Hematopoietic stem cell transplantation is the only curative treatment for many disorders and international data shows a growing trend.
MethodWe aimed to evaluate the temporal trends in HSCT transplant rates in Argentina. A time-series analysis was performed for the period 2009 to 2018 using the national database from the National Central Coordinating Institute for Ablations and Implants. Crude and standardized transplant rates were calculated. A permutation joinpoint regression model analysis was used to identify significant changes over time.
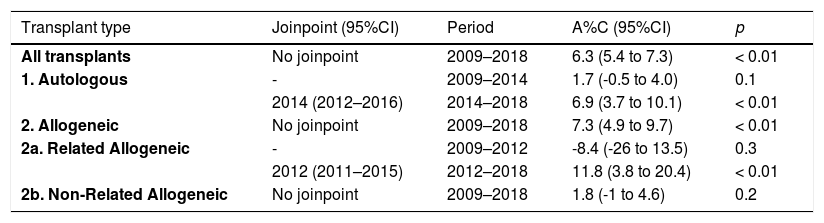
ResultsAltogether, 8,474 transplants were reported to INCUCAI by 28 centers (autologous 67.5%); the main indication was multiple myeloma (30%). The WHO age-sex standardized HSCT rates for the entire country were 153.3 HSCT/10 million inhabitants (95% CI 141.7–165.8) in 2009 and 260.1 HSCT/10 million inhabitants (95% CI 245.5–275.5) in 2018. There was a large gap in HSCT rates among the states and regions. The transplant rate was higher for autologous transplants throughout the years. Within the allogeneic group, the related donor transplant rate was higher than the unrelated donor transplant rate. The joinpoint regression analysis of HSCT rates for the whole country over time showed an observed annual percentage change of 6.3% (95% CI 5.4-7.3; p < 0.01). No changes were observed for unrelated donors during the study period.
ConclusionsAge-sex standardized HSCT rates in Argentina are increasing, mainly due to autologous and family donor allogeneic transplants. A wide variation across the country was found, demonstrating differences in the access to transplantation among Argentine regions.
Hematopoietic stem cell transplantation (HSCT) is the only curative treatment for many disorders, including hematological malignancies and benign diseases, both acquired and congenital. Autologous, as well as allogeneic HSCT, have been used for more than 20 years,1 the first HSCT having been performed in Argentina in 1986.2 In recent years, significant changes have occurred in the transplant field, such as an improvement in the supportive care and the spectrum of the conditioning regimen, increasing the age for transplant, and the access to the transplant of patients with comorbidities; particularly in the allogeneic setting, a wide availability of donors, including mismatched donors, have been reported.3 In Argentina, the creation of a Registry of HSC Voluntary Donors in 2001 added more possibilities to increase the HSCT rate in our country.2 At present, more than 80,000 transplants are performed all over the world every year and this number is expected to rise.4,5
However, the HSCT is a highly specialized, technologically sophisticated procedure, which requires expensive resources and a multidisciplinary team of trained transplant personnel. For these reasons, access to the HSCT suffers great inequality across several regions of the world, including within the same country, even in developed countries.6,7 The rate of transplants in different nations has already been reported and this was found to be significantly correlated with economic indexes.8 A voluntary survey of members of the Latin American Bone Marrow Transplantation Group (LABMT) regarding transplant activity between 2009 and 2012 showed a median transplant rate (number of transplants per 10 million inhabitants) of 64 in 2012, which is 5- to 8-fold lower than the corresponding rate for North American and European regions. In this LABMT survey, the corresponding transplant rate for Argentina was 149 (38 for allogeneic and 110 for autologous transplants).9 However, there are no data available on the homogeneity of access to the transplant procedure in Argentina, where there is also a significant internal migration for this procedure.
We aimed to evaluate the temporal trends in HSCT transplant rates in Argentina from 2009 to 2018 and transplant rates across the country and to estimate the effect of age, period and birth cohort, using the national database from the National Central Coordinating Institute for Ablations and Implants (INCUCAI).
MethodsStudy designA time-series analysis was carried out to assess temporal trends in HSCT rates in Argentina from 2009 to 2018 using official secondary databases. The main outcome was to evaluate the temporal trend in HSCT rates for all HSCTs and by donor type. Secondary outcomes were the description of the indications and HSCT rates by state and age of the recipient and were used to estimate the effect of age, period and birth cohort. The Independent Ethics Committee and INCUCAI approved the protocol and authorization from each transplant center was requested for this study.
