T-cell prolymphocytic leukemia (T-PLL) is an uncommon mature T-cell neoplasm characterized by the proliferation of abnormal lymphoid cells morphologically akin to prolymphocytes.1 However, in some rare variant forms of the disease, the prolymphocytic lymphoid cells are absent.
Here, we present a rare variant of T-PLL that, unless remembered and, from an immunophenotypic point of view, adequately studied, can be misdiagnosed.
Case reportA 59-year-old woman was referred to our laboratory with a request for an immunophenotyping of peripheral blood due to lymphocytosis in CBC. She had diabetes mellitus, systemic arterial hypertension, dyslipidemia, and morbid obesity. Unfortunately, we did not receive any additional clinical or laboratorial information.
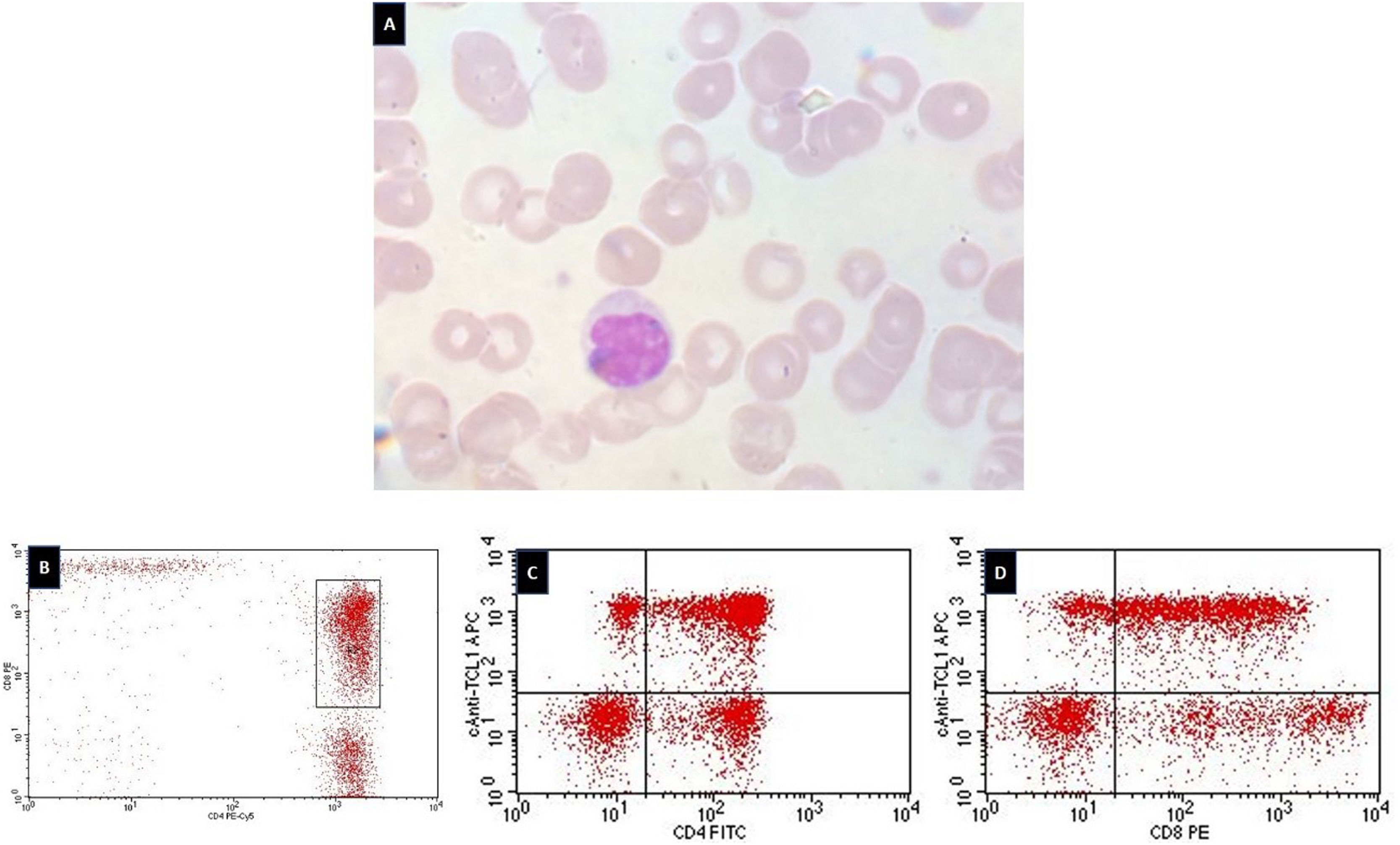
The blood film revealed the presence of small to medium-sized lymphoid cells characterized by convoluted nucleus with condensed chromatin without nucleoli, and slightly basophilic cytoplasm devoid of granules. The cytomorphological appearance was suggestive of Sézary syndrome (Figure 1, A).
Cytological and flow cytometry findings of the patient's blood. (A) The blood smear shows the cerebriform aspect of the nucleus of the lymphoid cell (Leishman stain; x100 objective). (B) Dot-plot showing the double positive (CD4 and CD8) T-cells. (C) Dot-plot showing the CD4+/TCL1+ T-cells. (D) Dot-plot showing the CD8+/TCL1+ T-cells.
