Children with sickle cell disease may have their quality of life affected by oral alterations. However, there is still little data on oral health-related quality of life in these children. The aim of this study was to investigate the influence of sickle cell disease, socioeconomic characteristics, and oral conditions on oral health-related quality of life of children and teens.
MethodOne hundred and six children and teens with sickle cell disease were compared to a similar sample of 385 healthy peers. Data were collected through oral examinations, interviews to assess quality of life (Child Perceptions Questionnaire for children aged 8–10 and 11–14) and questionnaires containing questions on socioeconomic status.
ResultsThere were no statistically significant differences in the total scores of the Child Perceptions Questionnaires or domain scores comparing sickle cell disease patients to control subjects. When sub-scales were compared, oral symptoms and functional limitations had a greater negative impact on the quality of life of adolescents with sickle cell disease (p-value <0.001 and p-value <0.01, respectively) when compared to healthy controls. The only statistically significant determinants of negative impact on oral health-related quality of life in the overall sample was home overcrowding (more than two people/room) in the younger children's group, and dental malocclusion among teens.
ConclusionThere was no significant difference in the negative impact on the oral health-related quality of life between the group with sickle cell disease and the control group. Of the oral alterations, there was a significant difference in the oral health-related quality of life between adolescents with sickle cell disease and controls only in relation to malocclusion. Among the socioeconomic characteristics, only overcrowding was significantly associated with a negative impact on oral health-related quality of life.
Sickle cell disease (SCD) is an inherited autosomal recessive blood disease. The inheritance of one sickle cell gene from each parent (SS) is the most common and the severest form of the disease, affecting around 280,000 newborns per year. This disease, in addition to thalassemia, is responsible for 3.4% of all deaths of children under five years of age.1 Each year, 3500 children in Brazil are born with SCD.2
Children with SCD are at risk for serious morbidities related to vascular occlusion, hemolysis, and infection, which can impair their quality of life (QoL) and lead to early death. The pathological effects of SCD, seen in mineralized connective tissues, also occur in dental tissues and the oral cavity, usually in late childhood and during adolescence.3 The most commonly described findings in the oral cavity, which are not pathognomonic but may be characteristic of the disease, are pallor of the oral mucosa due to a low hematocrit and depapillated tongue.4 There are reports of delayed tooth eruption, hypoplasia and hypomineralization, hypercementosis, pulp stones and asymptomatic pulp necrosis due to thrombosis in the blood vessels.5–7
Individuals with SCD experience a lower QoL compared to healthy peers.8,9 Due to the clinical course of the disease, SCD is thought to affect the QoL in multiple dimensions. The most serious organic changes result in emotional and physical stress for children and their families.10 The frequency of episodes of fever, hospitalizations, and pain can trigger anger and sadness.11 Moreover, lower health-related QoL in children with SCD is associated with a socioeconomic disadvantage,12 a low level of education and not living with both biological parents.13 Religion and spirituality have been identified by individuals with SCD as an important factor in coping with stress and in determining the QoL.14
QoL may be affected by oral conditions. Oral conditions such as dental caries and malocclusions affect self-esteem, the ability to chew and speak, and may be associated with absenteeism from school and psychological problems.15,16 Although there have been studies on the QoL of patients with hematological diseases with regard to their behavioral and psychological impacts, emphasis on oral health has remained relatively underexplored. Only recently, the oral health-related QoL (OHRQoL) of 54 teenagers with SCD was evaluated by an adolescent medicine clinic in Columbus, Ohio, comparing them with adolescents with other chronic diseases. There was no statistically significant difference in the OHRQoL between the two groups.17
The objective of this study was to investigate the influence of SCD and factors related to the disease, oral conditions, resources and individual characteristics on the OHRQoL of children with this disease.
