Lymphomas with primary manifestation in the female genital tract are unusual. Those that meet criteria for primary extranodal lymphomas are even rarer.1 In 1997, the U.S. National Cancer database included more than 90,000 Non-Hodgkin Lymphoma (NHL) patients and found that 28% of them presented a primary extranodal lymphoma, with only 1.5% originating in the female genital tract.2 In those cases, the majority involved the ovaries or the uterus while primary lymphomas of the vagina were uncommon, with just few cases reported in the literature.2 Most of the previously published cases were B-cell non-Hodgkin lymphomas. The most common histological subtype of gynecological lymphomas, primary or secondary, was Diffuse Large B-cell lymphoma1,3 Vaginal T-cell lymphomas are extremely rare and there were only four cases reported since 2000.3-6
Herein we report a rare case of an ALK-positive Anaplastic large cell lymphoma of the vagina successfully treated with chemotherapy and brentuximab vedotin. This is just the second report of this lymphoma subtype in this clinical setting in the literature.
Case reportWe report a case of a previously healthy 35-year-old patient who was referred to our service due to a vaginal lesion with associated fever for 1 month. She did not have weight loss or night sweats during this period. There was no lymphadenopathy or visceromegaly on clinical examination. At admission exams, she had a complete blood count with hemoglobin 12.9g/dL leukocytes 3680/mm3 neutrophils 59% lymphocytes 31% platelets 279.000/mm3 DHL 190 UI/L without renal or hepatic dysfunction.
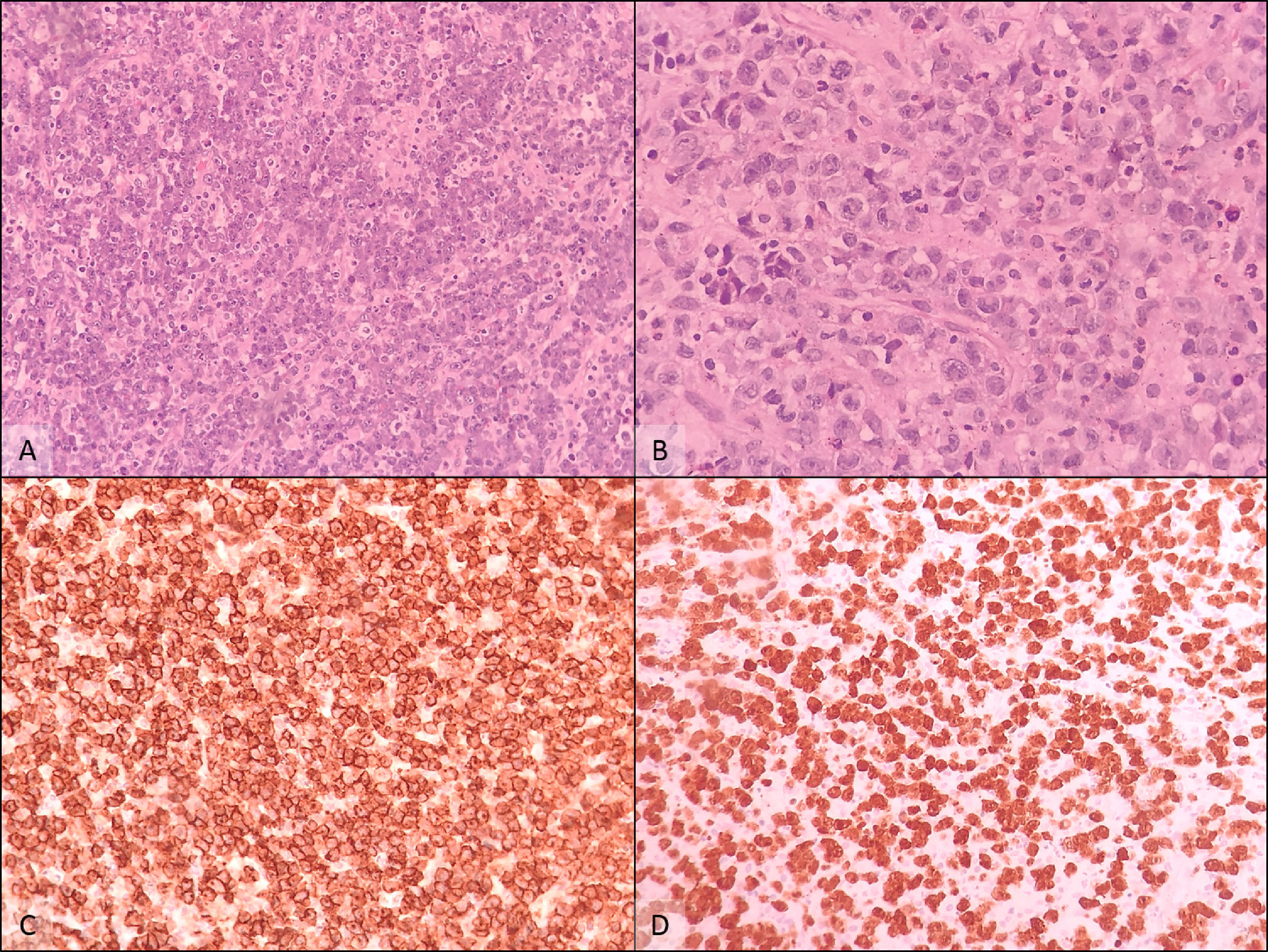
The patient underwent a surgical procedure to remove the lesion. The histopathological evaluation showed diffuse sheets of large lymphoid cells, some of them with eccentric, horseshoe-shaped nuclei, often with an eosinophilic region near the nucleus (hallmark cells). Immunohistochemically, the neoplastic cells were positive for CD4, MUM-1 and CD43, with strong and diffuse positivity for CD30 and ALK-1, with the latter displaying cytoplasmic, nuclear and nucleolar staining (Figure 1). This staining pattern is highly suggestive of the presence of the t(2;5)(p23.2-23.1;q35.1) translocation, which fuses the ALK gene on chromosome 2 and the NPM1 gene on chromosome 5. The proliferative index, measured by Ki-67, was 95%. These findings were consistent with the diagnosis of ALK-positive Anaplastic large cell lymphoma.
Histopathological findings. (A) Section of the vaginal lesion showed diffuse sheets of large lymphoid cells (Hematoxylin & eosin, × 200x). (B) At higher power, some cells with kidney-shaped eccentric nuclei (hallmark cells) could be seen (Hematoxylin & eosin, × 400). (C) There was expression of CD4 and MUM-1 (not shown), together with strong and diffuse membranous expression of CD30 (CD30 antibody, × 200), (D) as well as ALK-1 cytoplasmic, nuclear and nucleolar staining, suggestive of the t(2;5) translocation, involving ALK and NPM1 genes (ALK-1 antibody, × 200).
Magnetic resonance imaging of the pelvis had been performed before the excision and did not identify any lesion. The PET-CT at diagnosis showed no abnormal cellular metabolism and did not suggest the presence of neoplastic activity at all. A bone marrow biopsy was performed and showed no neoplastic infiltration.
According to the Modified Ann Arbor classification, the disease corresponds to a stage IEB.
At that moment, as we had no adequate image exam to evaluate the eventual residual lesion (since the MRI performed before the surgery was negative), it was decided to prescribe four cycles of brentuximab. As in our country it is not possible to prescribe this monoclonal antibody alone in first line treatment, she underwent four cycles of chemotherapy with brentuximab vedotin, cyclophosphamide, doxorubicin, and prednisone (BV-CHP).
The radiological follow-up with tomography and magnetic resonance after the treatment showed no new lesions. As the PET-CT showed no nodal or extranodal metabolic activity before the beginning of the treatment, we didn't perform a new one, especially due to its cost and eventual inability to detect vaginal residual lesions. She underwent clinical follow-up, with good status and resolution of the lesion. She had a complete response to treatment until a year follow-up with gynecological physical examination and laboratory evaluation.
DiscussionWe performed a literature review in an academic medical setting and searched for cases of T-cell vaginal lymphomas reported between 2000 and 2021. Data on T-cell vaginal lymphomas, such as patients' age, presentation at diagnosis, pathophysiology, stage (Modified Ann Arbor classification), treatment, and outcome, were extracted. We used MeSH (Medical Subject Headings) terms for “vaginal” AND “T-cell lymphoma”. After that we selected case reports matching the following criteria: (1) no concomitant involvement of the cervix and/or genital tract other than the vagina; (2) cases written in English (or abstracts in English) (Table 1).
Patients with vaginal T-cell lymphoma from 2000 to 2021.
CR complete response; NKCE - Enteropathy-like Indolent NK-Cell Proliferation; PTCL-NOS Peripheral T-Cell Lymphoma, not Otherwise Specified; RT radiotherapy; THP-COP pirarubicin, cyclophosphamide, vincristine, and prednisone.
We revised 22 cases of vaginal lymphoma reported in the period of 2000 and 2021.We reviewed only four cases of T-cells lymphoma that matched criteria, one of them specified as T-cell extranodal lymphoma, the other as Peripheral T-Cell Lymphoma, not Otherwise Specified (PTCL-NOS), the third one as Enteropathy-like Indolent NK-Cell Proliferation and the last one as ALK-positive Anaplastic large cell lymphoma. The mean age at presentation was 54 years old. The most common clinical presentation was vaginal mass (50%), vaginal bleeding (25%), routine exams (25%). Most of them were localized diseases without B symptoms or nodal commitment (66,6%), and half of them also had bulky presentations at diagnosis.
There was only one report of a vaginal ALK-positive Anaplastic large cell lymphoma. This 52 year-old patient had chronic renal failure and had received hemodialysis for 10 years. The vaginal mass was discovered during an operation for anal hemorrhoids. She rapidly developed sepsis and multiorgan failure and died within 2 weeks, before treatment could be initiated.7
To the best of our knowledge, this is the first vaginal ALK-positive Anaplastic large cell lymphoma treated with a brentuximab vedotin-CHP regimen reported in the literature.
As lymphomas affecting the female genital tract are uncommon, these tumors may be underdiagnosed, both because they are unexpected in these sites and because they may be misdiagnosed as either inflammatory lesions or other types of malignant tumor. Another important issue is the discussion about the treatment and prognosis of this neoplasia. Although it is known that localized ALK-positive Anaplastic large cell lymphoma is a disease with good prognosis and that should be treated mostly with localized strategies, in this case, we had some concerns about a eventually residual mass (not reached by the imaging exams, and especially due to PET-CT inability to detect vaginal residual lesions) and the impossibility to proceed radiotherapy. Considering the advancement of new therapeutic possibilities for T-cell lymphoma, we believe this report can help further chemotherapy regimen decisions.