The existing techniques to evaluate hemostasis in clinical laboratories are not sensitive enough to detect hypercoagulable and mild hypocoagulable states. Under different experimental conditions, the thrombin generation test may meet these requirements. This technique evaluates the overall balance between procoagulant and anticoagulant forces and has provided new insights in our understanding of the coagulation cascade, as well as of the diagnosis of hypocoagulability and hypercoagulability conditions. Thrombin generated in the thrombin generation test can be quantified as platelet-rich or platelet-poor plasma using the calibrated automated thrombogram method, which monitors the cleavage of a fluorogenic substrate that is simultaneously compared to the known thrombin activity in a non-clotting plasma sample. The calibrated automated thrombogram method is an open system, in which different antibodies, proteins, enzymes and peptides can be introduced to answer specific questions regarding hemostatic processes. The thrombin generation test has great clinical potential, such as in monitoring patients taking anticoagulants and antiplatelet drugs, screening for genetic or acquired thrombotic disorders, and evaluating bleeding risk control in patients with hemophilia using bypass agents or replacement therapy. Different to conventional coagulation tests, the thrombin generation test can be used for an overall evaluation of hemostasis, the results of which can then be used to evaluate specific characteristics of hemostasis, such as prothrombin time, activated partial thromboplastin time, and levels of fibrinogen and other coagulation factors. The introduction of this method will contribute to a better understanding and evaluation of overall hemostatic processes; however, this method still requires standardization and clinical validation.
Different aspects of hemostasis can be studied using the methods that are currently available to researchers and clinical laboratories. These include coagulometry and chromogenic methods, which assess separate aspects of the hemostatic process. However, these methods do not provide an overall evaluation of hemostasis.1 The method of evaluation is chosen depending on the patient's clinical data, and may separately provide important information about primary, secondary and tertiary phases of hemostasis, in addition to natural inhibitors such as protein C (PC) protein S (PS), antithrombin (AT) and tissue factor pathway inhibitor (TFPI). Molecular methods also contribute to the investigation of hemostatic disorders, in particular, in cases of genetic resistance to activated PC (aPC), which is primarily caused by factor V Leiden and other uncommon mutations, and in cases of hyperprothrombinemia caused by the G20210A prothrombin mutation.2 Despite the diversity of laboratory methods used to evaluate hemostatic processes, none of the currently available methods is able to assess all the phases of hemostasis. Thus, the results obtained using these conventional methods are not always associated with clinical manifestations.2
Traditionally used methods have satisfactory sensitivity for moderate and severe hypocoagulability, but not for hypercoagulable or mild hypocoagulable states. Such methods only provide information about the beginning of the coagulation process, and therefore, the result of the test is not representative of the entire clot formation process, as measured using the total thrombin generation capacity.2–4 The typical coagulometric measurements, such as prothrombin time (PT) and activated partial thromboplastin time (aPTT), measure only the clotting time corresponding to the initiation phase of the coagulation process. Furthermore, the end-point of these tests occurs after the formation of only 5% of total thrombin.2,4 Therefore, PT and aPTT reflect only the initial coagulation process while the formation of thrombin and fibrin is still occurring.2,5 A greater amount of thrombin is generated during the amplification and propagation phases, resulting in an exponential increase in thrombin, which becomes inactivated by physiological anticoagulants such as alpha-2-macroglobulin, AT, PC and PS.1,2 Therefore, conventional tests do not provide information about the amplification and propagation phases of the hemostatic system.1,2
The introduction of a method able to evaluate the entire coagulation process is highly desirable, as this could better reflect bleeding and thrombotic risks. Many attempts have been made to achieve this goal, which would ideally accurately reflect all components and conditions of the hemostatic process, including platelets, coagulation factors, natural inhibitors, the endothelium and its interactions, as well as fibrinolysis and blood flow. Several authors have suggested the need to introduce in vitro methods representative of the main physiological aspects of hemostasis as a possible solution.3,6–8 Attempts to develop a method to comprehensively evaluate hemostasis began several decades ago. In 1953, MacFarlane and Biggs9 were the first to report thrombin generation in the blood using a laborious and time-consuming technique, which rendered it inapplicable for use in the clinical practice. In the same year, Pitney and Dacie10 reported the measurement of thrombin generation in plasma. Many years later, convinced of the need for a comprehensive test for the broader assessment of hemostasis, the illustrious Professor Coenraad Hemker et al. at the University of Maastricht (Netherlands)1,11 improved and semi-automated the thrombin generation technique, initially employing a chromogenic method, and later a fluorogenic method.12 This improvement contributed greatly to the successful use of this technique in numerous studies.
