Elderly patients present clinical and functional heterogeneity. Thus the chronological age (60 years and older) alone does not characterize this group of individuals correctly. Performance status scales such as the Karnofsky Performance Scale (KPS)1 or Eastern Cooperative Oncologic Group Scale (ECOG),2 are used by hematologists in decision making for elderly patients with cancer. Good performance status is defined as a KPS equal to or greater than 80% or an ECOG less than 2. These scores are one of the criteria utilized to choose the treatment strategy for elderly patients with acute myeloid leukemia (AML). AML is more frequent in the aged. Considering the high risk of toxicity during AML treatment in elderly patients, many researchers have recommended the application of geriatric instruments at baseline and in the follow up of these individuals. The objective of this paper is to improve the understanding of how geriatric approaches may benefit the performance status assessment of elderly patients with AML. Two cases, as clinical challenges, are used to exemplify this clinical context.
Clinical challengesCase 1 – Patient 1: 75-year-old man with de novo AML, normal karyotype, KPS of 90% and ECOG of 1
Case 2 – Patient 2: 65-year-old woman with de novo AML, normal karyotype, KPS of 80% and ECOG of 1
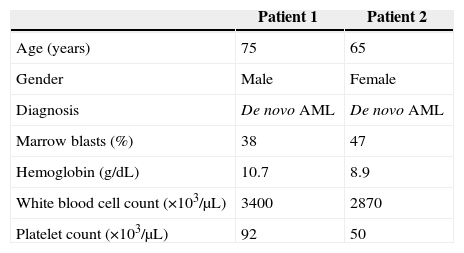
Question: How do geriatric instruments improve the characterization of these patients? (Table 1).
Hematologic data of clinical challenge patients.
| Patient 1 | Patient 2 | |
|---|---|---|
| Age (years) | 75 | 65 |
| Gender | Male | Female |
| Diagnosis | De novo AML | De novo AML |
| Marrow blasts (%) | 38 | 47 |
| Hemoglobin (g/dL) | 10.7 | 8.9 |
| White blood cell count (×103/μL) | 3400 | 2870 |
| Platelet count (×103/μL) | 92 | 50 |
AML: acute myeloid leukemia.
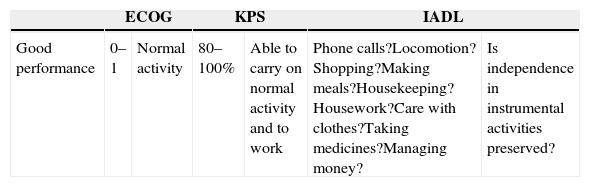
Performance status – assessed by KPS and/or by ECOG (Table 2) – is the traditional method applied by hematologists to evaluate the disease/treatment impact on the elderly patient's ability to care for themselves and to work.
Correlations between performance and functional scales.
| ECOG | KPS | IADL | ||||
|---|---|---|---|---|---|---|
| Good performance | 0–1 | Normal activity | 80–100% | Able to carry on normal activity and to work | Phone calls?Locomotion?Shopping?Making meals?Housekeeping?Housework?Care with clothes?Taking medicines?Managing money? | Is independence in instrumental activities preserved? |
| ADL | ||||||
|---|---|---|---|---|---|---|
| Poor performance | 2 | In bed<50% of normal daytime | 50–70% | Unable to work; able to live at home and care for most personal needs | Bathing?Dressing?Toilet?Transference?Continence?Feeding? | Is independence in basic activities preserved? |
| 3–5 | In bed>50% of normal daytime | 0–40% | Unable to care for self; requires equivalent of institutional or hospital care | |||
KPS: Karnofsky performance scale; ECOG: Eastern Cooperative Oncology Group scale; IADL: instrumental activities of daily living; ADL: basic activities of daily living; Good performance: KPS ≥80% and ECOG <2; Independence: no dependence in ADL and IADL; Dependence: need help in at least one daily activity.
These instruments are not based on a systematic questionnaire. The scores are obtained based on a general impression of the clinician about the patient's symptoms and the patient's autonomy to care for themself and to work. One disadvantage of this method is the lack of definitions to specifically characterize the score levels of these scales.3
Functional status is the level of autonomy that an individual has in daily activities. The Activity Daily Living Scale (ADL)4 and Instrumental Activity Of Daily Living Scale (IADL)5 are complementary tools widely validated to measure functional status.
ADL was validated by Katz in chronically ill patients and is composed of six questions about specific and universal tasks.4 IADL was delineated by Lawton and is a scale with nine questions with three possible answers: able, able with help and unable. It refers to the autonomy in activities that are more influenced by cultural context (Table 2).
