Lymphoma is a malignant disease of the lymphatic system where there is an uncontrolled proliferation of lymphocytes or their precursors. Lymphomas presented in different degrees of severity are divided into two major groups: Hodgkin's lymphoma (LH) and non-Hodgkin's lymphoma (NHL).1 NHL presents a variety of histological manifestations that makes it difficult to classify and causes controversy among pathologists. One of the forms of NHL is follicular, in which there is a regular nodular pattern that affects the lymph node or the extranodal area.2
Follicular lymphoma (FL) is responsible for 22% of all new cases of NHL, being the second most common subtype its cell originates from the germinal center (centrocytes and centroblasts), and genetic form consists of t(14; 18) translocation which gives rise to the BCL2-IGH redesign, which is characteristic of this disease and is present in 85% of cases. FL usually has a nodular (follicular) pattern, sometimes with focal diffuse areas, and has variable numbers of small, cleaved cells and centroblasts.3
FL has a prediction for the 7th decade and a slight predominance in females, with a heterogeneous presentation, and can be considered and treated as an indolent disease or an aggressive lymphoma according to histological subtype. Risk factors include a family history of NHL (odds ratio, OR ∼ 2), diagnosis of Sjögren's syndrome (OR ∼ 30), and certain polymorphisms in the 6p21.32 region, which encodes the human leukocyte antigen (HLA).4 The risk of developing histological transformation from indolent disease to aggressive disease can occur at approximately 3% per year for patients.5
The main factors associated with NHL are primary or acquired immunodeficiency, autoimmune diseases, and hereditary factors. The treatment of lymphomas in the head and neck region is complex, should not be based on pathology information alone but rather be made in multidisciplinary conferences, and based on the stratification of the RISK FLIPI (Follicular Lymphoma International Prognostic Index), and may include clinical follow-up, chemotherapy-associated or not with radiotherapy until hematopoietic stem cell transplantation.6,7
The purpose of the present case report is to present a case of high-grade transformation after FL diagnosis identified in the oral biopsy.
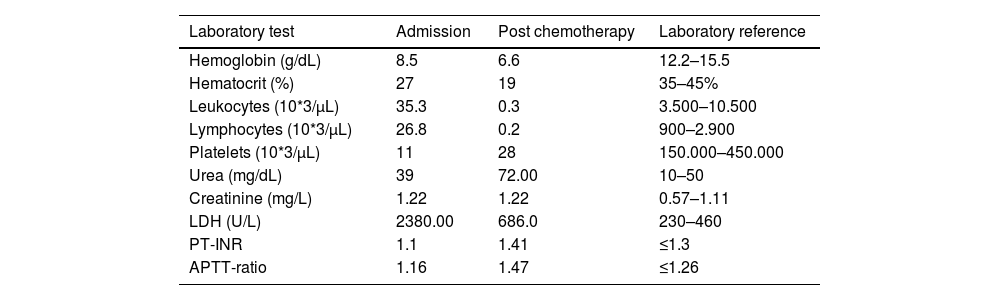
Case reportA 57-year-old female patient complained of abdominal discomfort and weight loss associated with night sweats for last two months. On physical examination, she presented decreased pulmonary auscultation in association with cervical and axillary adenomegaly. Complementary tests were performed: chest X-ray that demonstrated pleural effusion, immunophenotyping of peripheral blood lymphocytes, and cervical lymph node biopsy. Initially, she had a level of lactate dehydrogenase, LDH, in 808.0 U/L, and the blood count showed anemia, lymphocytosis, and thrombocytopenia (Table 1).
Laboratory evolution.
LDH: lactate dehydrogenase; APTT: activated partial thromboplastin time; PT: prothrombin time; INR: international normalized ratio.