MethodsEthical approvalThis study received approval from the Ethics Committees of the Fundação de Hematologia e Hemoterapia do Estado de Minas Gerais (Hemominas) and the Universidade Federal de Minas Gerais (UFMG), Brazil. Written informed consent was obtained from the participants or parents/guardians of the participants of this study. This research was conducted in accordance with the Helsinki Declaration as revised in 2008.
Participants and recruitmentThe study was conducted in the city of Belo Horizonte, the capital of the state of Minas Gerais, Southeast Brazil. The study sample was made up of children with SCD, residing in the metropolitan region of Belo Horizonte, aged from 8 to 14 years old, sampled from the patient registry of the referral center, Hemominas. A control group of healthy children and teens was recruited from the same schools attended by the children with SCD. A total of 450 children and adolescents with SCD aged 8–14 years were registered as receiving services from Hemominas in 2012. Among these, 196 children and teenagers resided in the metropolitan region of Belo Horizonte.18
The sample size was calculated from the expected standard deviations (SDs) of the QoL scales to evaluate the OHRQoL: the Child Perceptions Questionnaire for children aged 8–10 (CPQ8–10) (SD=10.7) and 11–14 years (CPQ11–14) (SD=10.1) investigated in a pilot study. The pilot study was conducted using a random sample of 34 children and 35 teens with SCD registered in Hemominas. The required sample size (n=51 children aged 8–10 years, and n=45 adolescents aged 11–14 years) was calculated based on the ability to detect a five-point difference in QoL scores on comparing SCD patients to apparently healthy controls, assuming an α=0.05 and β=0.10. The program SPSS version 20.0 was used for all statistical analyses. One hundred and eighty healthy adolescents and 205 healthy younger children who were enrolled at the same schools and in the same classes as those with SCD were selected, and matched by age and gender. The option to match one case to at least every three controls was because healthy controls could be less motivated to participate than individuals in a health-care setting.19
Eligibility criteria for inclusion in the SCD group were as follows: diagnosis of SCD hemoglobin (Hb) SS in their medical records, not suffering from a painful crisis at the time of the survey, no medical conditions other than SCD, no emergency dental appointment within the previous three months and no intellectual disability. Eligibility of the members of the control group included: no organic, physiological, or psychiatric disorders and no intellectual disability, apparently healthy with no dental appointment within the previous three months.
Calibration exercisePrior to the fieldwork, the examiner was calibrated and trained in respect to the diagnosis of oral diseases (dental caries and malocclusion). This consisted of two stages. The theoretical stage involved a discussion of the criteria for diagnosis of oral alterations. The second stage involved an oral clinical examination of children and adolescents not included in the study. Participants were examined in two sessions with a nine-day interval between. Data analysis involved the calculation of Kappa coefficients for inter-examiner agreement (malocclusion: k=0.91; dental caries: k=0.92; gingival bleeding: k=0.89) and intra-examiner agreement (malocclusion: k=0.92; dental caries: k=0.92; gingival bleeding: k=0.91). The test–retest of instruments was also carried out. At this stage, the participants answered the appropriate instrument for age (CPQ8–10 or CPQ11–14) in two sessions at an interval of nine days. The agreement value obtained for both instruments was a Kappa=0.82.
Clinical oral examinationDental examinations of patients with SCD were performed at Hemominas and healthy controls were examined in schools. A qualified dentist performed an intra-oral exam on each patient using a disposable mirror, community periodontal index (CPI) probes and gauzes. The World Health Organization (WHO)20 norms were used to evaluate the following: the Decayed, Missing and Filled Teeth index (DMFT), the Dental Aesthetic index (DAI) and the Gingival index. The DAI identifies clinical and aesthetic components and mathematically derives a single score. This score has been found to be significantly associated with the perception of treatment needed by students and parents.20 The research team was made up of one dentist and four trained and certified dental researchers.