In 1995, Mor et al.6 evaluated the validity of KPS by showing the autonomy in daily living activities for each KPS assessed in 685 patients with advanced cancer on applying the KPS and ADL. They showed that the autonomy of these patients was lower as their KPS score decreased.
KPS, ECOG, ADL and IADL refer to the same construct, i.e., to the same abstract theoretical concept. Different to KPS and ECOG, ADL and IADL employ a sequence of specific questions. The possible answers to each question are graduated in two (able or unable) or in three (able, able with help, and unable) levels. These instruments highlight improvements or impairments in functionality during the follow up of the patient.
As shown in Table 2, the correlation between these scores suggests that patients with poor KPS have lost their autonomy in the IADL5 and are at risk of dependence in basic ADL.4 However, individuals with good KPS probably have preserved autonomy in the ADL dimension but may evolve with some IADL dependence.
Loosing autonomy in ADL and having poor scores in KPS (≤80%) or ECOG (>1) are of prognostic value.3,7
However, despite the prognostic value of performance status, elderly patients with good KPS could be at high risk to succumb during the induction phase of AML treatment for reasons not related to the disease. This event has justified some researchers to applying geriatric approaches in elderly patients with AML. The gold standard method for evaluating older patients is Comprehensive Geriatric Assessment (CGA).
CGA is a multidisciplinary and time-consuming approach that includes functional, cognitive, psychological status, comorbidity, nutritional, polypharmacy and social support assessments. Over the last 20 years, CGA has been applied in the oncogeriatric field and has aggregated important data for the therapeutic management of this group of individuals. It is notable that the ADL and IADL are tools widely used for the functional status assessment included in CGA.8
In 2006, Wedding et al.9 demonstrated the benefit of adding the IADL to the KPS in the functional assessment of elderly patients with AML. Since then, several other researchers have studied the impact of geriatric parameters in the survival and the quality of life of older patients with hematological malignancies.10
Aging is associated with a high incidence of comorbidities that have a significant impact on survival and on complications of treatment.11 Comorbidities are morbid entities that have already been diagnosed at the time of the diagnosis of the index disease, here AML, or that are diagnosed during the patient follow up.
Extermann et al.11 studied the tools used for comorbidity scoring in elderly patients with cancer. They showed that comorbidity scores increase with advancing age and that these scores are correlated with mortality but not associated to functional status.11 In conclusion, comorbidity and functionality are independent variables and should be measured separately in older patients with cancer.
Recently, hematologists developed disease specific instruments that measure the impact of comorbidities on elderly individuals with AML, myelodysplastic syndromes and those submitted to hematopoietic stem cell transplantation. Sorror et al. developed the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI)12 which has already been validated in patients with AML.
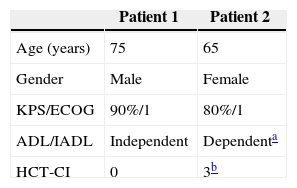
What happened to the patient's assessment with the aggregation of some geriatric scales? Table 3 shows the result of functional and comorbidity assessment of the two reported cases.
Functional assessment and comorbidity scores of clinical challenge patients.
| Patient 1 | Patient 2 | |
|---|---|---|
| Age (years) | 75 | 65 |
| Gender | Male | Female |
| KPS/ECOG | 90%/1 | 80%/1 |
| ADL/IADL | Independent | Dependenta |
| HCT-CI | 0 | 3b |
KPS: Karnofsky performance scale; ECOG: eastern cooperative oncologic group scale; ADL: activities of daily living scale; IADL: instrumental activities of daily living scale; Independent: no dependence in daily activities; HCT-CI: hematopoietic cell transplantation-comorbidity index.
Patient 1 was submitted to the standard treatment with full doses of the AML induction protocol and one consolidation phase. After consolidation, he evolved with sepsis and prolonged neutropenic period. Six months after the diagnosis of AML, he was alive and without evidence of disease.
Patient 2 was submitted to exclusive palliative care, according to her and her family's wishes and considering the impact of her comorbidity score and her dependence according to ADL/IADL. She died of AML four months after diagnosis.
Considering these two patients, both with good KPS, Patient 1 was ten years older than Patient 2. Despite this, he had greater autonomy and a lower comorbidity score that delineated a clinical context more favorable to AML treatment. Moreover, the aggregation of geriatric tools added information about Patient 2 that identified her functional and comorbidity-related risks. These instruments provided specific information for the management of her final phase of life.
In conclusion, ADL and IADL improved the sensitivity of the functional assessment of these elderly patients. They added important information about Patient 2 that changed her performance score from ‘good’ to ‘good but dependent’. Furthermore, the HCT-CI score predicted the impact of comorbidities on her survival. The applications of ADL, IADL and HCT-CI improve the assessment of elderly patients with hematological malignances.
Conflicts of interestThe authors declare no conflicts of interest.