Different factors affect the quality and viability of cord blood stem cells, and therefore the efficacy of umbilical cord stem cell transplantation. Fetal distress is one factor affecting the quantity of CD34+ cells in cord blood. This study was designed to compare the viability and yield of the umbilical cord blood stem cells of women who have undergone emergency lower segment caesarean section for fetal distress or for other causes.
Materials and methodsThis cross-sectional analytical study was performed at a tertiary care hospital facility with a total sample size of 68: 34 participants had undergone emergency C-section for fetal distress, and 34 had undergone emergency C-section for other causes. Umbilical cord blood was collected ex-utero in a 350 mL bag with citrate-phosphate-dextrose solution with adenine. Three milliliter of blood were transferred to an ethylenediaminetetraacetic acid (EDTA) tube for cell counts and flow cytometry testing for CD34+. The chi-square test was used to compare the total mononuclear cell, CD34+, and viability between the groups.
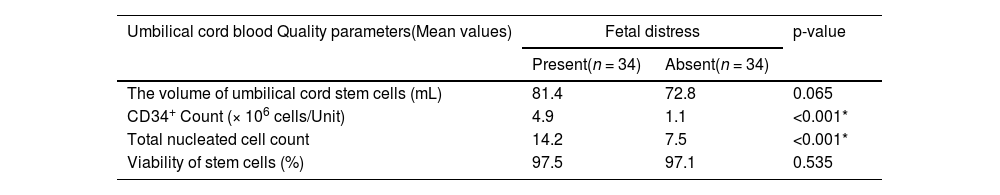
ResultsThe CD34+ count [mean 4.9 versus 1.1 (× 106 cells/unit)] and total nucleated cell count [mean 14.2 versus 7.5 (× 108/unit)] were significantly higher in cord blood units collected from women who delivered by C-section for fetal distress (p-value <0.05). However, the volume of umbilical cord stem cells and viability of stem cells did not vary significantly based on the presence or absence of fetal distress (p-value >0.05).
ConclusionThe current study shows that umbilical cord blood collected during fetal distress has a significantly higher content of stem cells and total nucleated cells than the non-fetal distress group
After childbirth, the placenta and associated umbilical cord contain blood, known as umbilical cord blood (UCB) or cord blood. Cord blood, which contains stem cells, can treat cancer and other genetic and haematological illnesses.1 Since the first UCB transplant in 1988, the use of UCB was established as an alternative source of hematopoietic stem cells (HSC) for bone marrow reconstitution.2 Compared to bone marrow and mobilized peripheral blood HSC for transplantation, cord blood provides several benefits, including easy availability, less danger to the donor, reduced human leukocyte antigen (HLA) matching standards, and a lower risk of graft-versus-host disease.3 However, the inadequate number and quality of a single cord blood unit lead to delayed engraftment rates. Different factors affect the quality and viability of cord blood stem cells, influencing the efficacy of UCB stem cell transplantation.4 Fetal distress is one factor that impacts the quantity of CD34+ cells in cord blood. There are very limited studies on this matter. This research will enable us to determine whether fetal distress might affect the viability and number of umbilical cord stem cells and contribute to our understanding of maternal and fetal factors that influence the quantity and survivability of umbilical cord stem cells. It can also help us to improve our knowledge that might be applied to increase the effectiveness of UCB stem cell transplantation in children and adults.
UCB stem cells are a rich source of hematopoietic stem cells for transplantation in hematologic malignancy and blood diseases.5 However, a major drawback is the small number of cells, low CD34+ cell count, and low total nucleated cells. According to research, proinflammatory cytokines, such as interleukin-1 beta, interleukin-6, interleukin-8, stress hormones (cortisol and epinephrine) and ischemia, which cause the rapid mobilization of stem cells into the blood, are released during emergency caesarean sections performed because of fetal distress and result in a higher count of CD34+ cells.6 Studies have examined whether the number of stem cells in UCB increases or decreases following vaginal and caesarean deliveries during fetal distress. So far, not many studies have been performed to evaluate the outcome of emergency lower segment caesarean section (LSCS) regarding the yield and viability of UCB stem cells.4
This study was designed to compare the viability and yield of UCB stem cells of women who underwent emergency LSCS for fetal distress or for other causes.