Non-clinical examinationThrough interviews with parents, information was gathered on socioeconomic aspects, religiosity (never, sometimes, frequently), race (White, Black, other), children living with both parents and medical information (disease severity, age at diagnosis of SCD). The following socioeconomic aspects were evaluated: home overcrowding (number of people/room), years of schooling of the mother and father, house ownership, car ownership, family income (US$/month).
Oral health-related quality of life instrumentThe Brazilian version of the Child Perceptions Questionnaires (CPQ) for children aged 8–10 years (CPQ8–10)21 and for children aged 11–14 years (CPQ11–14)21 were used to assess the OHRQoL. These questionnaires were translated and validated for the Brazilian population, and proved to have good psychometric properties. The CPQ8–10 contains 25 questions21 and the short version of the CPQ11–1422 contains 16 questions. The instruments encompass four health domains: oral symptoms, functional limitations, emotional well-being, and social well-being related to oral health conditions. These are two of the four questionnaires comprising the OHRQoL measures developed by Jokovic et al.23 All items consider the frequency of events in relation to the condition of the mouth and teeth over the previous three months. The responses to questions were scored on a frequency scale using the following response options and associated codes: ‘Never=0’; ‘Once/twice=1’; ‘Sometimes=2’; Often=3’, and ‘Everyday/Almost every day=4’. The questionnaires also contained two single-item global ratings. The CPQ sub-scale scores were calculated by summing responses. The overall CPQ8–10 score, which may range from 0 to 100, and the overall CPQ11–14 score, which may range from 0 to 64, was the sum of all domain scores. Higher scores translate to a greater negative OHRQoL.
Statistical analysisDescriptive and univariate analyses were performed separately for the overall sample (SCD and healthy children and adolescents) and only for SCD patients (children and adolescents). The responses to categorical questions by each group were compared using either the Chi-square test or the Fisher's exact test for contingency tables with small cell counts. The nonparametric Mann–Whitney test was used to compare medians of continuous variables between the SCD and control groups. The age, gender and school location, which were recorded at the time of the interview, were controlled in the multivariable linear regression analyses of OHRQoL.
ResultsExcellent inter-rater reliability was found for the oral exams: Kappa value=0.89 (inter-examiner) and Kappa value=0.92 (intra-examiner). The correlation of responses to interviews was also tested (Kappa value=0.82). The agreement in the recalibration of clinical exams, which was carried out every two months, consistently achieved a Kappa value ≥0.87.
The response rate was 100% in both case and control groups. In the SCD group, there were 106 participants: 56 children (31 boys and 25 girls) with an average age of 8.9 (SD=0.87) years and 50 teens (30 boys and 20 girls) with an average age of 12 (SD=1.08) years. There were 385 individuals in the control group. In this group, there were 205 children (112 boys and 93 girls) with an average age of 8.9 (SD=0.8) years and 180 adolescents (106 boys and 74 girls) with an average age of 11.9 (SD=1.0) years.
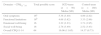
In the group of children (Table 1), both maternal and paternal educational levels were lower in the SCD group (p-value <0.001 and <0.01 respectively). More children with SCD came from homes with no car (p-value <0.01). Malocclusion (DAI) was worse in children with SCD (p-value <0.001). However, dental caries (DMFT) were more prevalent in the children in the control group (p-value <0.05). In the group of children (aged 8–10 years), there were no statistical differences in total scores of the CPQ8–10 or domain scores when SCD individuals were compared to control subjects (Table 2).
Descriptive and comparative analysis of individual characteristics, factors related to the disease, resources, oral conditions, and negative impact on oral health-related quality of life between children suffering from sickle cell disease (SCD) and the control group.