Data source and variablesThe number of HSCT transplants from 2009 to 2018 was obtained from the INCUCAI Registry.10 This is an official and mandatory national reporting system, created in 2009, that compiles information on all the transplants performed in Argentina. From this database, we obtained data on the number of transplants, type of transplant (autologous and allogeneic), age at transplant, state of origin of the patient, underlying disease and year of transplant. The state of residence of the patient referred to the location of the primary residence of the patient, but not to the center where the transplant was performed. Until 2018, in Argentina, transplant centers were located in five out of twenty-four states (Ciudad Autónoma de Buenos Aires, Buenos Aires, Córdoba, Santa Fe and Misiones). Related transplants included matched sibling and mismatched/haploidentical family donors; unrelated donor transplants included HSCT from matched or mismatched unrelated donors with peripheral blood and marrow as a stem cell source, with cord blood HSCT included. We used the 2000 and 2010 censuses and inter-census estimations from the National Institute of Statistics and Censuses (INDEC) as population denominators.11 We used the geopolitical division of Argentina into twenty-four states.12 Authorization for this study could not be obtained from a few centers, which were closed during the performance of this study; missing data were compensated by applying the corresponding percentage in each calendar year.
Definitions and statistical analysisCrude and standardized transplant rates were calculated per 10 million inhabitants13 for each year between 2009 and 2018, considering the whole country, as well as each state. Transplant rates were age-sex standardized, based on the standard population proposed by the WHO14 and the Argentine population, according to the 2010 census.11,15 Age-sex standardized HSCT rates were determined by the calendar year and by the state of Argentina. Additionally, we computed the team density as the number of transplant teams per 10 million inhabitants and the team distribution, as the number of transplant teams per 10,000 square kilometers.16
We evaluated time trends of annual age-sex standardized transplant rates using a permutation joinpoint regression model analysis to identify significant changes over time throughout the 10-year period in Argentina, considering all transplants and then, according to the donor type. We considered as “joinpoint” the significant changes in time-related trends.17–20 We used the Joinpoint Regression Program 4.7.0.0 (February 26, 2019) developed by the United States National Cancer Institute.17,21
HSCT rates may also vary due to differences in age, period and birth cohort effects. These components that modify HSCT rates may correspond to different factors affecting the distribution of hematological disease, its diagnosis, its treatment and response to treatment, among others. The incorporation of these three components related to time simultaneously in a model is called the non-identifiability problem.22 In view of this problem, we chose age-period-cohort (APC) models using the Poisson regression for event counts to estimate the effect of each of these components on HSCT rates. APC models were