Hemoglobin (Hb) A2 (α2δ2) constitutes less than 3% of the total hemoglobin (Hb) in adults and has almost no physiological importance.1 On the other hand, the determination of Hb A2 is an important tool to diagnose the beta-thalassemia trait (BTT).1,2 Although individuals with BTT do not need treatment, the accurate detection of the carrier state is important in genetic counseling to determine risk of having a child with a major disease.3
Elevated levels of Hb A2 and microcytosis are suggestive of the diagnosis of BTT. However, BTT may be present with normal levels of Hb A2 as a few cases of β-thalassemia are not associated with elevated Hb A2, and because of the association of BTT with iron deficiency or with α-thalassemia (α-Thal).1,2,4–6 There are many other factors, inherited or acquired, that can interfere in Hb A2 levels (Table 1).3,4
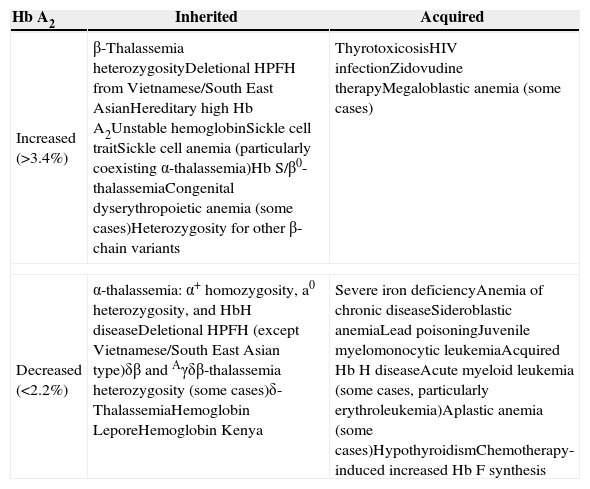
Causes of variation in the percentage of hemoglobin A2.
| Hb A2 | Inherited | Acquired |
|---|---|---|
| Increased (>3.4%) | β-Thalassemia heterozygosityDeletional HPFH from Vietnamese/South East AsianHereditary high Hb A2Unstable hemoglobinSickle cell traitSickle cell anemia (particularly coexisting α-thalassemia)Hb S/β0-thalassemiaCongenital dyserythropoietic anemia (some cases)Heterozygosity for other β-chain variants | ThyrotoxicosisHIV infectionZidovudine therapyMegaloblastic anemia (some cases) |
| Decreased (<2.2%) | α-thalassemia: α+ homozygosity, a0 heterozygosity, and HbH diseaseDeletional HPFH (except Vietnamese/South East Asian type)δβ and Aγδβ-thalassemia heterozygosity (some cases)δ-ThalassemiaHemoglobin LeporeHemoglobin Kenya | Severe iron deficiencyAnemia of chronic diseaseSideroblastic anemiaLead poisoningJuvenile myelomonocytic leukemiaAcquired Hb H diseaseAcute myeloid leukemia (some cases, particularly erythroleukemia)Aplastic anemia (some cases)HypothyroidismChemotherapy-induced increased Hb F synthesis |
Hb A2 – hemoglobin A2; HPFH: hereditary persistence of fetal hemoglobin; HIV: human immunodeficiency virus; HbH: hemoglobin H; Hb F: hemoglobin F or fetal hemoglobin.
Hb A2 can be measured by several laboratorial methods, but these methods have differences in accuracy.7 Cation exchange high performance liquid chromatography (HPLC), microcolumn chromatography, and cellulose acetate electrophoresis with elution are considered acceptable methods to diagnose BTT, whereas cellulose acetate electrophoresis followed by scanning densitometry is not.2 The accuracy of cellulose acetate electrophoresis with elution depends on the training and experience of the laboratory technician who performs the test, and microcolumn chromatography can give problems with co-elution of some Hb variants.7
Recent studies have confirmed the higher quality of automated HPLC in the measurement of Hb A2 compared to the other methods,8,9 which is why this has become the method of choice. On the other hand, in automated HPLC, the measurement of Hb A2 is inaccurate when Hb S is present.2,3,10 As the amount of Hb S is related to the degree of inaccuracy, levels are higher in patients with sickle cell anemia (SCA) or Hb S/β-thalassemia (S-βThal) than in sickle cell trait.2 Thus, the amount of Hb A2 does not indicate BTT when Hb A and beta gene variants are found together.11 Furthermore, when beta gene variants are present without Hb A, the diagnosis of concomitant BTT is not necessarily associated to the elevation of Hb A2 and so further investigations using family studies or DNA analysis are necessary.10
As mentioned above, α-Thal is capable of interfering in the determination of Hb A2.4 Individuals with the α0-thalassemia trait or homozygous for α+-thalassemia have lower levels of Hb A2, but the influence of the coinheritance of α-Thal and BTT on Hb A2 levels is uncertain.6
In Brazil, the incidence of α-Thal varies from 0.11 to 0.22% depending on the geographical region studied.12–15 It is well known that the association of α-Thal and SCA is common in Brazil.16–18 Since SCA is considered a public health problem in Brazil and due to the clinical significance of α-Thal in respect to this anemia, diagnosis is important.19–21 However, diagnosis is mainly achieved by molecular techniques that are expensive and not easily accessible. It is also important to remember that the co-inheritance of α-Thal and SCA results in increased levels of Hb A2 as measured by automated HPLC, and could result in a misdiagnosis of S-βThal.4
There lies the importance of the paper entitled “Hemoglobin A2 values quantified by high performance liquid chromatography in patients with sickle cell disease, and the influence of the presence of alpha-thalassemia” written by Fonseca et al. and published in this edition of the Revista Brasileira de Hematologia e Hemoterapia.22 The authors demonstrate that Hb A2 was overestimated not only in individuals with Hb S but also in patients with Hb C, and that the Hb A2 level was influenced by the genotype of α-Thal.
In conclusion, in a country with a high degree of miscegenation such as Brazil, not only the diagnosis of double heterozygous states, such as S-βThal, but also the diagnosis of co-inheritance of SCA with α-Thal should be carried out carefully, taking into consideration the limitations of the available laboratory techniques. Family studies or DNA analysis, when possible, are desirable to confirm the correct diagnosis.
Conflicts of interestThe authors declare no conflicts of interest.
See paper by Fonseca et al. on pages 296–301.