| Children SCD (n=56) | Children control group (n=205) | |
|---|---|---|
| Individual characteristics | ||
| Gender – n (%) | ||
| Male | 31 (55.3) | 112 (54.6) |
| Female | 25 (44.7) | 93 (45.4) |
| Child living with biological parents – n (%) | ||
| No | 21 (41.1) | 46 (29.0) |
| Yes | 30 (58.9) | 113 (71.0) |
| Factors related to the disease | ||
| Religiosity – n (%) | ||
| No | 6 (10.7) | |
| Sometimes | 7 (12.5) | |
| Frequently | 43 (76.8) | |
| Race – n (%) | ||
| White | 9 (16.0) | |
| Black | 19 (34.0) | |
| Mixed | 28 (50.0) | |
| Age at diagnosis of SCD – n (%) | ||
| <7 months old | 52 (95.5) | |
| 7 months – 3 years | 3 (5.0) | |
| Socioeconomic factors | ||
| Home overcrowding – n (%) | ||
| ≤2 people/room | 32 (57.0) | 101 (49.3) |
| >2 people/room | 24 (43.0) | 104 (50.7) |
| Mother's educationa – n (%) | ||
| ≤8 years | 44 (86.0) | 99 (66.5) |
| >8 years | 7 (14.0) | 57 (36.5) |
| Father's educationa – n (%) | ||
| ≤8 years | 35 (83.0) | 89 (60.5) |
| >8 years | 7 (17.0) | 58 (39.5) |
| Own house – n (%) | ||
| No | 32 (63.0) | 100 (62.9) |
| Yes | 19 (37.0) | 59 (37.1) |
| Own cara – n (%) | ||
| No | 47 (92.0) | 117 (73.6) |
| Yes | 4 (8.0) | 42 (26.4) |
| Family income US$/month – mean (SD) | 584.4 (245.2) | 615.8 (274.7) |
| Oral conditions | ||
| DMFT/DMFT – mean (SD)b | 1.3 (2.1) | 1.8 (2.0) |
| Decayed – mean (SD) | 0.9 (1.8) | 1.1 (1.5) |
| Missing – mean (SD) | 0 | 0.2 (0.6) |
| Filled – mean (SD) | 0.4 (1.2) | 0.5 (1.0) |
| DAIc | 32.2 (10.6) | 25.5 (7.4) |
| Gingival bleeding – n (%) | ||
| No | 47 (84.0) | 182 (88.8) |
| Yes | 9 (16.0) | 23 (11.2) |
SD: standard deviation.
The Child Perceptions Questionnaire subscales for 8 to 10-year-old sickle cell disease (SCD) children and controls (CPQ8–10).
| Maximum score | Children SCD (n=56) Mean (SD) | Children control group (n=205) Mean (SD) | |
|---|---|---|---|
| Score CPQ8-10 | 100 | 14.5 (12) | 17.9 (15) |
| Oral symptoms | 20 | 5.5 (3.6) | 5.9 (3.8) |
| Functional limitation | 20 | 2.8 (3.1) | 3.5 (4.7) |
| Emotional well-being | 20 | 3.3 (4.5) | 3.9 (4.7) |
| Social well-being | 40 | 2.9 (3.6) | 4.6 (6.2) |
SD: standard deviation.
In the group of teens (Table 3), individuals with SCD were less likely to be living with both biological parents when compared to healthy controls (p-value <0.001). The family income (US$/month) was higher in the group of adolescents with SCD (p-value <0.001). Both maternal and paternal education levels were higher in the group of teenagers with SCD (p-value <0.001). History of gum bleeding was more frequent in the group of teens with SCD (p-value <0.001). However, there were no statistically significant differences in total scores of the OHRQoL between healthy and SCD adolescents. When the sub-scales were compared, oral symptoms and functional limitations had a greater negative impact on the QoL of adolescents with SCD (p-value <0.001 and <0.01, respectively) when compared to healthy controls (Table 4).