fitted using the STATA apcfit command 15.1 version (Copyright 1985–2015 StataCorp LLC. Statistics/Data Analysis. StataCorp, 4905 Lakeway Drive - College Station, Texas 77845 USA). It models age, period and cohort effects by fitting cubic splines and overcomes the identification problem arising from the linear relations of the three time-related factors.23,24 Since APC models treat time-related variables as continuous, we used the period and HSCT rates estimated for each year. As age was obtained by five-year intervals, we used the age in the middle of each interval to fit the APC model. We used the year 2014 and the 1970 birth cohort as references for period and birth cohort effect estimation, respectively. The specific effects of the period and birth cohort were estimated as relative risks (RR) to this reference, respectively, and presented with a 95% CI.
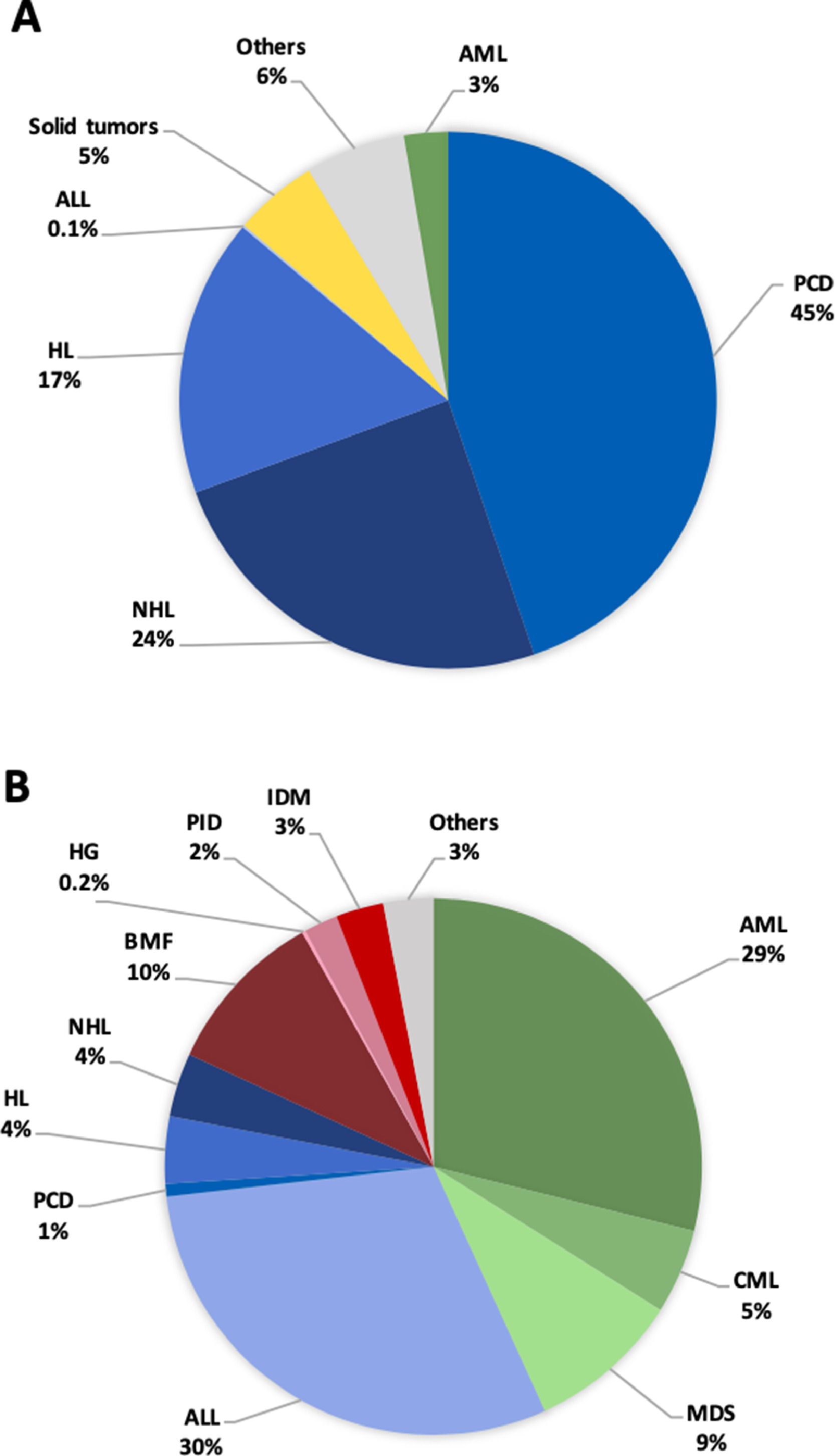
ResultsNumber of transplantsAltogether, 8474 transplants were reported to the INCUCAI (Tables S1 and S2) between 2009 and 2018 by 28 centers: autologous n = 5,724 (67.5%), allogeneic n = 2,750 (32.5%; matched sibling n = 1,518; family haploidentical n = 537, and; unrelated donors n = 825). The total number of patients who underwent transplant under the age of 20 in both dedicated and joint adult-pediatric units was 1,206 (14%; autologous and allogeneic) (Table S1). A low number of patients were transplanted after the age of 65 (n = 761; 9%) and no transplant was registered after the age of 80. The absolute number of HSCT, according to the state of residence of the patient, is shown in Table S2. The absolute number of HSCT by state ranged from 3209, for patients residing in Buenos Aires, to 39, for patients residing in Santa Cruz. The most frequent indications for HSCT in the 2009 to 2018 period are shown in Figure 1. The main indication for HSCT was multiple myeloma (30%), followed by non-Hodgkin lymphoma (17.3%), Hodgkin lymphoma (12.2%), acute myeloid leukemia (11.6%), acute lymphoblastic leukemia (10.3%), aplastic anemia (3.5%), solid tumors (3.3%), myelodysplastic syndrome (3.3%) and other indications (8.6%). The lowest number of HSCT was registered for hemoglobinopathies (six HSCTs throughout the studied period). For the year 2018, the team density demonstrated a high concentration of transplant teams in the capital of the country (Ciudad Autónoma de Buenos Aires, CABA) with a rate of 42.4 per 10 million inhabitants. In respect to the other states performing transplants, the team density was as follows: Santa Fe 8.6, Córdoba 8.2, Misiones 8.1 and Buenos Aires 4.1. The team distribution followed a similar pattern: CABA 689.6, Misiones 0.3, Santa Fe 0.2, Buenos Aires 0.2 and Córdoba 0.2 (per 10,000 km2). Considering the whole country, the team density was 6.1 and the team distribution was 0.1. The median number of HSCTs per team was 28.
Main indications of patients transplanted during the 2009–2018 period. (A), Autologous; (B), Allogeneic. ALL: acute lymphoid leukemia; AML: acute myeloid leukemia; BMF: bone marrow failure; CML: chronic myeloid leukemia; HG: hemoglobinopathy; HL: Hodgkin lymphoma; IDM: inherited diseases of metabolism; MDS: myelodysplastic syndrome; NHL: non-Hodgkin lymphoma; PCD: plasma cell disorders; PID: primary immune disease.
