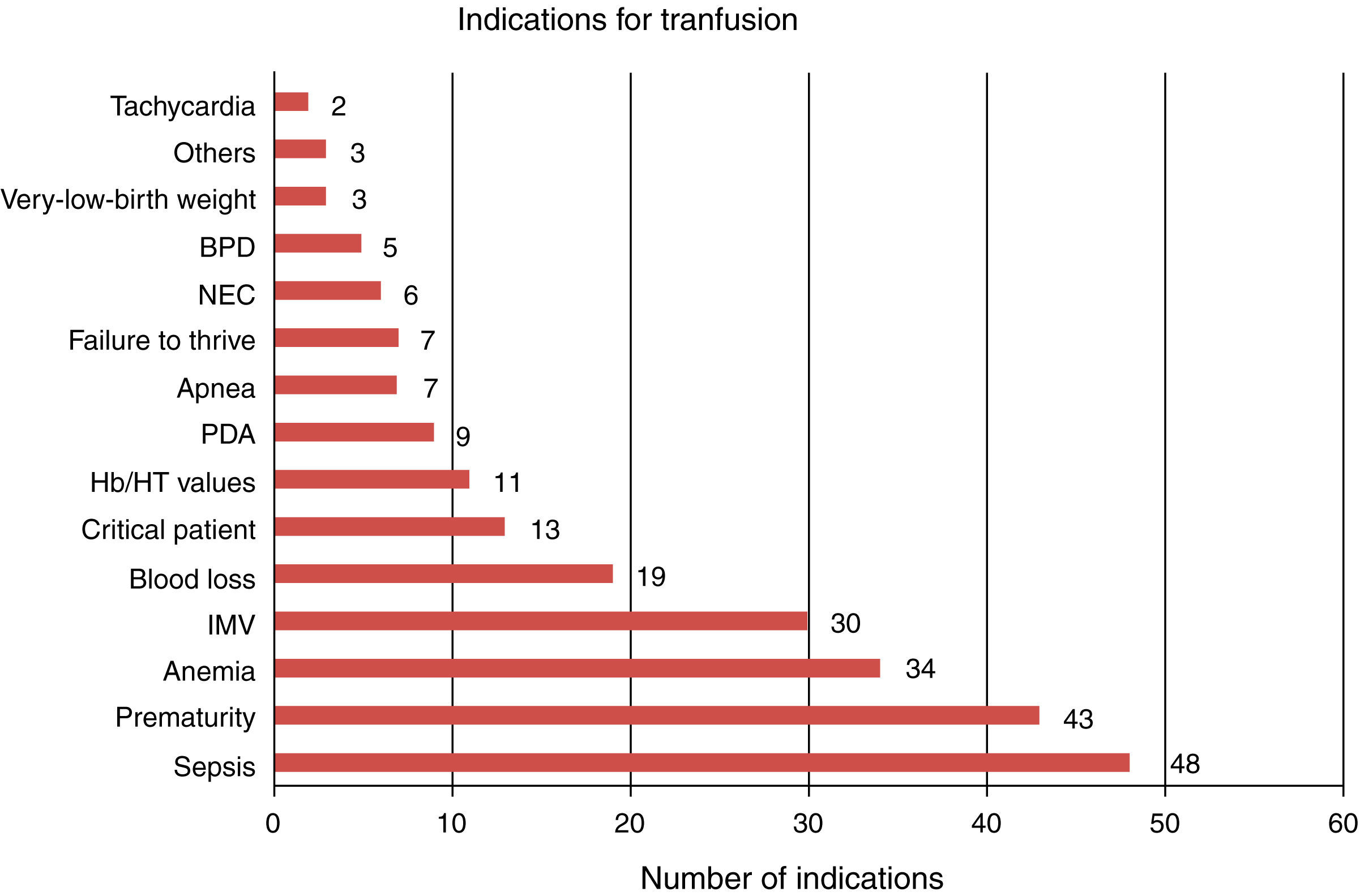
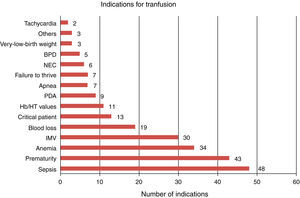
Figure 2 shows the most reported indications of the need of red blood cell transfusions as prescribed by the physicians. The most frequent causes were sepsis, prematurity and anemia.
