Primary myelofibrosis is a clonal myeloproliferative neoplasm characterized by atypical myeloid proliferation and significant symptom burden. Activation of the Jak-STAT signaling pathway plays a central role in the pathogenesis of this disease. Approximately 90% of patients have one of three genetic mutations: Jak2V17F, CALR and MPL. The Jak2V617F mutation is the most common mutation and has been found in 60%‒65% of patients. Last year in SOHO 2024 annual meeting we first demonstrated genetic mutations of primary myelofibrosis patients in Azerbaijan. However, in our study only a small number of patients underwent genetic testing. Here we have updated the data of our cohort. The main goal of our study was to know the genetic profile of primary myelofibrosis patients in Azerbaijan.
MethodologyWe retrospectively analyzed 123 patients with primary myelofibrosis who underwent genetic testing. We created 2 groups according to JAK2 levels. Group comparability was assessed by comparing baseline demographics and follow-up time between groups. Normality and heteroscedasticity of continuous data were assessed using the Shapiro-Wilk and Levene tests, respectively. Continuous outcomes were compared using unpaired Student t-test, Welch t-test or Mann-Whitney U test, depending on the data distribution. Discrete outcomes were compared using Chi-Squared or Fisher's exact test, respectively. The alpha risk was set at 5% and two-tailed tests were used.
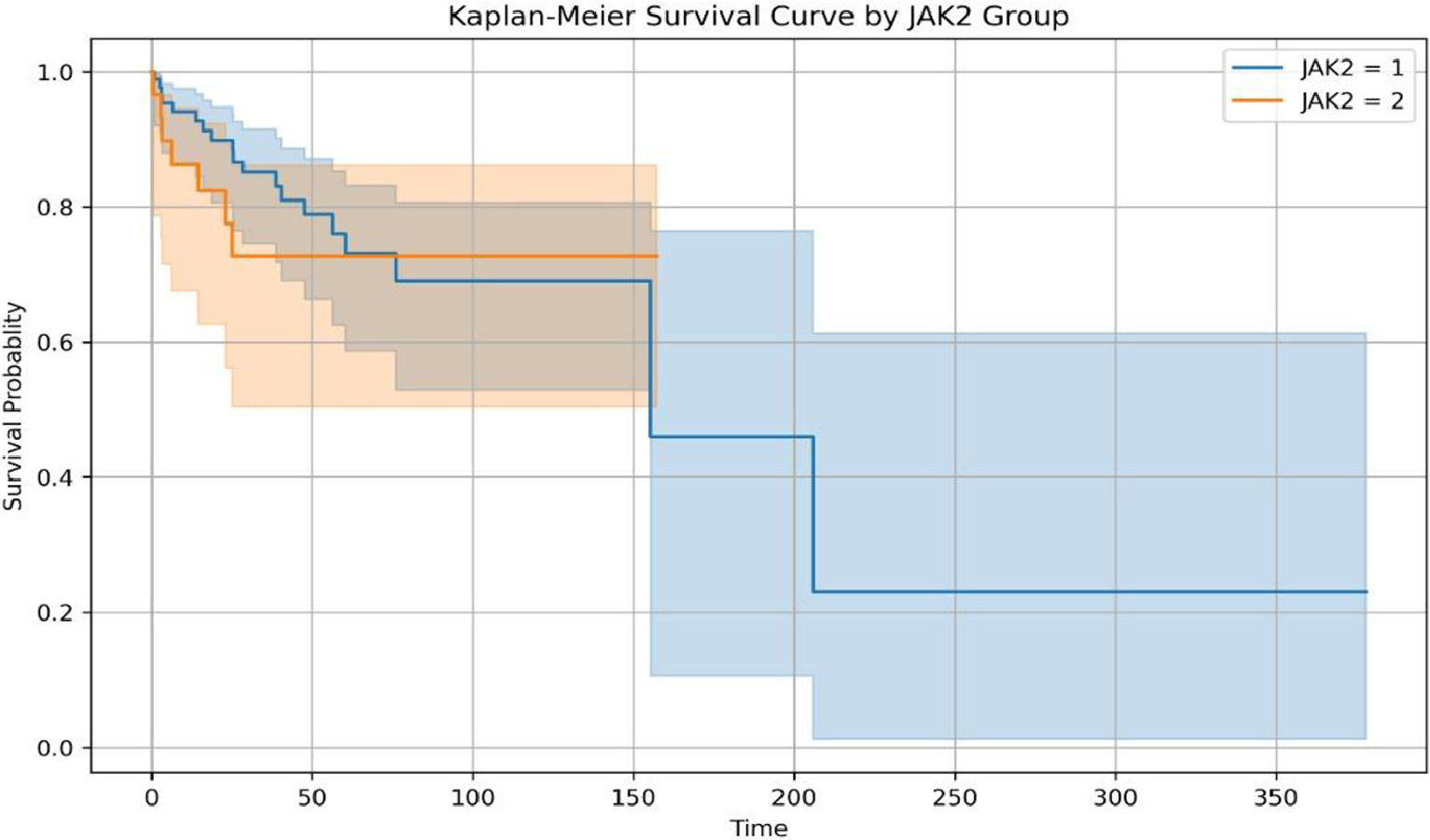
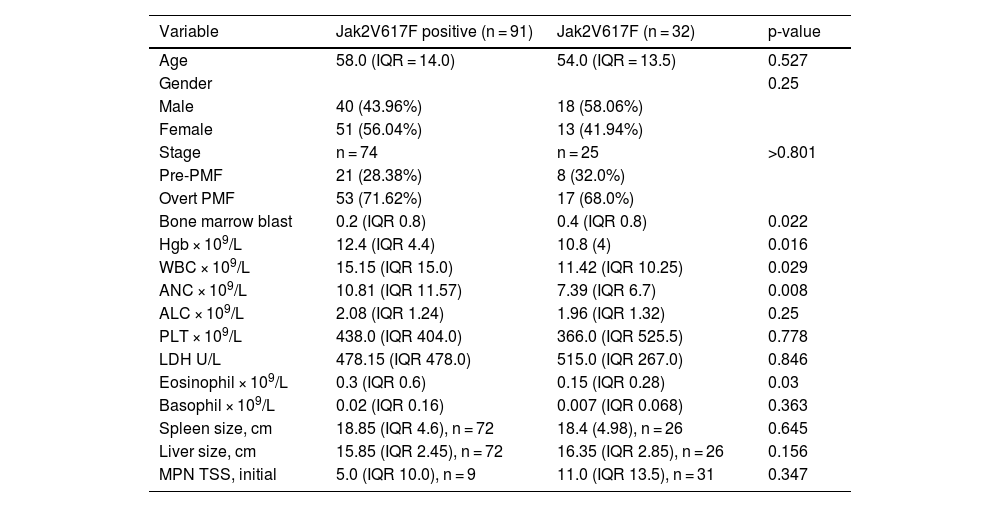
ResultsA total of 123 patients underwent genetic testing. Jak2V617F was positive in 91 (74%), CALR was positive in 3 (2.4%), MPL was positive in 1 (0.8%) patient. 32 (26%) patients were Jak2 negative. The median allele burden was 68.21% (IQR = 46.16). Median age was 58.5-years, 58 (47.2%) patients were male. We separated patients to groups according to Jak2 mutations and compared their clinical laboratory characteristics (Table 1). There was no difference between two groups according to IPSS: Low – 27 (31.03%), INT1 – 42 (48.28%), INT2 – 17 (19.54%), High ‒ 1 (1.15%) in Jak2 positive (n = 87) vs. Negative (n = 31) Low ‒ 11 (35.48%), INT1 ‒ 12 (38.71%), INT2 ‒ 7 (22.58%), High – 1 (3.23%). Jak2V617F positivity was significantly associated with higher Hgb (p = -0.022), WBC (0.029), higher ANC (p = -0.008), higher eosinophil count (p = -0.03) and lower bone marrow blast count (p = -0.022). Jak2V617F positivity was also associated with lower LDH, lower TSS and higher PLT count, but this was not statistically significant. The splenomegaly rate didn't differ between groups (Jak2 positive ‒ 94.44% and Jak2 negative ‒ 84.62%; p = 0.203). Median follow-up was 34.61-months. Although statistically insignificant, Jak2V617F negative patients seems to have better OS than Jak2V617F positive patients (p = -0.644). Median OS didn't reach in Jak2 negative group vs. 155-months in Jak2 group (Fig. 1).