Descriptive and comparative analysis of individual characteristics, factors related to the disease, resources, oral conditions, and negative impact on oral health-related quality of life between teenagers suffering from sickle cell disease (SCD) and the control group.
| Teens SCD (n=50) | Teens control-group (n=180) | |
|---|---|---|
| Individual characteristics | ||
| Gender – n (%) | ||
| Male | 30 (60.0) | 106 (58.9) |
| Female | 20 (40.0) | 74 (41.1) |
| Child living with biological parentsa – n (%) | ||
| No | 30 (73.0) | 56 (38.9) |
| Yes | 11 (27.0) | 88 (61.1) |
| Factors related to the disease | ||
| Religiosity (frequent church) – n (%) | ||
| Never | 9 (18.0) | |
| Sometimes | 14 (28.0) | |
| Frequently | 27 (54.0) | |
| Race – n (%) | ||
| White | 6 (12.0) | |
| Black | 19 (38.0) | |
| Mixed | 25 (50.0) | |
| Age at diagnosis of SCD – n (%) | ||
| <7 months old | 47 (94.0) | |
| 7 months – 3 years | 3 (6.0) | |
| Socio-economic factors | ||
| Home overcrowding – n (%) | ||
| <2 people/room | 25 (64.0) | 90 (62.0) |
| >2 people/room | 14 (36.0) | 55 (38.0) |
| Mother's educationa – n (%) | ||
| ≤8 years | 22 (58.0) | 132 (91.7) |
| >8 years | 16 (42.0) | 12 (8.3) |
| Father's educationa – n (%) | ||
| ≤8 years | 14 (61.0) | 120 (83.3) |
| >8 years | 9 (39.0) | 24 (16.7) |
| Own house – n (%) | ||
| No | 31 (76.0) | 91 (85.9) |
| Yes | 10 (24.0) | 53 (14.1) |
| Own car – n (%) | ||
| No | 40 (98.0) | 128 (88.9) |
| Yes | 2 (1.0) | 18 (11.1) |
| Family income US$/month (mean±SD)a | 1463 (671) | 628 (257) |
| Oral conditions | ||
| DMFT/DMFT – mean (SD)b | 1.5 (1.9) | 2.1 (2.8) |
| Decayed – mean (SD) | 1.0 (1.4) | 1.0 (1.7) |
| Missing – mean (SD) | 0.1 (0.6) | 0.2 (0.7) |
| Filled – mean (SD) | 0.4 (0.8) | 0.8 (1.7) |
| DAI | 32 (10.3) | 29.2 (10.6) |
| Gingival bleedinga – n (%) | ||
| No | 23 (46.0) | 152 (84.4) |
| Yes | 27 (54.0) | 28 (15.6) |
SD: standard deviation.
The Child Perceptions Questionnaire subscales for 11 to 14-year-old sickle cell disease (SCD) teens and controls (CPQ11–14).
| Domains – CPQ11–14 | Total possible score | SCD teens (n=50) Media (SD) | Control teens (n=180) Media (SD) |
|---|---|---|---|
| Oral symptoms | 16a | 5.38 (3.40) | 4.89 (2.82) |
| Functional limitations | 16b | 4.68 (3.62) | 3.33 (2.96) |
| Emotional well-being | 16 | 3.22 (3.23) | 3.71 (3.95) |
| Social well-being | 16 | 2.78 (3.49) | 2.52 (3.43) |
| Overall CPQ11-14 | 64 | 16.06 (11.65) | 14.37 (9.73) |
SD: standard deviation.
Tables 5 and 6 show the results of multivariable-adjusted linear regression. Table 5 shows the results of combined analyses of SCD patients and healthy controls. In both younger children and adolescents, a diagnosis of SCD was not associated with a negative impact on OHRQoL. The only statistically significant determinants (p-value <0.05) of a negative impact on OHRQoL in the overall sample was home overcrowding (more than two people/room) for the younger children's group, and dental malocclusion (DAI) among teens.