DiscussionTransfusional therapy is a common procedure in the NICU. However, transfusional data in NICUs are not well known. On considering recent publications describing the many transfusion complications, the importance of a better understanding the risk factors becomes more apparent.
The choice of clinical and demographic data reported in this study was based on the main factors described as risk factors in the target population in the literature.3,6
The maternal and neonatal data that characterize the population of this study are similar to data found in literature.3–6,20–23 Differences found could be explained by the fact that most papers only include very low birth weight newborns.3–6,20–23 The incidence of transfusions found in this study is much lower than what was found in previous reports (55.9% in Santos et al.6; 85.0% in Fabres et al.3), probably due to this same reason.
Over half of the infants received more than one transfusion during their hospital stay similar to what was reported by dos Santos et al.6 However, it was lower than the results of her most recent publication.7 The distribution of the transfusions in this study stratified by age group was similar when compared to these works6,7; the highest incidence of transfusions was in the first 14 days of life followed by after 28 days of age, probably due to late complications, especially in the extremely premature newborn infant group.5,6
This study found a lower mean number of transfusions per newborn than what is reported in literature,4,6,20–23 with the exception of the report by Freitas and Fanceschini.5 In the liberal group of two clinical trials20,22 the mean number of transfusions per infant was more than twice the mean number found in the current study.
The fact that there were no significant differences between the number of transfusions in the liberal group and the number of transfusions in the restrictive group shows that the decision to transfuse using restrictive criteria does not reduce the number of transfusions per infant.
It is worth noting that the level used to categorize patients between liberal and restrictive transfusional regimens was the cut-off considered safe for newborn infants not on ventilation support as reported by Robin and Haresh.18 Thus, very low cut-off levels were used which could explain the results found by logistic regression, in which the restrictive group was found to be a risk factor for intra-ventricular hemorrhage and death. Only one other report, by Bell et al.,22 found a higher incidence of degree IV intra-ventricular hemorrhages for a restrictive group. There are no other studies reporting a higher incidence of death when using restrictive transfusional regimens.4,6,20,22,23 It must also be remembered that this is a retrospective report and that there was no control group of non-transfused newborn infants. The creation of a cut-off level was an effort to get around this issue, so that it could be used as a statistical tool that would allow a comparison between two transfusional regimens.
When analyzing the most commonly reported indications of RBC transfusions by physicians, the most frequent reason was sepsis, closely followed by ‘prematurity’. Late-onset sepsis is the condition that is most associated with a need to transfuse.5,6 However, it is the authors’ impression that the term sepsis in this study is much more related to the severe condition of these newborns than to the classic meaning of sepsis itself, which would classify this indication as ‘the critical condition of the patient’ instead of ‘sepsis’ per se. Kasat, Hendricks, Muñoz and Mally24 described the most common indications for transfusion reported by physicians and nurses: desaturation episodes, tachycardia – which was the least common indication in the current study, bradycardia, pallor, apnea and sepsis.
The present study has its own limitations, as it was a retrospective study, which made it impossible to evaluate, for instance, episodes of apnea. Even so, the results give extra knowledge on the transfusional profile of newborn infants admitted in NICUs.
ConclusionThe characteristics of the transfused newborn infants in the NICUs of this study do not diverge from the literature in respect to current transfusional practices. The variability found in this practice also shows the difficulty in deciding when to transfuse during the clinical practice of the neonatologist.
There was no statistical difference in the number of transfusions per infant between the restrictive and liberal groups. The restrictive group was associated with higher risk for intra-ventricular hemorrhages and death.
Conflict of interestThe authors declare no conflicts of interest.