Due to the lack of information about global tests of thrombin generation, we present a short discussion of this technique with emphasis on the calibrated automated thrombogram® (CAT) method. In this concise review, we present methodological aspects of the thrombin generation test (TGT), the evaluation of hemostatic components under some analytical conditions, the use of the test in experimental studies, potential clinical applications as a global coagulation test, as well as its limitations and future perspectives.
Thrombin generation assays and the calibrated automated thrombogram methodThrombin is a key protein involved in the regulation of hemostatic processes; it has both procoagulant and anticoagulant properties.13 While in vivo thrombin generation can be evaluated by measuring the thrombin-antithrombin complex (TAT) and prothrombin fragments 1+2 (F1+2), ex vivo TGT aims to evaluate the endogenous capacity of the overall hemostatic potential. Therefore, while high levels of TAT and F1+2 represent the pathological activation of in vivo coagulation, ex vivo thrombin generation reflects the endogenous capacity of the hemostatic system, and can be indicative of thrombotic or hemorrhagic risk. TGT continuously measures the proteolytic activity of thrombin formed in plasma using chromogenic or fluorogenic substrates following the activation of clotting using a triggering agent, as was comprehensively shown by Lecut et al.1 The synthetic substrate, which is coupled to a chromogen or fluorophore, is selectively cleaved by thrombin, releasing the chromogen or fluorophore. The output signal is continuously measured, and is proportional to the amount of thrombin present in the reaction, the kinetics of which comprise two stages. The first, the initiation stage, corresponding to the coagulation time measured using tests such as PT and aPTT, can be inhibited by TFPI. The second, the amplification/propagation stage, is followed by a resolution phase resulting from the action of various inhibitors present in plasma, such as aPC, AT and alpha-2-macroglobulin.
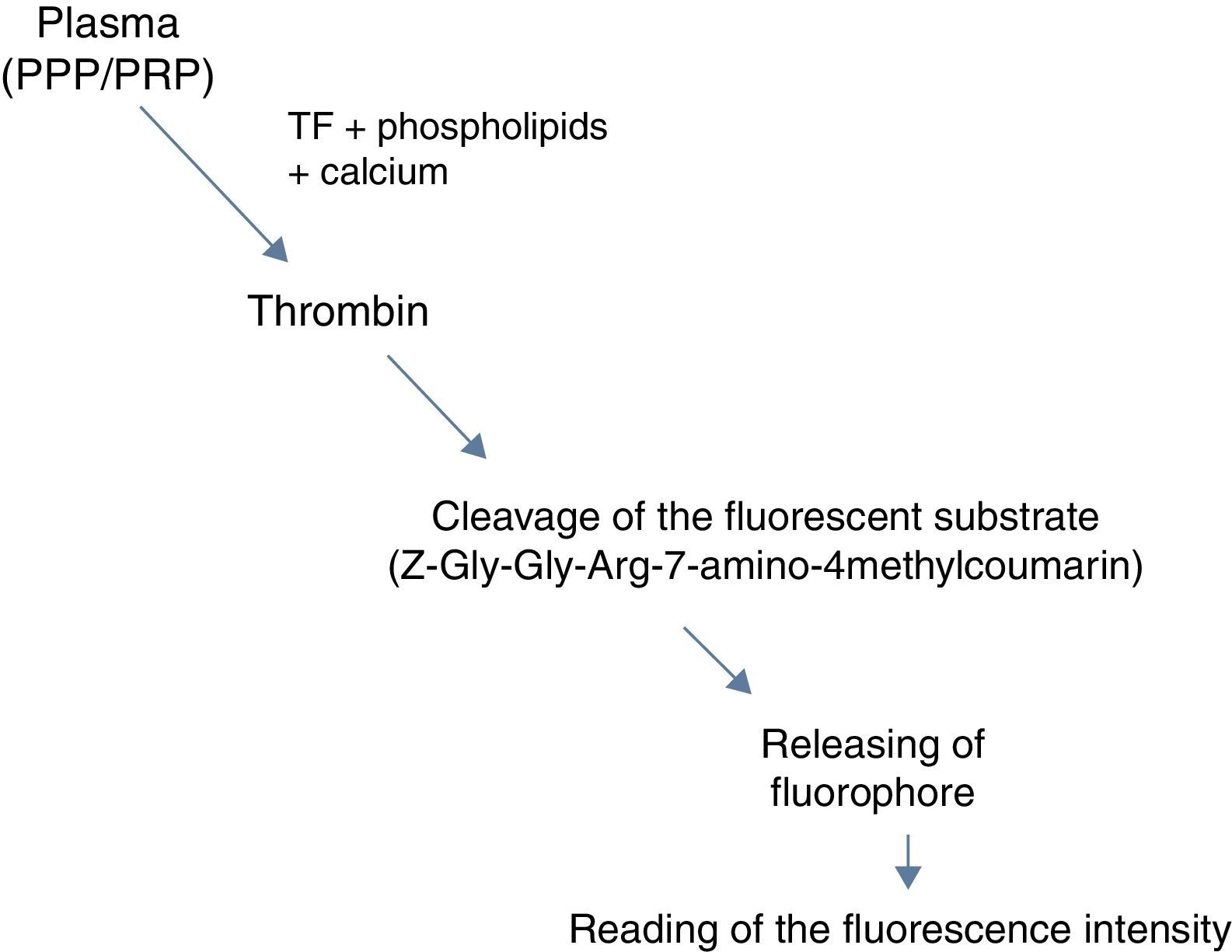
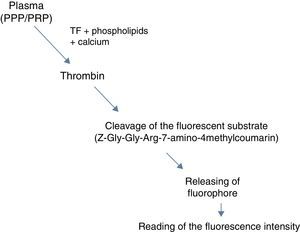
The CAT method, developed by Hemker et al.12 enables the quantification of thrombin concentrations in platelet-rich (PRP) or platelet-poor plasma (PPP) by monitoring the separation of a fluorogenic substrate, which is simultaneously compared to known thrombin activity in a non-clotting plasma sample.12 This thrombin calibrator contains a known concentration of thrombin-like enzyme linked to alpha-2-macroglobulin. The thrombin-like enzyme is not inhibited by plasma components, and reacts only with the fluorogenic substrate. The color of the plasma may interfere