Anemia occurs commonly worldwide and at all ages of life1 and, although frequently overlooked, it affects mortality, morbidity and quality of life, even when mild.2,3 The prevalence of anemia varies widely depending on its definition. The World Health Organization has established some cut-off hemoglobin (Hb) levels, stratified by gender and in part by age, to define the presence of anemia.4 For adults, these levels are less than 12g/dL for women and less than 13g/dL for men, although these cut-off points may not be fully appropriate for the elderly.5 Severe anemia has been defined as Hb <8.0g/dL for both genders. However, hemoglobin is a simple surrogate marker for the disease that has provoked anemia. To treat anemias simply restoring a “safer” hemoglobin level (i.e., by means of transfusions or erythropoietin) may be very different than curing them by eliminating the causes that had provoked the condition. Moreover, several reports have shown that both transfusions and erythropoiesis stimulating agents may indeed carry an increased risk of adverse events. Therefore, it is quite surprisingly that in health services, anemia continues to be regarded as a “minor” disease, even when severe, to be assigned to the ambulatory setting in the absence of a robust body of literature to support this common practice.
In Italy, disorders of red blood cells in people older than 17 years [International Classification of Diseases – ninth revision Clinical Modification (ICD-IX-CM) codes 280–285] “outside urgencies” are considered not to be appropriate for hospital admission, regardless of the severity of the Hb deficiency or the presence of important comorbidities, including a reduced functional capacity in older people.6 We believe that to rely on assumptions of this kind in advance of evidence may carry a risk to induce some potentially deleterious consequences, including overuse of blood transfusions to reach an Hb level “safe” for emergency room discharge rather than patient clinical status. Historically, and in current guidelines,7 the indication for transfusion comes from both Hb concentration and the clinical scenario; to transfuse in order to avoid hospital admission should be regarded as unethical.
We conducted an observational, prospective study of all patients admitted to an Internal Medicine ward with very severe anemia, aiming to explore the clinical and assistential burden of severely anemic patients admitted to the hospital. Patients with an Hb concentration of 6g/dL or less were eligible. Those presenting with overt hemorrhage or acute anemia were excluded. Patients were managed as usual, and no diagnostic or therapeutic procedure was performed for study purposes alone. In defining the main diagnosis at discharge, our standard procedure was to select first the procedure that had absorbed the largest amount of resources, accordingly to a predefined hierarchy (Table 1) and then to choose the consequent diagnosis. Accordingly to our laboratory, we defined microcytic anemia as all cases with a mean corpuscular volume (MCV) of less than 81fL, and macrocytic anemia as those with a MCV of more than 98fL and normocytic anemia as all others. Thrombocytopenia was defined as an absolute platelet count of less than 150×109/L; leukopenia as a white blood cell absolute count of less than 4.0×109/L and lymphopenia as an absolute lymphocyte count of less than 1.1×109/L.
Hierarchy of the procedures for International Classification of Diseases (ninth revision) Clinical Modification coding.