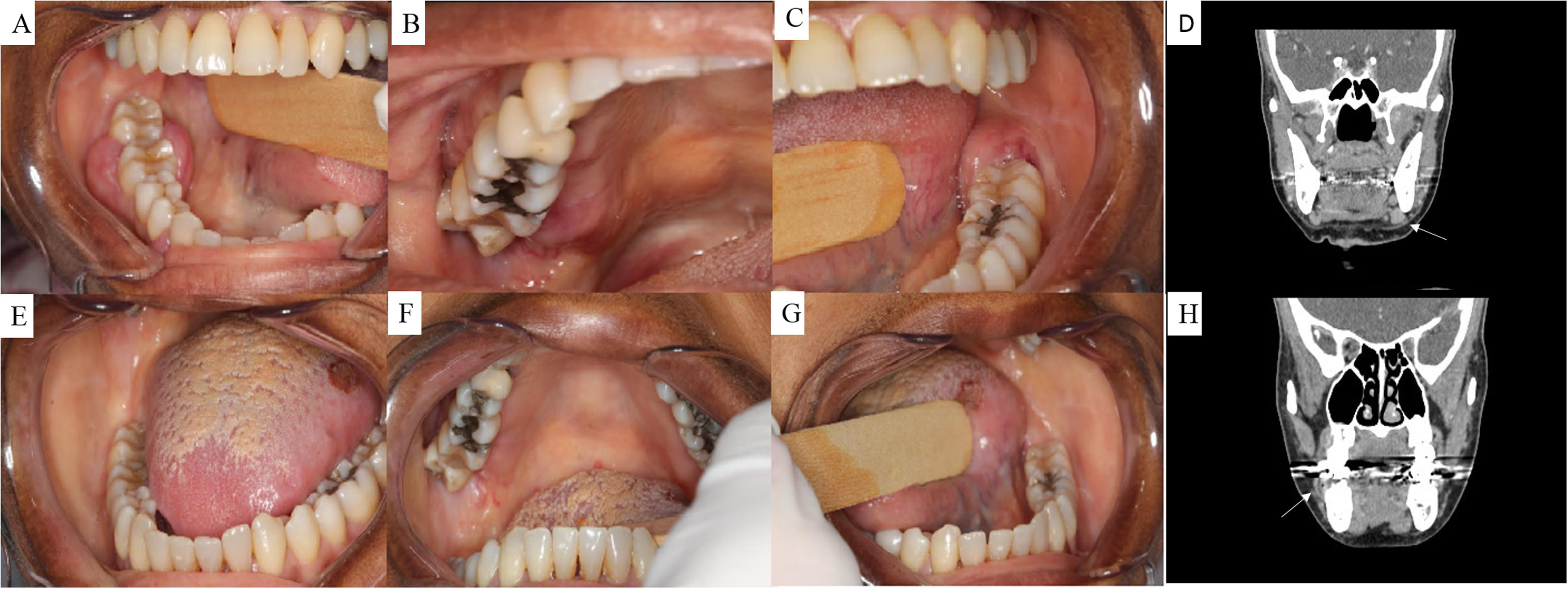
The biopsy of the cervical lymph node and bone marrow showed grade I FL. Complementary exams, such as computed tomography, revealed diffuse adenomegaly in the cervical (Fig. 1D and H), axillary, and abdominal chains, hemoglobin <12 g/dL, and LDH in 2341 U/L, filled three risk factors for FLIPI current. Therefore, the patient was IV B treated with high-risk FLIPI.
(A and B) Initial clinical aspects of intraoral lesions, presence of nodular lesions in the inserted gums of the right side in the posterior, superior and inferior regions on the buccal vestibule and lingual. (C) Initial clinical aspect of intraoral lesion, presence of a nodular lesion in the inserted gums of the left side in the posterior on the buccal. (E–G) Clinical aspects of the resolution of intraoral lesions after systemic therapy. (D and H) computed tomography, soft tissue window of the cervical region, coronal section, cervical linfoadenopathy on the left (D), and gingival enlargement on the right mandible.
In a few weeks, the patient developed worsening abdominal pain and involvement of the oral cavity with the presence of a nodular lesion in the attached gingiva of the lower molars on the right, retromolar trigone, and hard palate (Fig. 1A–C). Due to the rapid worsening, the patient underwent a biopsy of the gingival mass. Histopathological analysis showed the transformation of follicular lymphoma from grade I to grade III, a disease with behavior that is more aggressive and requiring chemotherapy like diffuse B-cell NHL (DLBCL). Nevertheless, the histological findings in oral biopsy were quite relevant to show the aggressiveness of disease progression.
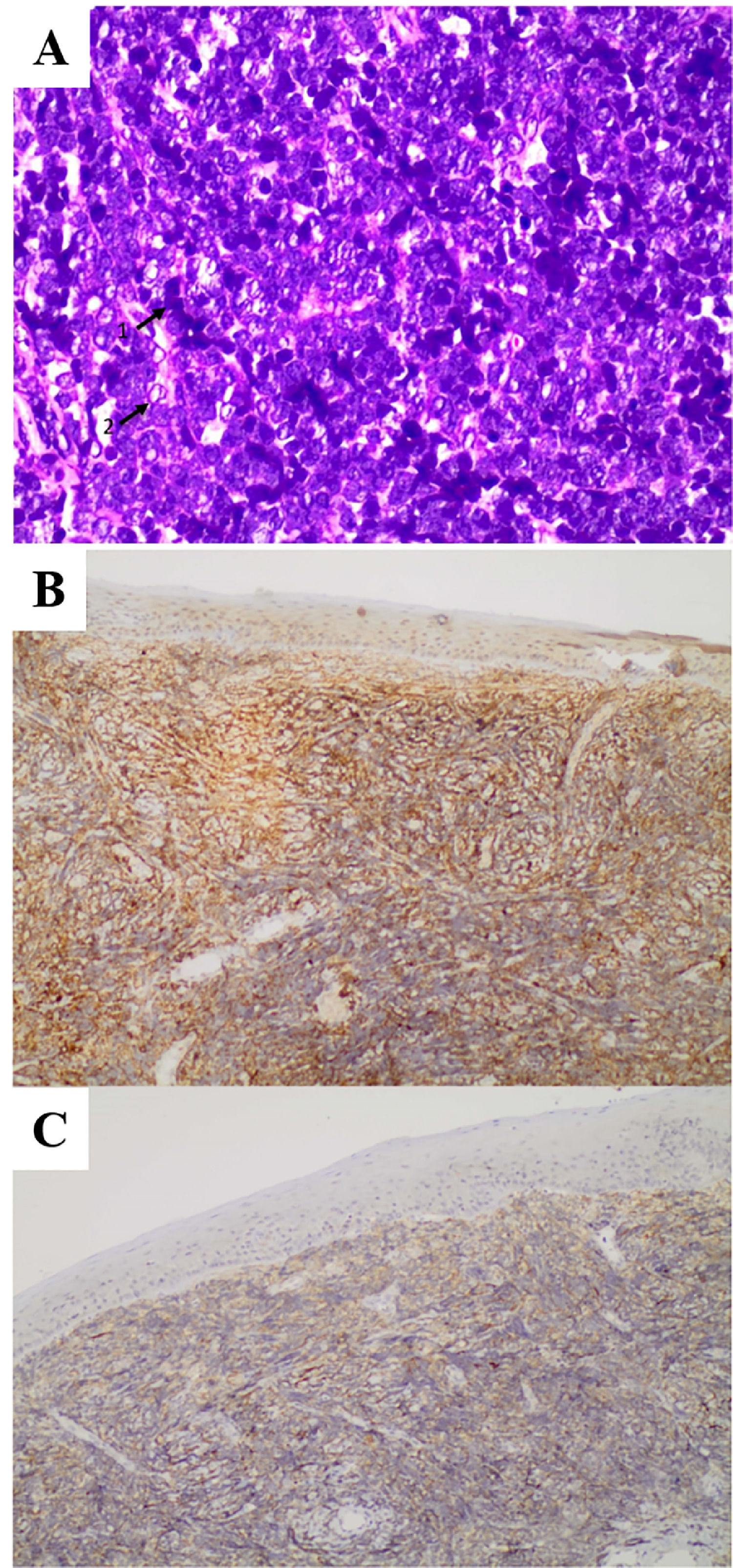
The histopathological features from infiltration in oral mucosa showed stroma infiltration by diffuse growth lymphoid neoplasm, comprising small and intermediate cells of cleaved nuclei at times, not cleaved at others. Positive stains were CD20+, CD10+, and Bcl-2+ lymphoproliferative cells. Negative stains were anti-CD3 and BCL6 leading to centrofollicular B-cell NHL diffusely infiltrated in the squamous mucosa (Fig. 2).
(A) Pathological assessment: H&E staining, magnification ×20, the photomicrograph shows mononuclear infiltrate with hyperchromatic cells (¹) and neoplastic cells with larger chromatin and loose nuclei (²), where you can use the small nucleoli corresponding to the centroblasts, which are the immature lymphocytes of lineage B. (B) Photomicrograph showing immunostaining for CD20. Immunohistochemistry 10×. (C) Photomicrograph showing immunostaining for CD10. Immunohistochemistry 10×.