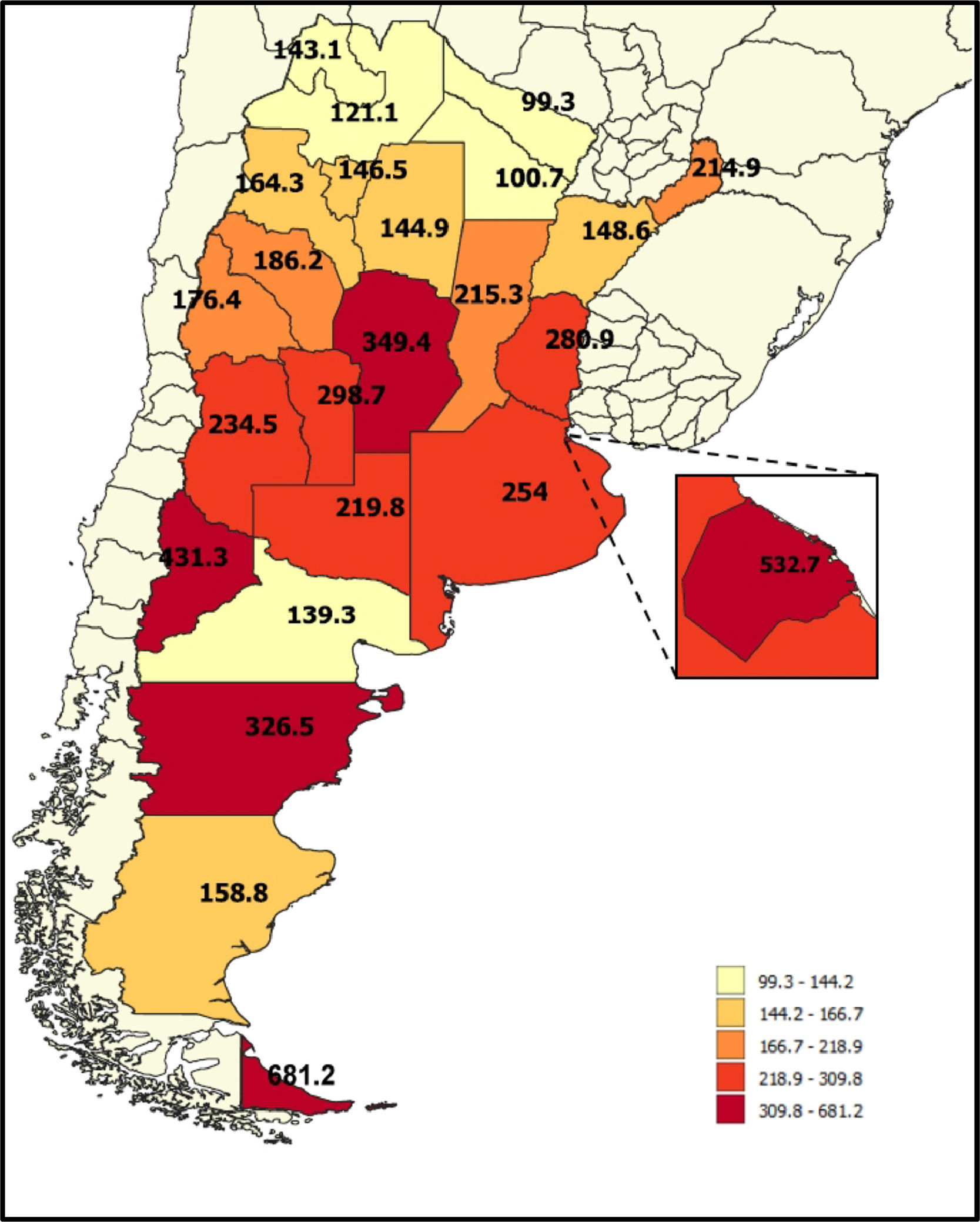
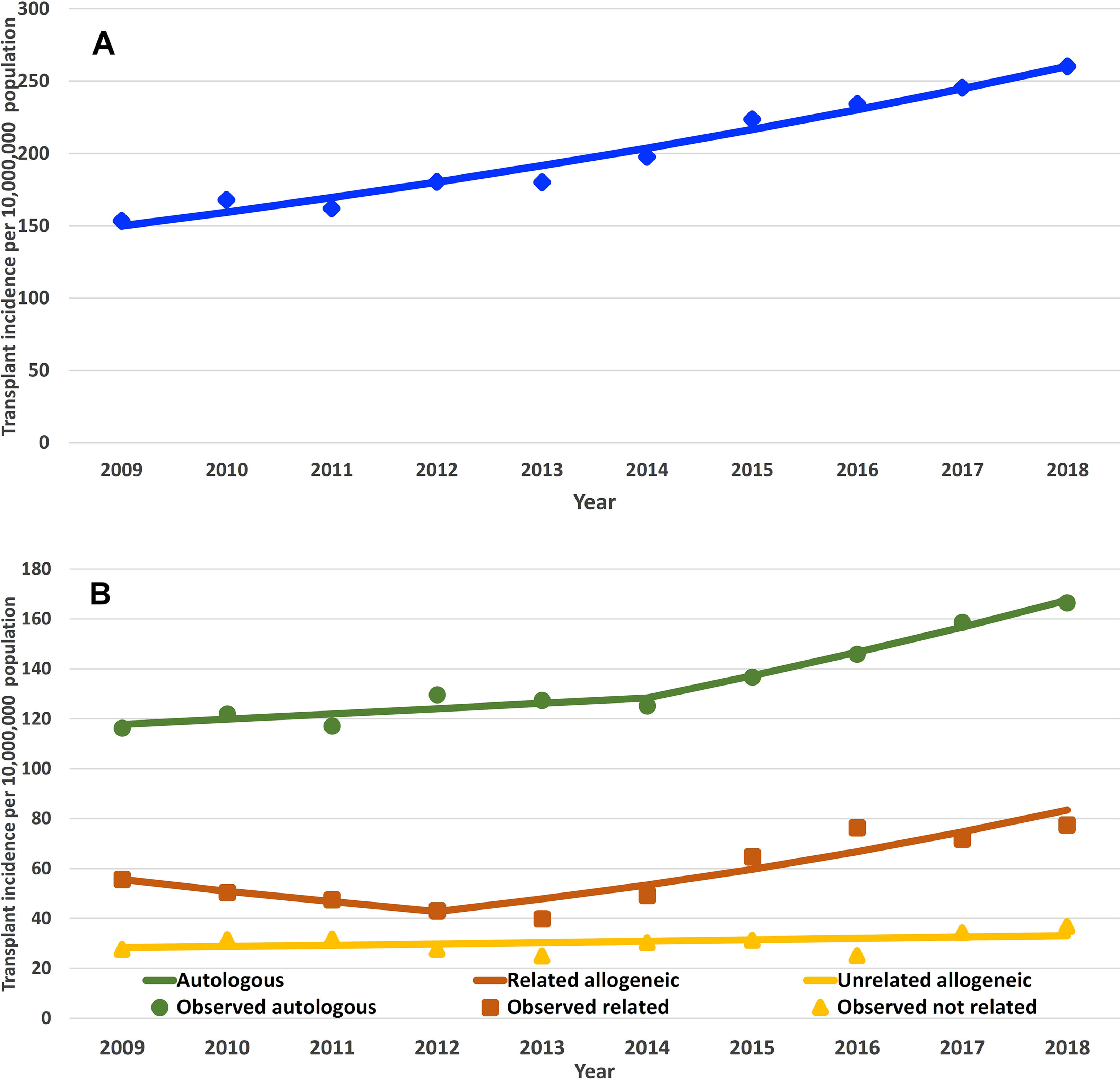
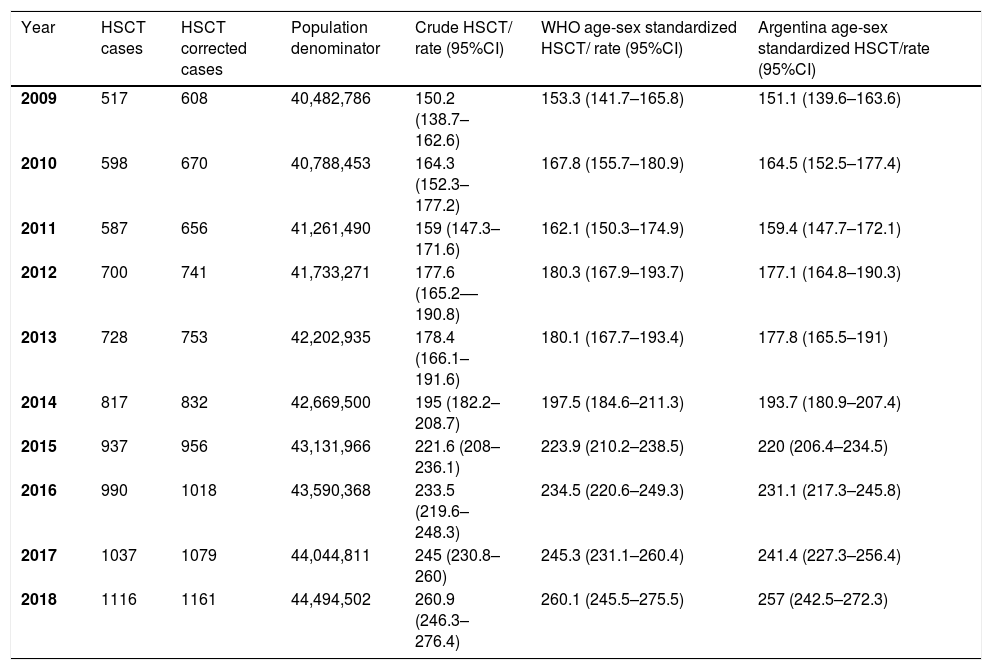
A total of 8474 HSCTs were performed in the whole country during the 10-year study period. The WHO age-sex standardized HSCT rates for the entire country were 153.3 HSCT/10 million inhabitants (95% CI 141.7–165.8) in 2009 and 260.1 HSCT/10 million inhabitants (95% CI 245.5 – 275.5) in 2018. The rates for the entire period showed an increment, presented in Figure 2A and Table 1. The transplant rate was higher for autologous transplants throughout the years (Figure 2B). Within the allogeneic group, the related donor transplant rate was higher than the unrelated donor transplant rate (Figure 2C). Trends for all donors are shown in Figure 3. The proportion for haploidentical family donors was 1.9% in 2009, increasing to 11.4% in 2014, 26.7% in 2015 and 33.1% in 2016, overcoming unrelated donors. For the year 2018, the proportion of donors for the allogeneic transplant was as follows: matched sibling 44.1, haploidentical 30.6% and unrelated donors 25.3%. HSCT rates according to age are shown in Figure 4. For the year 2018, the highest HSCT rate was observed in the 60 to 69 age cohort, this also being the main cohort for the autologous transplant. In the allogeneic group, the 50 to 59 age range was the main group receiving a transplant (Table S3). Age-sex standardized HSCT rates for the entire period by state and regions of the country are shown in Table S3 