| 1. Open surgery |
| 2. Endoscopic surgical procedures |
| 3. Other invasive diagnostic or therapeutic procedures |
| 4. Procedures with closed biopsy of organ or tissues |
| 5. All other diagnostic or therapeutic procedures |
The main outcome of the study was all-cause, in-hospital mortality. Secondary outcomes were one-year mortality and the percentage of admissions for anemia that were lost to a retrospective analysis based only on coding. Continuous variables are expressed as means±standard deviation (SD) or as medians with minimum and maximum values when data did not have a normal distribution; categorical data are given as counts and percentages. The Institutional Review Board approved the study, which was carried out and is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies.8
Between October 2009 and June 2015, 86 patients were admitted for very severe anemia. Of these, 61 (71%) were women and 25 (29%) were men; eight patients (9.3%) came from nursing homes, one from a prison and the remaining cases were from home. The mean age was 76.8±15.6 (range: 33–100). Seventy-one patients (82.5%) were 65 years or older. Nine of the patients (six women and three men) died during hospitalization (10.5%); the remaining 77 patients were discharged and followed up for about 170 patient-years. Deceased patients were older than discharged patients: mean age was 90±10 vs. 75.5±15.7 (p-value <0.01). During the same period, general in-hospital mortality was 12.3%. Mean follow-up was 806 days (range: 16–2072 days) during which time 32 more patients died. Mean time to death was 412 days. The cumulative percentages of death at 1, 3 and 12 months were 3.9%, 13.0% and 29.9%, respectively. When in-hospital mortality was included and added to one-month mortality, the corresponding figures became 13.9%, 22.1% and 37.2%. Hematological data are shown in Table 2. There were no significant differences in mean Hb and MCV, or in the presence of cytopenias other than anemia. However, discharged patients more often had microcytic anemias (54.5%) compared to deceased patients, whose anemias were more often normocytic or macrocytic (77.8%). Patients with a normocytic anemia had an increased risk to die in the hospital when compared with those with microcytic anemia (OR 7.5; 95% confidence interval: 1.3–43.1; p-value <0.05). Lymphopenia, a surrogate marker for hyponutrition, was more prevalent in deceased patients (44.4% vs. 32.5%).
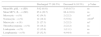
Hematological data.
| Discharged 77 (89.5%) | Deceased 9 (10.5%) | p-Value | |
|---|---|---|---|
| Mean Hb, g/dL – n (SD) | 5.02 (0.81) | 5.43 (0.71) | ns |
| Mean MCV, fL – n (SD) | 85.4 (20.7) | 88.4 (16.6) | ns |
| Microcytic – n (%) | 42 (54.5) | 2 (22.2) | nsa |
| Normocytic – n (%) | 14 (18.2) | 5 (55.6) | <0.05b |
| Macrocytic – n (%) | 21 (27.3) | 2 (22.2) | nsc |
| Thrombocytopenia – n (%) | 14 (18.2) | 2 (22.2) | ns |
| Leukopenia – n (%) | 12 (15.6) | 1 (11.1) | ns |
| Lymphopenia – n (%) | 25 (32.5) | 4 (44.4) | ns |
A total of 295 units of packed red cells were transfused to the 77 discharged patients (mean: 3.8), and 29 units to the nine deceased patients (mean: 3.2). One patient who died refused blood transfusions because of religious beliefs. Patients discharged alive were submitted to 77 invasive procedures: 39 to esophagogastroduodenoscopy, 23 to colonoscopy, four to capsular videoendoscopy (preceded by radiologic study of gastrointestinal tract in all four cases) and 11 to bone marrow biopsies. Administrative data was complete for 85 cases (98.8%). Diagnosis Related Groups (DRG) according to the ICD-IX-CM coding are shown in Table 3; three were surgical, and the remaining were clinical. Only 31/85 cases were coded as DRG 395 (red blood cell disorders – age >17), so about 63% of patients admitted for anemia would have been lost if this survey had been conducted retrospectively on discharge data. The mean reimbursement was 3165 euros.
Diagnosis Related Groups (DRG) accordingly to International Classification of Diseases (ninth revision) Clinical Modification coding.