Material and methodsStudy settingThis was a cross-sectional analytical study conducted at a single centre which is a tertiary care-level facility. During the study period from April 2021 to December 2022, a total of 68 participants, 34 women who underwent LSCS due to fetal distress and 34 women who underwent LSCS due to causes other than fetal distress, were included.
Sample size calculationThe study was planned as one of the continuous response variables from independent controls and experimental subjects, with one control per experimental subject. The sample size was calculated based on the expected difference between Experimental and Control Groups of 0.08. Hence, it was necessary to study 34 subjects in each group in order to reject the null hypothesis that the population mean of the groups would be equal with a probability of 0.9. The type 1 error of probability associated with the test of this null hypothesis is 0.05.
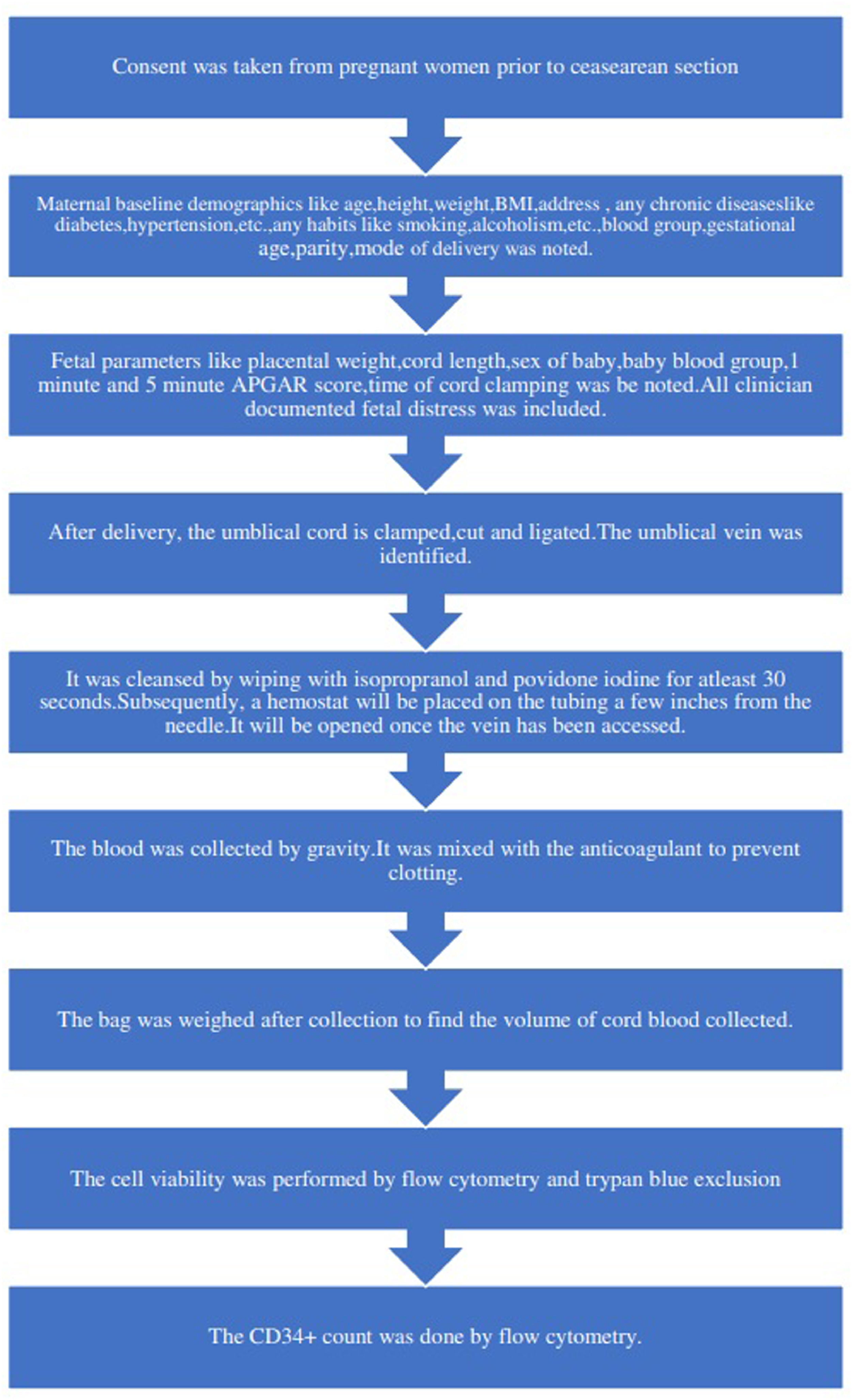
Inclusion and exclusion criteriaWomen delivered by emergency LSCS during the study period who consented to be a part of the study were included. Pathological or suspicious cardiotocography (CTG) was considered as per the 2015 International Federation of Gynecology and Obstetrics (FIGO) intrapartum CTG criteria.7 Mothers who underwent antenatal interventions like intrauterine transfusions or were known to have a fetus affected by a haemolytic disease, all deliveries with structural placental abnormalities, cord abnormalities, congenital anomalies of the fetus, and peripartum complications like severe post-partum haemorrhage were excluded. The study methodology is summarized in Figure 1.
Collection and processing of umbilical cord bloodThe labour room was requested to inform the investigator prior to all emergency LSCS. After explaining the procedure, consent was taken from the mother or relatives, and data was collected as per standard structured proforma. After the delivery of the baby, the umbilical cord was double-clamped and cut. The first clamp was applied near the placental side, the second clamp was near the baby side. After the removal of the placenta from the uterus, it was weighed and transferred to a kidney tray to check for any tears and intactness of the segments. The umbilical cord was cleaned using a betadine solution to remove maternal blood and contaminants. The umbilical vein was identified and pricked with a 16-gauge blood bag needle under aseptic conditions, and cord blood was collected in a 350 mL bag with citrate-phosphate-dextrose solution with adenine (CPDA). Milking of the cord was performed. The UCB was gently and periodically mixed with the anticoagulant to prevent clotting. The collection was continued till the umbilical cord appeared to collapse. The blood bag was weighed to find the volume of cord blood collected. Three milliliter of blood was transferred to an ethylenediaminetetraacetic acid (EDTA) tube for flow cytometry (FCM).
