The recent infective outbreak caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), now officially defined as coronavirus disease 2019 (COVID-19), has already affected over 95,000 people from over 85 countries worldwide, causing approximately 3300 deaths.1 The clinical characteristics of this pandemic disease may be complicated by the onset of a severe form of intestinal pneumonia in 10–15% of infected patients, which may then progress toward acute respiratory distress syndrome (ARDS) and eventually in multi-organ failure (MOF) and death.2 Since laboratory hematology is a mainstay for screening, diagnosis, but also for prognostication and therapeutic monitoring of a kaleidoscope of human disorders,3 the aim of this article was to investigate whether or not hemoglobin values may be a predictive factor of worse clinical progression in patients with COVID-19.
We performed an electronic search in Medline, Web of Science and Scopus, using the keywords “laboratory” OR “hemoglobin” AND “coronavirus 2019” OR “2019-nCoV” OR “SARS-CoV-2”, between 2019 and the present time (i.e., March 4, 2020), with no language restriction. The title, abstract and full text of documents identified according to these search criteria were analyzed and those reporting information on the hemoglobin values in COVID-19 patients with or without severe disease (i.e., those needing mechanical ventilation, intensive care unit (ICU) admission or those who died), were meta-analyzed. The reference list of all documents was examined to identify additional eligible studies. The final meta-analysis entailed the estimation of the weighted mean difference (WMD) and 95% confidence interval (95% CI) of hemoglobin values between subjects with or without severe disease. The statistical analysis was performed with the MetaXL software, Version 5.3 (EpiGear International Pty Ltd., Sunrise Beach, Australia). The mean and standard deviation of each study were extrapolated from the data of sample size, median and interquartile range (IQR), as suggested by Hozo et al.4
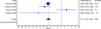
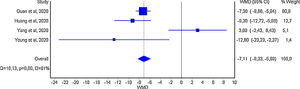
Overall, 80 items were originally detected, according to our search criteria, but 77 of these were excluded because they were review articles (n=6), commentaries or other editorial material (n=1), did not specifically deal with COVID-19 disease (n=62), or did not provide hemoglobin levels in COVID-19 patients, with or without severe disease (n=8). One more study was detected from the reading the reference list of selected articles, so that a final number of four studies were included in our meta-analysis,5–8 totaling 1210 COVID-19 patients (224 with severe disease; 18.5%). The primary endpoint was defined as a composite of admission to the intensive care unit (ICU), need of mechanical ventilation or death in the study by Guan et al.,5 ICU admission in the study by Huang et al.,6 death in the study by Yang et al.7 and the need for mechanical ventilation in the study by Young et al.8 The heterogeneity among the studies was high (i.e., I2, 81%; p<0.001).
The mean hemoglobin difference of the four individual studies reporting continuous values of this parameter is shown in Figure 1. In all except one7 of these four investigations, the hemoglobin value was found to be significantly lower in COVID-19 patients with severe disease than in those with milder forms, yielding a WMD of −7.1g/L; 95% CI, −8.3 to −5.9g/L).
Despite the heterogeneity observed among the available studies, the results of this meta-analysis show that hemoglobin values are essentially reduced in COVID-19 patients with severe disease, compared to those with milder forms, thus confirming previous evidence garnered from patients with other types of pneumonia.9 Some clinical considerations can hence be made. First, initial assessment and longitudinal monitoring of hemoglobin values seems advisable in patients with the SARS-CoV-2 infection, whereby a progressive decrease in the hemoglobin concentration may reflect a worse clinical progression. Subsequently, studies shall be urgently planned to assess whether transfusion support (e.g., with administration of blood or packed red blood cells) may be helpful in this clinical setting to prevent evolution into severe disease and death.
Authorship contributionsGL conceived and designed the study, analyzed the data, performed the statistical analysis and drafted the manuscript; CM interpreted the data and assisted in the writing of the manuscript. All authors critically revised the manuscript and approved the final version.
Conflicts of interestThe authors declare no conflicts of interest.