with the results, and therefore, the thrombin calibrator is continuously measured for each plasma sample. The addition of tissue factor (TF), phospholipids (amplify the effect of TF) and calcium in the plasma, results in coagulation activation and subsequent generation of thrombin. Thrombin cleaves the fluorescent substrate (Z-Gly-Gly-Arg 7-amino-4-methylcoumarin) that is added to the reaction in a later step, releasing a fluorophore whose fluorescence intensity over time is proportional to the concentration of thrombin formed (Figure 1).12,14
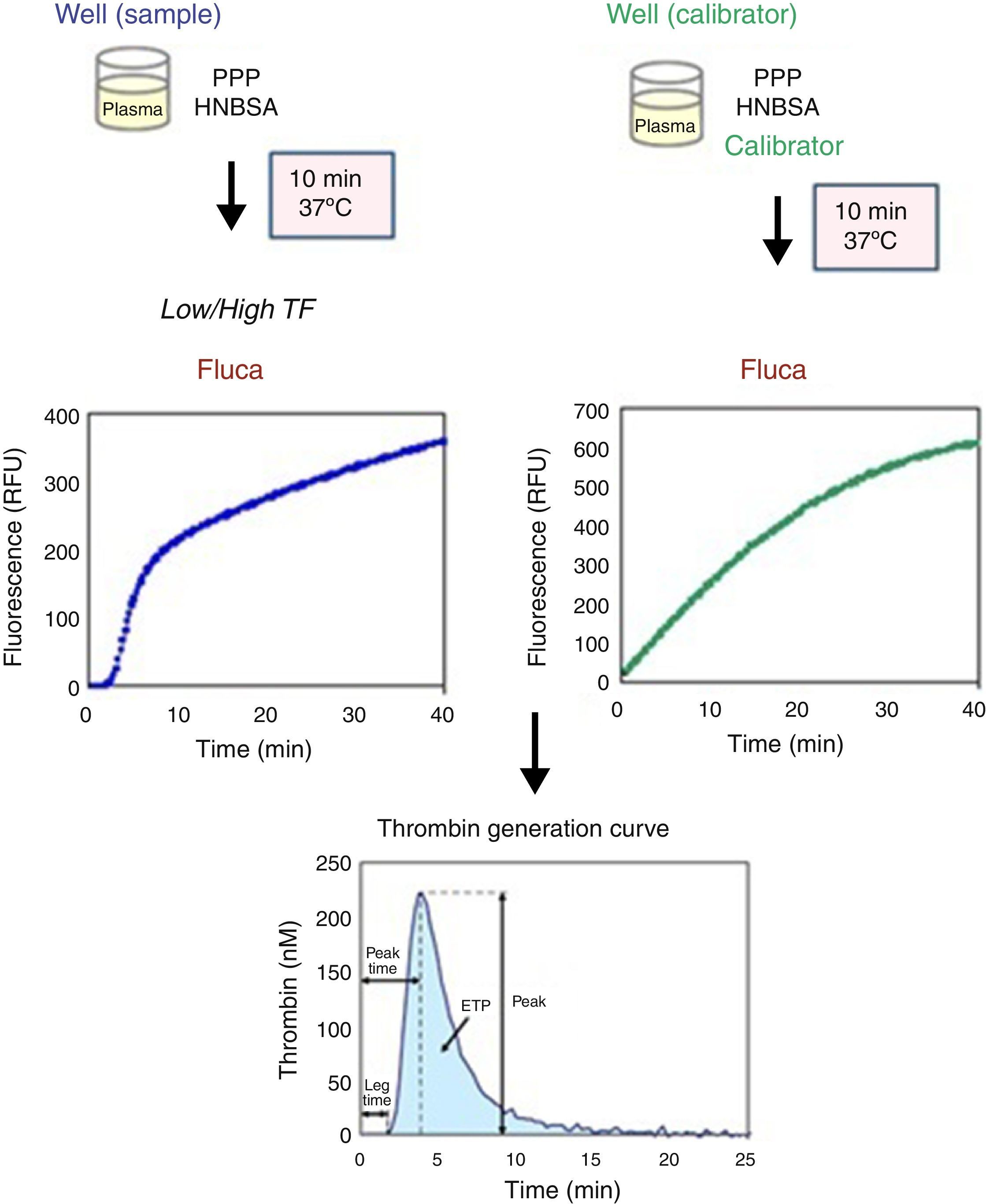
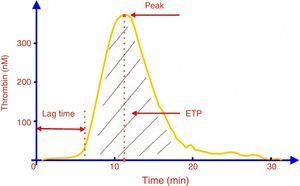
After measurements are taken in a 96-well plate using a fluorimeter (Fluoroscan, Thermo Scientific), Thrombinoscope BV software is used to convert fluorescence units (RFU) into thrombin concentrations (nM). The software also calculates thrombogram parameters such as peak and endogen thrombin potential (ETP) from the area under the curve and the peak thrombin concentration, respectively. The fluorescence intensity is converted to thrombin concentration (nM) using a reference curve prepared by measuring the conversion rate of the substrate with a known concentration of thrombin.12,14,15 Comparison of the two signals (test and calibration samples) allows a calculation of the thrombin concentration in the plasma (Figure 2).