and the trend by region in Figure 1S. There is a large gap in HSCT rates among the states and regions. For the year 2018, the highest transplant rate was observed for patients from Tierra del Fuego, followed by CABA, Neuquén, Córdoba and Chubut (all greater than 300); a transplant rate less than 150 was found for patients from Formosa, Chaco, Corrientes, Jujuy, Santiago del Estero, Tucumán and Salta (Figure 5). None of these states had a transplant team in the study period.
Crude and WHO age-sex standardized HSCT rates per 10 million inhabitants. Argentina, 2008–2019.*
HSCT; hematopoietic stem cell transplantation.
The joinpoint regression analysis of HSCT rates for the whole country over time showed an observed A%C of 6.3% (95% CI 5.4 - 7.3; p < 0.01) without any significant joinpoint detected (Table 2 and Figure 6). However, when the analysis considered the type of transplant, the joinpoint regression analysis of the HSCT rates showed different patterns of the temporal trend (Table 2). In regard to autologous transplants, it showed two segments separated by a joinpoint as the best model. The first segment, from 2009 to 2014, had a non-significant A%C of 1.7% (-0.5–4.0; p = 0.1), while the last segment, from 2014 to 2018, showed a significant A%C of 6.9% (3.7 - 10.1; p < 0.01.). In respect to all allogeneic transplants, the observed annual percentage change was significant; however, it was not in the unrelated group and in the first years for related transplants (Table 2). All joinpoint regression-modeled HSCT rates, as well as by type of transplant, for Argentina are shown in Table 2 and Figure 6.