The white blood cell count of the UCB sample was first checked and diluted with phosphate-buffered saline to bring the count to <50,000 cells/mm3.
Flow cytometry for cell enumerationThe standard operating procedure adopted in our laboratory for single platform (SP) FCM enumeration of CD34+ hematopoietic stem cells is based on the International Society for Hematotherapy and Graft Engineering (ISHAGE) protocol.8 FCM enumeration of CD34+ cells was based on four parameters: a. CD34 positivity b. Dim CD45 expression (lymphocytes and monocytes), like characteristics of blasts c. Low side scatter d. Low to intermediate forward scatter; 7-Aminoactinomycin D was used to check viability. The test was run in duplicate, and the average of the values was taken as the final report. The equipment used was Beckman Coulter Navios, and the analysis software used was Kaluza version 2.1.
Statistical analysisThe data on nominal and ordinal variables such as sex of the baby, blood group, mode of delivery, personal history, diseases, etc., are expressed as frequencies and percentages. The continuous data such as age, cord length, placental weight, total mononuclear cell count, CD34+ count, and viability are expressed as means ± standard deviation (SD) or median with range. The chi-square test was used to compare total mononuclear cell count, CD34+, and viability between the groups. The agreement in the chi-square test or Fisher's exact test between the groups was explored using Kappa statistics. All statistical analyses were carried out at a 5 % significance level and a p-value less than 0.05 was considered significant. All the statistical analyses used the Statistical Package for Social Sciences (SPSS) software version 19.0 (IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp).
Ethics and informed consentEthics approval was obtained from our hospital's Institute Ethics Committee (IEC - letter number JIP/IEC/2021/023 dated 07.04.2021). Furthermore, a written informed consent form approved by the IEC was used to obtain consent from the participants after educating them about the intervention and what was expected from them. In addition, a patient information sheet in English and the local language was given to them.