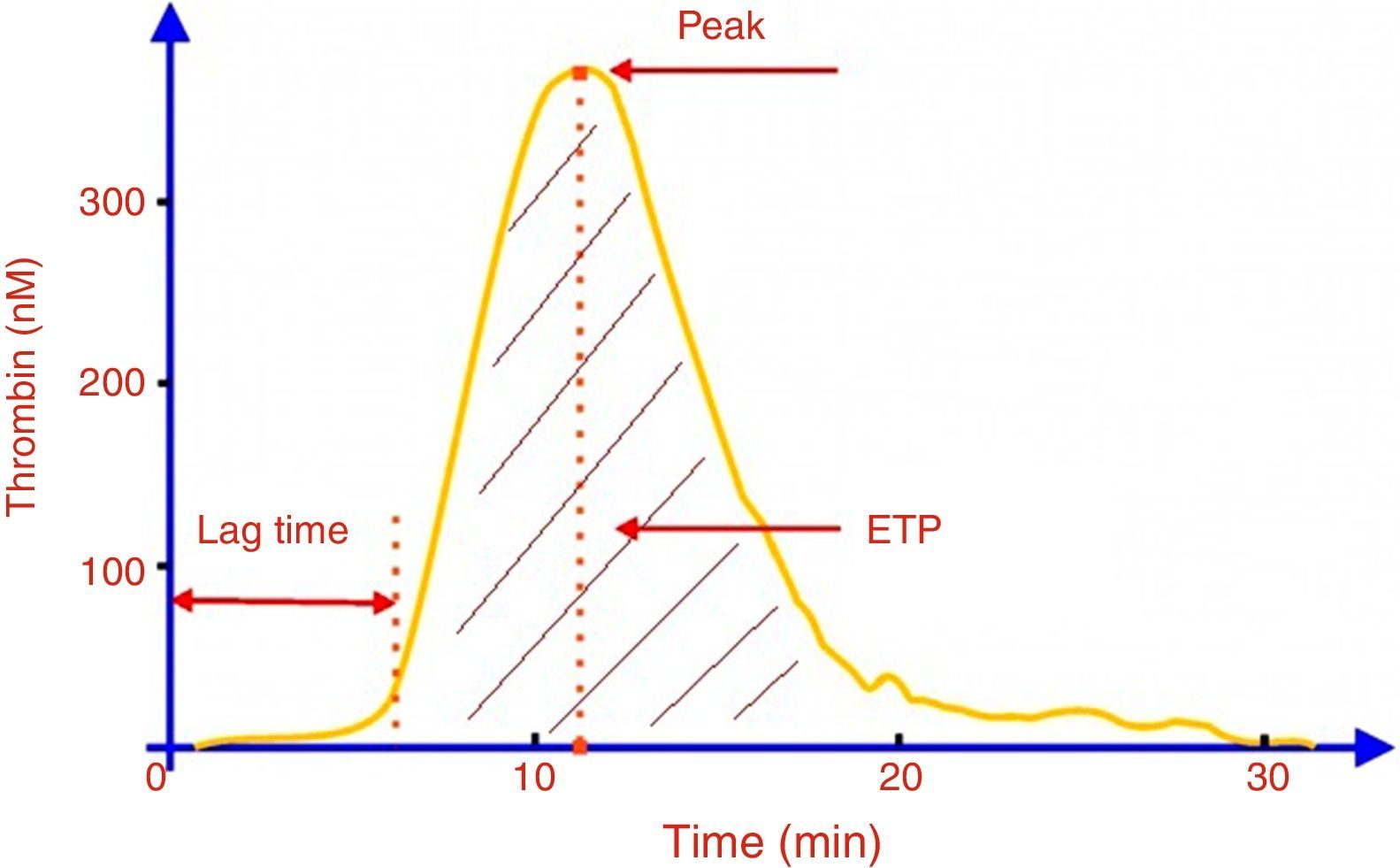
The thrombin generation curve (Figure 3) is characterized by an initiation phase (lag-time) followed by the formation of large amounts of thrombin (propagation), culminating in a peak thrombin concentration, and finally inhibition of thrombin generation by natural anticoagulants.15 The ETP (area under the curve), represents the amount of thrombin formed over 60min.11 Clot formation is known to occur at the end of the lag-time, therefore, the duration of this parameter corresponds to the clotting time.14 The coagulation state can be inferred from analysis of these parameters from the thrombin generation curve. A prolonged lag-time and reductions in both ETP and peak values indicate a state of hypocoagulability, characterized by less thrombin generation. On the other hand, higher thrombin generation is characterized by reduced lag-time, and increased ETP and peak values, indicating a hypercoagulable state.1
As mentioned previously, the CAT method is based on the use of a synthetic fluorogenic substrate that is sensitive to the action of thrombin.16 However, this synthetic substrate can be cleaved not only by free thrombin, but also by thrombin bound to alpha-2-macroglobulin, potentially resulting in higher values for thrombin generation. To account for this, the CAT method uses an algorithm that nullifies the activity of thrombin linked to alpha-2-macroglobulin.12 Similar to the CAT method, the reagents for this are available from Diagnostica Stago (France). Several versions of this test are currently commercially available for chromogenic (Innovance Endogenous Thrombin Potential assay, Siemens; Pefakit Thrombin Dynamics Test, Pentapharm, Switzerland) and fluorimetric (Technothrombin TGA, Germany) techniques. The advantages and disadvantages of these methods, as well as comparisons, including the reagent concentrations and use of fluorogenic or chromogenic substrates, have been reported elsewhere.1,17
An advantage of TGT is that the operation modes are very flexible, and the experimental conditions are designed for specific purposes. The flexibility of this method allows numerous investigations using various types and concentrations of reagents that activate coagulation, with and without the addition of different substances (e.g., aPC and thrombomodulin), cells (e.g., platelets) or different buffers. An advantage of the fluorogenic method over the chromogenic method is that fibrinogen does not influence the results. As in vivo activation of coagulation occurs in the presence of blood cells, there has been much research into the development of this technique for use with whole blood.18
As mentioned by Lipets and Ataullakhanov,5 although other stimuli can be used, the thrombin generation reaction is generally triggered by the addition of low or high picomolar (pM) concentrations of TF, in addition to phospholipids and Ca2+ ions, in order to measure the bleeding or thrombotic potential. Depending on the intended purpose of the test, the amount of TF added may better reflect particular aspects of the hemostatic mechanism. For example, when high amounts of TF (≥10pM) are added, the reaction is very fast with reduced sensitivity for factors of the intrinsic pathway. However, at TF concentrations between 2 and 5pM, the reaction is more sensitive to deficiencies of factor (F)VIII, FIX and FXI.19 Therefore, in PPP samples, the CAT method is sufficiently sensitive to detect all deficiencies of coagulation factors (with the exception of FXIII) and the effect of all anticoagulants, including vitamin K antagonists, heparinoids, and direct inhibitors of FXa and thrombin, as previously reported by Brinkman.20 With PRP samples, this method is sensitive for cases of von Willebrand disease, and is able to show the effect of platelet inhibitors such as aspirin and abciximab. Furthermore, thrombin generation may be inhibited by the addition of aPC or thrombomodulin, reflecting congenital or acquired disorders of the aPC/PS pathway.12,17,21
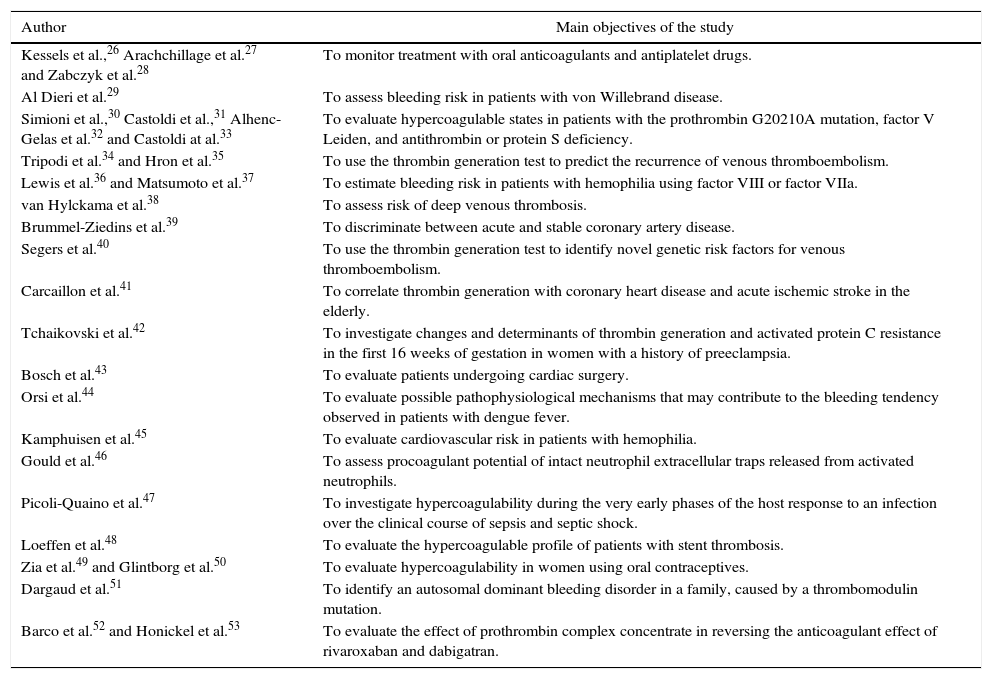
Application of the thrombin generation test as a potential tool for experimental and clinical studiesMany thrombin generation assays have been created to evaluate the clinical potential of this technique, particularly the correlation between TGT parameters and risk of bleeding, and venous and arterial thrombosis.1,18 Of all the thrombogram parameters, ETP appears to be the most widely used, as it is better correlated to the clinical phenotype, as described by Lipets and Ataullakhanov.5 A number of potential clinical applications of TGT have been identified, such as to assess treatment failure of patients who have thrombotic disorders and are receiving oral anticoagulants, heparin, antiplatelet drugs or a combination of such drugs and to comprehensively evaluate the thrombotic or hemorrhagic status of at-risk individuals. Some of the most important reports are presented in Table 1. In the research field, TGT has been widely used in various parts of the world. Briefly, TGT has been used to help elucidate new hemostatic mechanisms by exploring various plasma components, such as those reported by Peraramelli et al.,22 Spronk et al.,23 Omarova et al.24 and Zamolodchikov et al.25 These studies have explored the role of PS in TFPI activity,22 provided new insights into thrombin formation23 and reported a novel mechanism for the inhibition of thrombin-mediated FV activation by the fibrinogen γ′ peptide.24 Furthermore studies have investigated the role of peptide β-amyloid, a key mediator of Alzheimer's disease, as a promoter of thrombin generation through the activation of coagulation FXII.25 Many other studies have proposed or contributed to our understanding of hemostatic mechanisms, however these are beyond the scope of this report.
Potential clinical applications of the thrombin generation test.
| Author | Main objectives of the study |
|---|---|
| Kessels et al.,26 Arachchillage et al.27 and Zabczyk et al.28 | To monitor treatment with oral anticoagulants and antiplatelet drugs. |
| Al Dieri et al.29 | To assess bleeding risk in patients with von Willebrand disease. |
| Simioni et al.,30 Castoldi et al.,31 Alhenc-Gelas et al.32 and Castoldi at al.33 | To evaluate hypercoagulable states in patients with the prothrombin G20210A mutation, factor V Leiden, and antithrombin or protein S deficiency. |
| Tripodi et al.34 and Hron et al.35 | To use the thrombin generation test to predict the recurrence of venous thromboembolism. |
| Lewis et al.36 and Matsumoto et al.37 | To estimate bleeding risk in patients with hemophilia using factor VIII or factor VIIa. |
| van Hylckama et al.38 | To assess risk of deep venous thrombosis. |
