Acute Lymphoblastic Leukemia (ALL) remains the most common malignant disease of childhood, accounting for approximately 26% of pediatric oncology diagnoses. Modern treatment approaches, particularly multi-agent chemotherapy regimens such as the BFM protocol, have significantly improved 5-year survival rates, reaching up to 96%. However, the toxicity of chemotherapy regimens, particularly late effects, negatively impacts long-term quality of life and clinical outcomes. These adverse effects include cardiotoxicity, secondary malignancies, endocrine dysfunction, and neurological damage. Given the limitations of conventional treatment protocols, exploring less toxic and more effective therapeutic strategies is of critical importance.
Objective• To identify the late effects of chemotherapy in pediatric patients treated for ALL.
• To propose effective strategies for the early detection and management of these effects.
• To compare the BFM protocol applied in Azerbaijan with international experiences.
Materials and methodsThis study includes 120 pediatric patients diagnosed with ALL and treated at the National Hematology Center of Azerbaijan between 2020 and 2023. A retrospective analysis of patient records was conducted. The evaluation of late chemotherapy effects was performed using internationally standardized methodologies:
• Cardiotoxicity: Echocardiography and pro-BNP biomarker measurements.
• Neurotoxicity: Clinical neurological assessment and electrophysiological testing.
• Endocrine dysfunction: Thyroid function tests, insulin resistance evaluation, and growth hormone monitoring.
• Secondary malignancies: Long-term follow-up and biomolecular analyses.
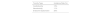
ResultsAmong the analyzed patients, 38% exhibited various late-onset adverse effects. The incidence rates of key toxicity types were as follows:
ConclusionThis study demonstrates the significant late effects of chemotherapy in pediatric patients treated with the BFM protocol in Azerbaijan. The findings emphasize the importance of implementing routine monitoring mechanisms, particularly for cardiotoxicity and endocrine dysfunction. International literature suggests that incorporating novel therapeutic agents, such as CAR-T cell therapy and targeted therapies like blinatumomab, into treatment regimens may improve clinical outcomes.