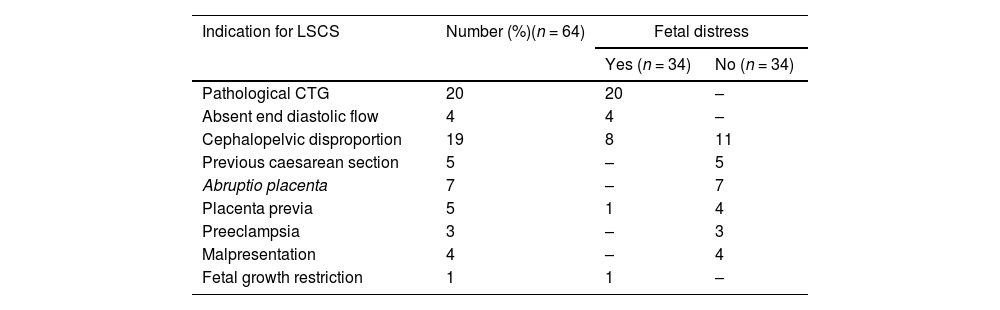
ResultsSixty-eight participants were included in the study,: 34 women who underwent LSCS due to fetal distress and 34 who underwent LSCS due to causes other than fetal distress. The mean age of the study participants was 26.2 years (± 3.9 years), and the mean weight and height of the women who underwent emergency LSCS were 69.2 kg (± 9.2 kg) and 159.5 cm (± 4.7 cm), respectively. The mean body mass index of the women was 27.2, with a standard deviation of 3.3. The mean gestational age of the study participants was 269.1 days (± 9.4 days). In the present study, 89.7 % of women had term delivery, and 10.3 % had preterm delivery. The mean birth weight of the babies was 3.3 kg (± 0.5 kg). Most (97.1 %) of the babies had normal birth weight, with only 2.9 % being born with birth weight less than 2500 g. More than half the women in the present study were not primigravida (52.9 %). In the present study, five women (7.3 %) had comorbidities. The illnesses included hypothyroidism and diabetes mellitus. Only one woman who underwent LSCS in the present study reported habits (Betel chewing - 1.5 %). The various indications for LSCS in both groups are compared in Tables 1 and 3.
Indications for lower segment caesarean section in the participants and comparison between groups.
LSCS: lower segment caesarean section; CTG: cardiotocography.
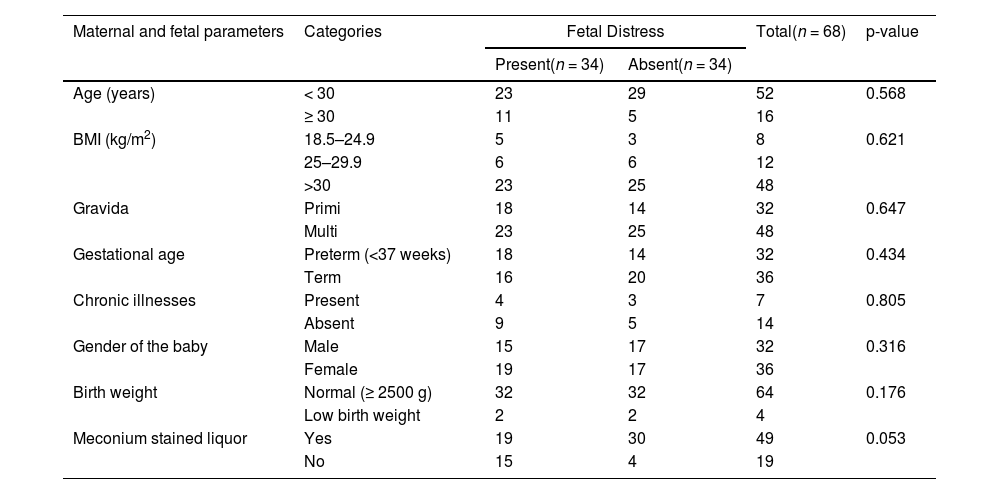
The mean duration of the first stage, second stage and overall duration of labour were 337.8 min, 5.3 min and 5.8 h, respectively. Meconium-stained liquor was found in 19 (27.9 %) pregnancies. With regard to gender, the number of fetuses was almost equal with 32 males and 36 females. The various other fetal parameters of the participants that could affect the outcomes are compared in Table 2 and were shown not to be significantly different between the groups.