| Brummel-Ziedins et al.39 | To discriminate between acute and stable coronary artery disease. |
| Segers et al.40 | To use the thrombin generation test to identify novel genetic risk factors for venous thromboembolism. |
| Carcaillon et al.41 | To correlate thrombin generation with coronary heart disease and acute ischemic stroke in the elderly. |
| Tchaikovski et al.42 | To investigate changes and determinants of thrombin generation and activated protein C resistance in the first 16 weeks of gestation in women with a history of preeclampsia. |
| Bosch et al.43 | To evaluate patients undergoing cardiac surgery. |
| Orsi et al.44 | To evaluate possible pathophysiological mechanisms that may contribute to the bleeding tendency observed in patients with dengue fever. |
| Kamphuisen et al.45 | To evaluate cardiovascular risk in patients with hemophilia. |
| Gould et al.46 | To assess procoagulant potential of intact neutrophil extracellular traps released from activated neutrophils. |
| Picoli-Quaino et al.47 | To investigate hypercoagulability during the very early phases of the host response to an infection over the clinical course of sepsis and septic shock. |
| Loeffen et al.48 | To evaluate the hypercoagulable profile of patients with stent thrombosis. |
| Zia et al.49 and Glintborg et al.50 | To evaluate hypercoagulability in women using oral contraceptives. |
| Dargaud et al.51 | To identify an autosomal dominant bleeding disorder in a family, caused by a thrombomodulin mutation. |
| Barco et al.52 and Honickel et al.53 | To evaluate the effect of prothrombin complex concentrate in reversing the anticoagulant effect of rivaroxaban and dabigatran. |
Although TGT has many potential clinical applications and considerable advantages over almost all other techniques, it also has some limitations that need to be overcome before its use in clinical laboratories. Although this technique can be performed using PPP or PRP, this involves a time-consuming process, which prevents its use for rapid diagnosis. An ideal technique would be performed using whole blood samples containing all blood cells, which would reproduce the in vivo conditions better.18 It should be noted that there are other tests that can be used for the overall assessment of hemostasis, such as thromboelastography (TEG® systems, Haemonetics Corporation, Braintree, MA, USA) and thromboelastometry (ROTEM®-Analyser, Tem Innovations GmbH, Munich, Germany), both of which are performed using whole blood. Thromboelastography, a global test widely used in the management of acute hemorrhages, is also capable of detecting hypercoagulable states.54 However, according to Lancé,13 this method does not fully reflect the effects of using low-molecular-weight heparin or the direct use of oral anticoagulants, nor the effects of inherited or drug-induced platelet dysfunction. TGT presents a wider range of potential clinical applications compared to thromboelastography. Thus, the application of TGT on whole blood (containing all blood cells) may outweigh the advantages of TGT on plasma, as this assay may better reflect the in vivo conditions.