Transplant types with trends as defined by joinpoint analyses by calendar year. Argentina, 2009–2018.a
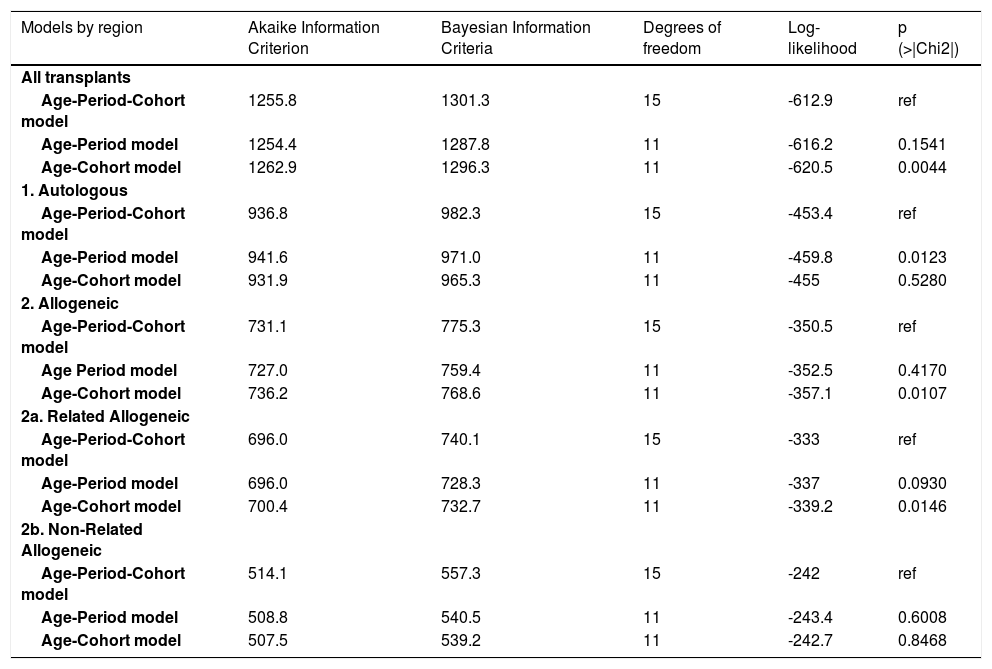
The APC analysis showed that age was the variable significantly associated with a trend for all transplants and by donor type (Table 3). For all transplants, two segments of age can be identified: one segment up to the age of 45 and the other segment over 45 to 60 years old. Globally, the transplant rate started to increase around the year 2013 and stabilized around the year 2015 (period effect). The inclusion of the birth cohort in the model may have not changed the results (Table 3, Figure 4S). Further analysis of the subtypes of transplants is affected by the low number of events; therefore, the interpretation should be taken with caution. In respect to autologous transplants, an upward segment between 40 and 60 years old is observed and this group clearly shows how the transplant rate increased with age. There is no effect of period and, regarding the cohorts, an increase by 1970 can be seen (Table 3, Figure 4S). For allo-transplants, again, the effect of age is evident, particularly after the year 2013 and for related donors. Younger cohorts may have a greater possibility of allogeneic transplants. In the case of unrelated donors, no effect of age, period or cohort is apparent (Table 3, Figure 4S).