Beta coefficients of the negative impact on the oral health-related quality of life (OHRQoL) in children and teens with sickle cell disease (SCD) and control group by individual characteristics, factors related to the disease, resources, and oral conditions.
| CPQ score (negative impact on OHRQoL) | Children SCD (n=56) Controls (n=205) | Teens SCD (n=50) Controls (n=205) | ||
|---|---|---|---|---|
| Predictors | β | SE | β | SE |
| Individual characteristics | ||||
| Age (in years) | −1.35 | 1.2 | −0.64 | 0.83 |
| Gender boy (0/1) | 0.197 | 2.03 | 2.34 | 1.72 |
| Child living with both biological parents: No-0/Yes-1 | −3.36 | 2.54 | 2.31 | 1.94 |
| Factors related to the disease | ||||
| SCD (0/1) | −4.80 | 2.60 | −2.41 | 3.69 |
| Resources | ||||
| Family income (US$/month) | 0.004 | 0.004 | 0.003 | 0.89 |
| Home overcrowding (>2 people/room): No/Yes | 9.56 | 2.51a | 2.26 | 1.73 |
| Mother education: >8/≤8 years | −1.33 | 2.43 | −0.156 | 2.75 |
| Father education: >8/≤8 years | −0.474 | 2.4 | −3.05 | 2.27 |
| Own house: No/Yes | 0.629 | 2.46 | −0.09 | 1.81 |
| Own car: No/Yes | 0.302 | 2.65 | 2.61 | 1.15 |
| Oral conditions | ||||
| DAI | 0.128 | 0.148 | 0.165 | 0.08* |
| DMFT | 0.133 | 0.57 | 0.57 | 0.04 |
| Gum bleeding: No-0/Yes-1 | 0.4 | 2.83 | 0.88 | 2.03 |
CPQ: Child Perceptions Questionnaire; β: beta coefficient; SE: standard error.
Beta coefficients of the score with a negative impact on oral health-related quality of life (OHRQoL) in children and teens suffering from sickle cell disease (SCD) by individual characteristics, factors related to the disease, resources, and oral conditions.
| Score CPQ (negative impact on OHRQoL) | Children SCD (n=56) | Teens SCD (n=50) | ||
|---|---|---|---|---|
| Predictors | β | SE | β | SE |
| Individual characteristics | ||||
| Age (in years) | 2.81 | 1.89 | 7.88 | 4.11 |
| Gender boy (0/1) | −1.33 | 2.86 | 9.66 | 7.88 |
| Child living with both biological parents: No/Yes | −2.36 | 3.45 | 19.92 | 7.46 |
| Factors related to the disease | ||||
| Religiosity: Never/Sometimes/Frequently | −8.96 | 3.73a | −21.09 | 10.78a |
| Race: White/Mixed/Black | −4.52 | 2.12a | −4.18 | 4.37 |
| Age at diagnosis SCD: <7 months old/7 months–3 years | 6.59 | 10.2 | 1.034 | 7.03 |
| Disease severity | 1.62 | 0.95 | 1.192 | 2.58 |
| Resources | ||||
| Family income (US$/month) | −.006 | 0.06 | −0.016 | 0.009 |
| Home overcrowding (>2 people/room): No/Yes | 0.941 | 3.48 | 16.7 | 7.43 |
| Mother education: >8/≤8 years | −2.99 | 5.89 | −10.2 | 10.35 |
| Father education: >8/≤8 years | −4.1 | 5.83 | −15.09 | 8.86 |
| Own house: No/Yes | −2.2 | 3.15 | −6.99 | 10.47 |
| Own car: No/yes | −3.37 | 4.66 | 7.92 | 23.47 |
| Oral conditions | ||||
| DAI | 0.36 | 0.2 | 0.048 | 0.31 |
| DMFT | 0.27 | 0.88 | 5.049 | 2.32 |
| Gum bleeding: No/Yes | 5.41 | 4.36 | 13.99 | 10.31 |
CPQ: Child Perceptions Questionnaire; β: beta coefficient; SE: standard error.