ConclusionComparison of clinical and laboratory data between Jak2 positive and negative groups in patients with primary myelofibrosis in Azerbaijan has been performed. In our cohort, Jak2V617F positive have significantly higher Hgb, Wbc, ANC, bone marrow blast and eosinophil counts, also higher PLT, lower LDH and Total Symptom burden (TSS), but it's not statistically significant. Similar to our study, article by Vannucchi A.M and colleagues published in the journal Leukemia in 2008, the authors showed that JAK2 V617F mutations in PMF are associated with older age, higher HB level, leukocytosis, and lower platelet count.[1] How Jak2V617F mutation affects the OS in PMF remains controversial. Although it's not statistically significant, we found that Jak2V617F negative patients have a better median OS than positive patients in our cohort. Unlike this, in a multicenter study of 152 patients, Campbell PJ et. al. showed that in PMF, the presence of JAK2V617F was associated with inferior survival despite the fact that mutated patients were less likely to require red blood cell transfusions during follow-up.[2] On the contrary, in a series of 117 PMF patients from a single center, Tefferi et al. reported no significant impact of V617F presence on either survival or leukemic transformation.[3] But we didn't have the exact rate of the CALR and the MPL mutation rate in the Jak2-negative group in our cohort, so we didn't know how this mutation was affecting our study results. So the small number of patients in the comparison groups and the lack of testing for ASXL1, lower number of CALR, MPL mutation is a limitation of our study. There is a need for prospective, large studies with comprehensive genetic testing to learn exactly how genetic mutations affect survival in our PMF patients.
References:
- 1.
Vannucchi AM, Antonioli E, Guglielmelli P, Pardanani A, Tefferi A. Clinical correlates of JAK2V617F presence or allele burden in myeloproliferative neoplasms: A critical reappraisal. Leukemia. 2008;22:1299-307.
- 2.
Campbell PJ, Griesshammer M, Döhner K, Döhner H, Kusec R, Hasselbalch HC, et al. V617F mutation in JAK2 is associated with poorer survival in idiopathic myelofibrosis. Blood. 2006;107:2098-100.
- 3.
Tefferi A, Lasho TL, Schwager SM, Steensma DP, Mesa RA, Li C-Y, et al. The JAK2(V617F) tyrosine kinase mutation in myelofibrosis with myeloid metaplasia: lineage specificity and clinical corre-lates. Br J Haematol. 2005;131:320-8.
Table 1 Patient characteristics.