Comparison of fetal and maternal parameters between the groups.
The CD34+ counts [mean 4.9 versus 1.1 (× 106 cells/unit)] and total nucleated cell (TNC) counts [mean 14.2 versus 7.5 (× 108 cells/unit)] were significantly higher in cord blood collected from women who delivered through LSCS due to fetal distress (p-value <0.05). However, the volume of umbilical cord stem cells and viability of stem cells did not vary significantly based on the presence or absence of fetal distress (p-value >0.05).
DiscussionThis study was conducted among women who underwent emergency LSCS due to fetal distress and other causes to evaluate the cord blood quality parameters such as TNC, CD34+ count, the volume of UCB, and viability of cells. These parameters were compared between women who underwent emergency LSCS due to fetal distress and those without fetal distress. Studies have found that fetal distress can affect the aforementioned parameters. When a fetus is in acute or intrapartum distress due to a lack of oxygen, anaerobic glycolysis occurs, accumulating lactic acid and pyruvic acid (metabolic acidosis). H+ ions are activated as a result, which depresses the fetal cardiac node and causes erratic FHS. Chronic fetal distress occurs when there is a long-term decrease in uterine blood flow to the placenta, which causes inadequate blood supply to the fetal pulmonary and renal system organs, leading to fetal hypoxia and acidosis.9 Ischemia and interleukin-8 cause stem cells to mobilize quickly into the bloodstream. Although the causes of the mobilization of stem cells into the UCB are not fully understood, compared to vaginal deliveries, primary elective caesarean sections have lower levels of proinflammatory cytokines (interleukin-1b, interleukin-6) and stress hormones (epinephrine, cortisol).10 There are limited studies on the effect of emergency LSCS due to fetal distress on cord blood parameters. In adults, extensive exercise and ischemia have been shown to mobilize stem cells into circulation rapidly.11,12
This study found that CD34+ counts (mean: 4.9) and total nucleated cell counts (mean: 14.2) were higher among women who underwent emergency LSCS due to fetal distress compared to emergency LSCS due to other causes (p-value <0.05). These results are similar to other studies.13,14 However, the volume of UCB stem cells and viability of stem cells did not vary significantly based on the presence or absence of fetal distress (p-value >0.05). This finding is similar to a study by Nunes et al.15 Multiple studies have evaluated various maternal and fetal factors influencing TNC, CD34+ count, and volume of UCB. The present study is the first to evaluate the effect of fetal distress on the yield and viability of UCB stem cells, comparing emergency LSCS with fetal distress and emergency LSCS due to other causes. A study by Manegold showed that white blood cell counts, nucleated red blood cells, and colony-forming units were all higher in units from secondary caesarean sections due to fetal distress compared to those collected following primary caesarean sections. The decision to perform a secondary caesarean section is usually based on unforeseeable obstetric factors. Therefore, discussion with the expectant woman regarding UCB donation and standardized preparation for the donations should be undertaken before the onset of labour to ensure the collection of these valuable UCB units after the safe delivery of the newborn.
Distressed fetus pregnancy is often considered a contraindication for UCB collection. Perhaps this recommendation is not warranted. It may not be feasible to recruit preferentially distressed-fetus pregnancy; however, they need not be an exclusion criterion for UCB for transplantation, as cord blood units are not very rich in CD34+ cells. Whether this information can be utilized in the future for a good collection of stem cells by recruiting fetal distress groups as the source of stem cell collection is something that needs to be thought of due to the logistics involved.
ConclusionThe present study shows that UCB collected during fetal distress have a significantly higher content of stem cells and TNC than from the non-fetal distress group. The other quality parameters, like volume of UCB and viability in the fetal distress group, were comparable to the non-fetal distress group.
Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry