Sickle cell disease (SCD) is a group of genetic conditions related to the presence of a sickle hemoglobin (Hb S) mutation (HBB:c.20A>T). People with SCD can be homozygous for Hb S or can have compound heterozygosity for Hb S with other gene mutations.1,2 Some hematologic features of SCD are listed in Table 1, but rare genotypes can also be found. Since the concentration of Hb S is a pathophysiological factor of disease severity, the presence of lower concentrations of Hb S due to double heterozygosity can determine phenotypic heterogeneity.1,3 However, other genetic and environmental factors can also have an effect on the disease phenotype.4
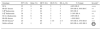
Hematological features of some sickle hemoglobinopathies.
| Genotype | PCV (%) | Retic (%) | MCV (fL) | Hb F (%) | Hb A2 (%) | % Variant | Severitya |
|---|---|---|---|---|---|---|---|
| SCA | 25 | 8 | 90 | 5 | 3 | >90% Hb S | ++++ |
| Hb SC disease | 35 | 3 | 80 | 2 | 3 | 50% Hb S, 50% Hb C | ++ |
| S-β0 thalassemia | 27 | 7 | 82 | 7 | 5 | 90% Hb S | ++++ |
| S-β+ thalassemia | 38 | 2 | 70 | 2 | 6 | 5–30% Hb A | ++ |
| SCA-α thalassemia | 30 | 6 | 78 | 5 | 5 | >90% Hb S | +++ |
| Hb SE disease | 35 | 3 | 75 | 2 | 3 | ∼30% Hb E | ++ |
| Hb SD disease* | 20 | 86 | 1–10 | 2–4 | 45% Hb S, 45% Hb D | +++ | |
| Sickle cell trait | 45 | 1 | 85 | 1 | 2 | 60% Hb A, 40% Hb S |
SCA: sickle cell anemia; PCV: packed cell volume; Retic: reticulocyte count; MCV: mean cell volume; Hb: Hemoglobin.
Studies looking for abnormal hemoglobins (Hbs) in the Brazilian population have been performed since the 1950s.5–8 However, the Brazilian Government Directive MS # 822/01 that regulates newborn screening for hemoglobinopathies, has promoted an increase of data about hemoglobinopathies in different Brazilian regions.9–11 This associated with the use of isoelectric focusing electrophoresis (IEF) and high-pressure liquid chromatography (HPLC) as diagnostic methods, has enabled the identification of an increasing number of abnormal Hbs as well as compound heterozygous states of Hb S.12–14 An example is a paper published in this issue of the Revista Brasileira de Hematologia e Hemoterapia that shows data on a cohort of children with hemoglobin SD pattern.15
Hb D is an abnormal Hb, which migrates to the same position as Hb S in electrophoresis at alkaline pH, and can be separated from Hb S in acid pH.16–18 Several Hb D have been described in different racial groups, but the majority presented a point mutation in codon 121 of the β-globin gene, which results in the substitution of glutamic acid for glutamine (HBB:c.364G>C). This abnormal Hb is usually called Hb D-Punjab or Hb D-Los Angeles, however it can also be named Hb D-North Carolina, Hb D-Chicago, Hb D-Portugal, Hb D-Cyprus, and Hb D-Oak Ridge.19–21 The estimated prevalence of Hb D-Punjab is 0.1 to 0.4% in African-Americans.22 In Brazil, a study of African descendants showed a similar prevalence.5
Sometime after the discovery of Hb D-Punjab, the coinheritance of Hb D-Punjab and Hb S was identified in Caucasian patients with clinical and hematological manifestations similar to those of sickle cell anemia (SCA), because this mutation facilitates Hb S polymerization.23–25 Further clinical studies confirmed the severity of the manifestations of this association and the need to treat these individuals as SCA patients by prescribing hydroxyurea when indicated.21,26–29
There are other types of Hb D due to different point mutations in the β-globin gene, such as Hb D-Iran (HBB:c.67G>C) and Hb D-Ibadan (HBB:c.263C>A). However, individuals with these mutations have normal hematologic values and do not suffer from vaso-occlusive complications, since their red cells do not sickle under physiologic conditions.18,30,31
Hb Korle-Bu (Hb KB) or Hb G-Accra (HBB:c.220G>A) is a frequent mutation in Sub-Saharan Africa.32,33 This Hb has the same IEF mobility as Hb D-Punjab but can be differentiated by HPLC. Heterozygotes for Hb KB have no hematologic alterations, and individuals with double heterozygosis Hb S-Hb KB have normal red cells on blood smear and a benign clinical course, similar to sickle cell trait as Hb KB does not participate in the gelation of Hb S.33,34
Interestingly, the Hb KB mutation [beta73(E17)Asp→Asn] can occur in addition to the Hb S mutation [beta6(A3)Glu6Val] in the same beta globin chain. In this case, this Hb with a double mutation is termed Hb C-Harlem (or Hb C-Georgetown) (HBB:c.20A>T, HBB:c.220G>A), because it migrates to the position of Hb C in cellulose acetate electrophoresis at alkaline pH. Individuals heterozygous for Hb C-Harlem are asymptomatic, but the coinheritance of Hb S and Hb C-Harlem has clinical manifestations similar to SCA.20,32,35
Researchers from India and the Middle East are the main authors of the few papers about Hb SD-Punjab; there are less data published about the association Hb S-Hb KB.21,27–29,34,36–41 By studying two different groups of patients with Hb SD patterns, specifically Hb SD-Punjab and Hb S-Hb KB, Rezende et al. not only published important clinical data about the coinheritance of two rare Hb but also pointed out the importance of this differential diagnosis.15
Conflicts of interestThe author declares no conflicts of interest.
See paper by Rezende et al. on pages 240–6.