Table 6 presents the findings restricted to SCD patients, stratified by age group. Among the younger children, the only factors that were significantly associated with a negative impact on the OHRQoL were religiosity and race (with Black people having a higher QoL). No clinical factors were associated with a negative impact on the OHRQoL in the group of teens with SCD; the only factor related to a negative impact on the OHRQoL was religiosity, the frequency of church attendance (p-value <0.05). Living with both biological parents was marginally associated with a negative impact on the OHRQoL, but in an unexpected direction; children living with only one parent reported higher QoL (p-value=0.056).
DiscussionIn this study, an overall negative impact of SCD on the OHRQoL was not found. Clinical dental characteristics such as a history of gingival bleeding and experience with caries did not adversely affect the OHRQoL with the only exception being malocclusion (DAI) among adolescents. The main determinant of the OHRQoL was a socioeconomic factor (home overcrowding).
To the best of our knowledge, there is no reported data about the impact of malocclusion on the OHRQoL in SCD patients. In these patients, bone marrow hyperplasia causes a depression of the nasal bridge, midfacial overgrowth and malocclusion.24,25 The craniofacial bone abnormalities can determine the existence of dental malocclusion and the development of abnormalities of the teeth and arches, which cause aesthetic discomfort in the mildest cases and functional disorders or disabilities in the most severe cases.5,26,27 Despite the high frequency of craniofacial bone abnormalities and dental malocclusion among SCD patients, there is insufficient evidence to show that this disease is a risk factor for the occurrence of these clinical manifestations.28
In this study, SCD children and adolescents did not have a more negative overall profile of QoL when compared to the control group. Although this finding is somewhat unexpected, it agrees with previously reported results.18 The reason given in the previous study was that the control group also suffered from chronic diseases. In contrast, the control group of this study was composed strictly of apparently healthy children and adolescents. An interpretation of this finding is that children and adolescents with SCD are resilient, and that they adjust psychologically to their condition. Indeed, the main determinants of OHRQoL in this study were background socioeconomic circumstances (home overcrowding), religiosity, and aesthetic concerns (malocclusion) among teens.
Socioeconomic disadvantage impacts QoL by making access to health care more difficult.12 According to a study conducted with a convenience sample of African-American children with SCD, the OHRQL was correlated to family income.9 In contrast, a significant association between socioeconomic variables and OHRQL in children with SCD was not observed in this study. This result may be justified by the access to medical monitoring, as well as to treatment at the SCD health center. Monitoring and treatment results in better health care and consequently less impact on the OHRQL.
The results show that practicing a religion is protective in maintaining the OHRQoL in both children and adolescents with SCD. Religion and spirituality have been previously reported by individuals with SCD as an important factor in coping with stress and in determining QoL.29,30 Involvement in a religion is an important means of individual coping, as well as a means of receiving social support from others.31
Comparisons between the findings obtained in this study and other studies need to be viewed with a degree of caution as most of these studies are based on small, convenience samples recruited in clinical settings. Although population-based studies can and have been used to compare the impact of common conditions such as dental decay, malocclusion and gingival bleeding in random samples of children, SCD is not as prevalent and recruitment from the clinics in which they are treated remains the only feasible option. Moreover, this cross-sectional design cannot address the trajectories of QoL over time and across the life course of SCD patients. Further studies with longitudinal follow-up of patients are needed. The use of OHRQoL should be considered an important tool in the clinical practice, and an invaluable guide to assess the psychosocial functioning of young patients affected with SCD.
There was no significant difference in negative impact on OHRQoL between the SCD and control groups. Of the oral alterations, there was a significant difference in the OHRQoL between adolescents with SCD and controls only in relation to malocclusion. Among the socioeconomic characteristics, only overcrowding was significantly associated with the negative impact on OHRQoL.
FundingThis study received support from the National Council for Scientific and Technological Development (CNPq), Ministry of Science and Technology, the State of Minas Gerais Research Foundation (FAPEMIG), Brazil, and the Lemann Institute, Brazil.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank Hemominas.