The lack of reference values for specific TGT conditions, such as the type and concentration of the triggering agent, or whether or not a contact inhibitor factor is used, makes the use of TGT difficult in clinical laboratories, as it requires appropriate interpretation of the results. As stated by Spronk et al.,55 there is no consensus as to whether a contact pathway activation inhibitor should be used, for example, whether corn trypsin inhibitor is required. These reference values should ideally be established for each center according to the adopted protocol, and would require identical conditions for patient and control samples, including blood collection, sample preparation and storage. Another important limitation of TGT is the lack of sensitivity to changes in the endothelium. Although it is increasingly being recognized as a more precise test that replicates the in vivo hemostatic conditions, TGT still lacks official standardization, despite several studies having been conducted.55–57 Therefore, it is mandatory to standardize the main sources of variation, such as pre-analytical and analytical conditions and reagents, particularly the origin and concentration of TF. Such measures will certainly reduce intra- and inter-assay inaccuracies, and the large inter-laboratory variability of the method. However, future improvements of this technique, including the addition of endothelium-derived components to the reaction, may increase the predictive value of assays for the overall assessment of hemostasis. Therefore, standardization and validation of this method are essential for its introduction into the clinical practice. Evaluation of characteristics and conditions to ensure the reproducibility and accuracy of TGT are required.54 In line with this, Dargaud et al.8 evaluated a standardized protocol for measuring thrombin generation using the CAT method in an international multi-center study. These authors demonstrated that the use of standard conditions, such as identical equipment, standardized reagents, reference plasma for the normalization of results, and the same test procedure, showed a great reduction in assay variability compared to previously published data. Their data demonstrated that the standardized TGT methodology evaluated in this report effectively reduces the variability of this assay to acceptable limits.
In short, we agree with Othman58 on the need for a standardized global test that can reliably detect, predict and monitor hemostatic status for clinicians and researchers, in both clinical and experimental studies.
ConclusionsBased on the current literature TGT aims to globally assess hemostasis, providing information about the initiation, amplification/propagation and resolution phases. The results from this test are more representative of the physiological state, which may better reflect the hemostatic phenotype compared to routine tests, and has great potential for the evaluation of the risks of bleeding and thrombosis. However, TGT is not yet available for clinical use, as it still requires standardization and validation. The use of a standardized method may reduce the variability of this assay to acceptable limits. Finally, an ideal coagulation test does not exist yet. However, new developments are continuously emerging aimed at improving existing tests in order to globally assess hemostasis, particularly TGT using the CAT method.
Conflicts of interestThe authors declare no conflicts of interest.
We thank the Brazilian agencies FAPEMIG/SES and MS/CNPq for funding this study.