The flow cytometry analysis showed the presence of 15% of mature T-cells (CD3+, CD34−, nTdT−) with the following immunological profile: CD2+, CD5+, CD7+, CD26+, CD45bright, CD103partial, and TCRαβ+. Significantly, the mature T-cells were also double-positive for CD4brigth and CD8brigth (48% of the T-cells) (Figure 1, B), and were also positive for intracytoplasmic T-cell lymphoma-1 (TCL1) (60% of T-cells) (Figure 1, C and D).1 They were negative for CD1a, CD11c, CD13, CD16, CD20, CD25, CD33, CD38, CD56, CD57, CD64, CD79b, CD94, CD117, CD123, CD279 (PD-1), HLA-DR, and granzyme B.
Although it occurs in only 25% of cases, double-positivity for CD4 and CD8 is almost always associated with T-cell prolymphocytic leukemia (T-PLL),2 which, when combined with TCL1 expression, indicates that diagnosis. Moreover, the positivity for CD7 and CD26, combined with the negativity for CD25, was against the diagnosis of Sézary syndrome, as was the absence of CD16, CD56, and CD57, which practically excluded the possibility of T-cell large granular lymphocytic leukemia. Besides, the diagnosis of other peripheral T-cell lymphomas is unlikely given the absence of PD-1 (CD279) and the positivity for TCL1.
Another diagnosis that should be remembered in such scenarios is that of adult T-cell leukemia/lymphoma (ATLL). Although the acute variant of ATLL is distinguished by large lymphoid cells with irregular nuclei and basophilic cytoplasm (sometimes called ‘flower’ cells), there is a chronic form of the disease characterized by small lymphoid cells with nuclear notching and indentations. To complicate matters further, rare cases of ATLL are dual positive for CD4 and CD8.2 Therefore, this chronic variant of ATLL can be confused with Sézary syndrome and with the cerebriform variant of T-PLL. Molecular tests for the DNA of the HTLV-1 virus could help in the differential diagnosis. Unfortunately, this data was not available. Yet, in the present case report, we believe that two combined laboratorial features virtually dismiss the diagnosis of ATLL: (1) The negativity for CD25. Although there are a few cases of ATLL characterized by CD25 negativity (about 9%),3 the disease is almost always marked by strong CD25 positivity;2 (2) The positivity for TCL1. The TCL1 is expressed in many mature B-cell neoplasms (such as, for example, chronic lymphocytic leukemia and mantle cell lymphoma), but it is consistently negative in peripheral T-cell lymphomas.4 In fact, as far as we know, there is only one published case of a patient with the diagnosis of ATLL portraying TCL1 positivity (by immunohistochemistry and fluorescence in situ hybridization/FISH).5 Even so, the case presented a very small percentage of positive TCL1 cells (6.5% by FISH), which is strictly in contrast with the high percentage of T-cells TCL1+ (60%) we found in the cerebriform variant of T-PLL. The fact that only 6.5% of cells were positive for TCL1 suggests that this abnormality may be a secondary cytogenetic change present in a subset of lymphoma cells,5 as opposed to TCL1 expression in T-PLL, where activation of the gene is a primary event following chromosome abnormalities.2
DiscussionT-PLL is a rare, mature T-cell neoplasm that, in blood films, classically presents with small to medium-sized lymphoid cells with a round nucleus and prominent nucleoli, resembling prolymphocytes. However, in approximately 5% of the cases, the aberrant T-PLL cells are characterized by a nucleus exhibiting a peculiar cerebriform morphology (T-PLL, cerebriform variant).2 Although this variant has not been associated with distinct clinical presentations, its cytological features make it frequently confused with Sézary syndrome.
Hence, this case report aims to highlight two crucial laboratorial issues: (1) the importance of remembering that the cerebriform nuclear aspect is not pathognomonic of Sézary syndrome, or more concisely: the presence of Sézary cells is not equivalent to Sézary syndrome. Truly, the term ‘cerebriform’ was originally used by Lutzner and Jordan in 1968 &#¿; as the result of an elegant study in which the ultrastructural features of the cells from blood, lymph node, and skin were analyzed by means of electron microscopy &#¿; to describe the nucleus of the lymphoid cells of three patients with the diagnosis of Sézary syndrome.6 Yet, Sézary cells can be found in many skin diseases (such as psoriasis and vasculitis), B-cell lymphomas, and even in healthy individuals; (2) the importance of routine use of the antibody anti-TCL1, even in situations where the initial diagnostic hypothesis is not T-PLL, but Sézary syndrome, as in the present case.
Author contributionD.M.M performed flow cytometry analysis, reviewed the literature, and wrote the manuscript.
Ethics statementSingle case report. The patients’ anonymity and confidentiality were preserved throughout the article.
This case was diagnosed while I was the medical scientific advisor and the coordinator of the Flow Cytometry Section of the Clementino Fraga Laboratory (Fortaleza, CE, Brazil). For all the support, I am grateful to that institution.
Of note: to prove that, in our case, the TCL1 positivity was true and not the result of some technical problem, we performed the analysis of TCL1 in normal, mature T-CD4+ and T-CD8+ blood lymphocytes from a healthy subject (control), which were negative (data not shown). According to the literature, these populations are in fact TCL1 negative (See reference 4).