| DRG | Type | Number of cases |
|---|---|---|
| 12 - Degenerative nervous system disorders | MED | 1 |
| 14 - Intracranial hemorrhage or cerebral infarction | MED | 1 |
| 122 - Circulatory disorders W AMI W/O major comp, discharged alive | MED | 1 |
| 123 - Circulatory disorders W AMI, expired | MED | 1 |
| 135 - Cardiac congenital & valvular disorders age >17W CC | MED | 1 |
| 138 - Cardiac arrhythmia & conduction disorders W CC | MED | 1 |
| 142 - Syncope & collapse W/O CC | MED | 1 |
| 144 - Other circulatory system diagnoses W CC | MED | 1 |
| 172 - Digestive malignancy W CC | MED | 6 |
| 174 - Gastrointestinal hemorrhage W CC | MED | 8 |
| 179 - Inflammatory bowel disease | MED | 1 |
| 180 - Gastrointestinal obstruction W CC | MED | 1 |
| 182 - Esophagitis, gastroent & misc digest disorders age >17W CC | MED | 4 |
| 188 - Other digestive system diagnoses AGE >17W CC | MED | 1 |
| 189 - Other digestive system diagnoses age >17 W/O CC | MED | 1 |
| 190 - Other digestive system diagnoses age 0–17 | MED | 1 |
| 239 - Pathological fractures & musculoskeletal & conn tiss malignancy | MED | 1 |
| 271 - Skin ulcers | MED | 1 |
| 304 - Kidney, ureter & major bladder proc for non-neopl W CC | SURG | 1 |
| 310 - Transurethral procedures W CC | SURG | 1 |
| 316 - Renal failure | MED | 2 |
| 395 - Red blood cell disorders age >17 | MED | 31 |
| • Iron deficiency anemia | 19 | |
| • Secondary or not specified anemia | 6 | |
| • Myelodysplasia | 2 | |
| • Pancytopenia | 2 | |
| • Megaloblastic anemia | 2 | |
| 397 - Coagulation disorders | MED | 2 |
| 403 - Lymphoma & non-acute leukemia W CC | MED | 2 |
| 473 - Acute leukemia W/O major O.R. procedure age >17 | MED | 1 |
| 570 - Major small & large bowel procedures W CC W/O major GI DX | SURG | 1 |
| 571 - Major esophageal disorders | MED | 1 |
| 574 - Major hematologic/immunologic dx excep sickle cell crisis & coag | MED | 6 |
| 576 - Septicemia w mechanical ventilator w/0 96+ hours age >17 | MED | 4 |
| All | 85 |
In this preliminary study, we report data on a sample of 86 consecutive, unselected elderly patients (82.5% of whom were 65 years or older). In-hospital mortality was 10.5%, but more than one third of these patients eventually died within a year after the index admission. Discharged patients, as compared with those who died in the hospital, had microcytic anemias more often (54.5% vs. 22.2%). Conversely, deceased patients had a high prevalence of normocytic anemias (18.2% vs. 55.6%). We speculate that microcytic anemia could have been more often the expression of a single and possibly curable disease, whereas normocytic anemias should be the result of multiple comorbidities that played the main role in causing death. In our study, we demonstrated that very severe anemia is not a benign condition with high mortality, and we question the advisability of hospitalization. In many cases anemia could be managed without transfusions (i.e., iron and vitamin B12 deficiency, chronic renal insufficiency, myelodysplasia and chemotherapy-related anemia), but this is often impossible without patient monitoring, and there is a risk of overuse of blood transfusions in this kind of patient in order to discharge them from the Emergency Department. To clarify this issue there is a need for prospective, randomized studies; indeed in our cohort, 63% of discharge diagnoses were not in the DRG 395 group, and would have been missed if we conducted an investigation based on administrative data only. We acknowledge some limitations of this study beyond its observational nature. This is a single-center experience, and results may not be reproducible in other contexts. However, we recruited all consecutive patients with very severe anemia over a period of more than five years, and we excluded only patients with acute anemia from bleeding. Furthermore, with about 170 patient-years of observation, we think that data on mortality are sufficiently robust. We enrolled patients on the basis of an arbitrary threshold of Hb that we defined as “very severe”. Indeed, 33 patients had Hb less than 5.0g/dL, and 13 less than 4g/dL, values that should be regarded as life threatening, especially in old, comorbid patients. There is little doubt that if we chose a more permissive approach (i.e., an Hb level of 7.0–8.0g/dL), we would have recruited a wider sample of patients. To study patients with less severe anemia however, was not in our interest, since we focused on the prognosis of patients for whom there are scarce data in the literature. Our patients were transfused with three to four units of packed red cells each. Due to the observational design of the study, we were not able to elucidate if there was a detrimental effect of transfusions on patient outcomes. Finally, we did not evaluate the impact of comorbidities on mortality in this cohort of patients, but we are planning a follow-up study to address this important question.
Conflicts of interestThe authors declare no conflicts of interest.