Adjustments to the models of age-period-cohort effects, for transplant rate in Argentina and by transplant type, from 2009 to 2018. All p-values test the null hypothesis of equal goodness of fit between each model compared with the APC complete model.*
APC: age-period-cohort.
This study presented the first comprehensive report of the HSCT rate in Argentina. Using a National Database comprising all transplants performed in Argentina between 2009 and 2018, we found a steadily increasing HSCT rate, going from 153.3 HSCT/10,000,000 inhabitants in 2009 to 260.1 HSCT/10,000,000 inhabitants in 2018. This rate showed a significant increase throughout the studied period, mainly because of the autologous and related allogeneic transplants, without changes regarding unrelated allogeneic transplants. We also showed a large heterogeneity across the country, with rates ranging between 99 and 680 transplants for the year 2018.
According to the 2017 report, the highest transplant rate in Europe was registered for Germany (930), followed by Italy (850) and France (830) and the lowest rate was recorded by Romania (160).25 In the Asian-Pacific region, the highest HSCT rate was evidenced in Australia (714) and the lowest one in Myanmar (0.4) for the year 2015.26 Our transplant rate is lower than most European countries; however, the lowest rate for an Argentine province (99) is higher than the Latin American global rate (69).5
Overall, autologous HSCTs were more frequently reported than allogeneic HSCTs. This proportion is slightly higher than the global world perspective previously reported for the year 2006,27 but different from the Asian-Pacific region, where allo-transplants are more frequent; the main indication of the transplant in this population was hemoglobinopathy, which may account for the difference.26 Higher use of allogeneic, compared to autologous, HSCT was also reported for the East Mediterranean/African region.28 The highest proportion of autologous transplants explains that our main indication for transplant was plasma cell disorders, representing 45% of the diagnosis. Globally, 14% of transplants in the pediatric population is quite similar to the percentage previously reported.29 For 2018, the absolute number of patients transplanted after the age of 60 (23.6%) and after the age of 70 (2.1%) observed in our country was low, the majority being autologous transplants; however, when considering the age-sex HSCT rate, the highest was for the 60 to 69 years age group in the autologous transplant. The number of both autologous and allogeneic transplants for the treatment of malignant diseases in older patients continues to grow.4,30 According to the CIBMTR report, 39% of allogeneic transplant recipients were 60 years old and older and 55% of autologous transplant recipients for lymphomas and multiple myeloma were 60 or older in 2018. Likewise, patients ≥ 70 years old represented 9% of allogeneic transplants and 15% of autologous transplant activity in 2018, as per the CIBMTR data.31
An upward and predictable trend in the HSCT rate has been reported since 1999 from surveys in Europe.16 Additionally, according to the CIBMTR report for the United States in 2015, the number of autologous hematopoietic cell transplantations (HCTs) has steadily risen since 2000, mainly for the treatment of plasma cell and lymphoproliferative disorders and due to an increase in the age at transplant.32 In our report, joinpoint regression analysis indicated a significant trend towards increasing HSCT rates over time. A considerable period effect may reflect a global rise in the transplant rate since 2013, probably due to the access to novel agents in prevalent diseases for transplant, such as multiple myeloma (in the autologous rate), lymphoma and acute leukemias (in allogeneic cases), as well as the wide incorporation of the use of mismatched/haploidentical family donors for the allogeneic after 2014, overcoming unrelated donors since 2016. In the autologous transplant group, a sharp increase in the HSCT rate after the age of 40 was found, with an effect of birth cohorts before 1970 and without the effect of the period. In the allogeneic transplant setting, an increase in the HSCT rate with age is also found, with a probable change after 2013, without the birth cohort effect. In respect to unrelated donor transplants, no effect of age, period or cohort was found. Unlike the US and Europe, where unrelated donors surpassed related donors,33 in Argentina, this type of transplant remains the lowest (40% out of the allogeneic), despite the growth of unrelated donor registries all over the world. Our transplant rate for unrelated donors was 36.8 in 2018 (per 10 million inhabitants), which is less than a half than that reported for Switzerland and Germany (218 and 109 per 10 million inhabitants per year, respectively).33 This observation may reflect that probably not all patients in need of an allogeneic transplant have access to it, in addition to the growing use of mismatched/haploidentical family donors during the last years may have influenced this figure. Alternatively, the probability of finding a well-matched unrelated donor for our population may be lower than in Europe34 and this emphasizes the need to make major efforts to recruit donors in local registries.33
We showed a large heterogeneity across the country regarding HSCT rates. It is known that transplant rates are influenced by economic and sociodemographic factors, as well as by team density and team distribution.16,35 Among the macroeconomic factors, Gratwohl et al. identified governmental health care expenditures as the most closely associated with HSCT rates.27 A CIBMTR analysis showed that a higher percentage of individuals below the poverty line and patients with acute myeloid leukemia remained significantly associated with a lower transplantation rate and that the geographical location within the country (rural vs urban) was also associated with a lower transplant rate. These factors were not significant in the pediatric populations.36 In Europe, a wide regional difference in the access to the search for unrelated donors was found in Italy for patients with acute leukemia; furthermore, a considerable internal migration to obtain access to the transplant was found.8 A marked difference in transplant rates between regions was also described in Spain. In respect to the autologous transplantation rate, the only associated variable was the team density, whereas there was a strong influence of macroeconomic determinants in the case of allogeneic transplant rates.37 The high heterogeneity of transplant rates in Argentina may depend on these factors, but also on the variation in the insurance coverage of the transplant cost across the country. Access to transplants in our country may be affected by the team density and team distribution. The highest indicators are observed in CABA, the capital of the country; however, considering the whole country, the team density is lower than 10 (per 10 million inhabitants) and the team distribution is lower than 1 (per 10,000 km2), both suggested targets for establishing the HSCT in a country.16 In our study, the median number of transplants by team of ∼30 transplants per year is nearly half of the number reported by European centers.33 HSCT teams in Argentina are concentrated in five out of the twenty-four states in the country (four of them in the central region); therefore, in contrast to the US, most patients in Argentina will have to travel long distances to access a transplant center. However, the analysis of this factor is beyond the scope of this study.38
We used a careful statistical methodology to address our questions. However, the low number of observations in the analysis of the studied groups may limit the power of such analysis, as evidenced in the confidence intervals shown in the APC figures. In regard to HSCT rates by state, we assumed a similar disease incidence for all states and the lack of systematic national information precludes a further analysis, although it seems that there is no clear pattern of higher incidence in any particular Argentine region. Furthermore, the analysis of the outcome of the transplants was beyond the scope of this study.
In conclusion, age-sex standardized HSCT rates in Argentina have been increasing in recent years, mainly due to autologous and family donor allogeneic transplants. A wide variation in HSCT rates throughout the country was found, demonstrating differences in the access to transplantation among Argentine regions. This study will allow us to make a “situation diagnosis” (in order to know the country's reality) and, therefore, to guide programs aimed at ensuring accessibility through an equitable allocation of resources, the knowledge of the appropriate transplant application process, patient eligibility, the importance of timely planning and, as a final result, the quality of the procedure.
We give our special thanks to INCUCAI staff and participating centers: CEMIC, Centro de Hematología y Trasplante, CETRAMOR, Corporación Médica San Martín, Fundación Favaloro, FUNDALEU, HIGA General San Martín, Hospital Alemán, Hospital Británico, Hospital El Cruce, Hospital de Clínicas José de San Martín, Hospital de Niños Ricardo Gutiérrez, Hospital de Niños Víctor J Vilela de Rosario, Hospital de Niños Sor Ludovica de La Plata, Hospital de Niños Santísima Trinidad de Córdoba, Hospital de Pediatría Juan P Garrahan, Hospital Interzonal de Agudos Prof. Rodolfo Rossi, Hospital Italiano de Buenos Aires, Hospital Italiano de La Plata, Hospital Italiano de San Justo, Hospital Universitario Austral, Hospital Privado Universitario de Córdoba, Instituto Médico Alexander Fleming, Instituto Médico de Alta Complejidad, Sanatorio Allende, Sanatorio Anchorena, Sanatorio Sagrado Corazón and Hospital Escuela Ramón Madariaga.