Prior to the oral cavity biopsy, a retroperitoneal lymph node biopsy was performed which showed positive stains to CD10+, CD20+, Ki67+, CD3+, negative BCL-6, CD5, and cyclin D1. The proliferative index evaluated for MIB-1 antibodies was greater than 90% (Figure 2). Morphological and immunohistochemical findings were suggestive of high-grade follicular lymphoma.
After one week of chemotherapy protocol R-CHOP with prednisone 20 mg, vincristine 2 mg, rituximab 630 mg, doxorubicin 84 mg, and cyclophosphamide 1 g, the gingival mass in the oral cavity presented regression as shown in Figure 1E–G and the LDH dropped to 686.0 U/L. Despite this involution in the oral cavity, the patient presented a worsening systemic condition and died two weeks after starting the therapy.
DiscussionFL is characterized by diffuse lymphadenopathy, bone marrow involvement and splenomegaly, but extranodal involvement is less common. Cytopenia is relatively common, but constitutional symptoms of fever, night sweats, and weight loss are uncommon in the absence of transformation to DLBCL. The overall survival time is on average 20 years through the therapeutic advent of rituximab. However, as it is considered incurable with treatment, histologic transformation and recurrent FL are the main conventional cause of death in patients with this disease, despite their prolonged survival.8,9
In FL, the neoplastic cells are follicle-center B cells, comprised of a mixture of centrocytes (small, nondividing B cells) and centroblasts (large, proliferating B cells) arranged into follicular structures. The centrocytes and centroblasts visible during microscopy are the reference to classify the degrees of FL. In the case, the patient was initially classified as FL grade I with a proliferative index of approximately 25%. A few days later, her clinical condition worsened, and she underwent a retroperitoneal lymph node biopsy which showed a proliferative index of 90%, being staged as high-grade FL. It was only after oral cavity biopsy that the transformation to NHL of large centrofollicular B cells that diffusely infiltrated the squamous mucosa was observed, an appropriate classification when there is a diffuse growth containing >15 centroblasts per high-power field.2,6
Due to the difficulty of stratifying risk because of several issues, the last consensus of specialists opted to classify FL in classics (cFL), which encompass grades I, II, and III, because there are no significant differences; follicular large B-cell lymphoma (FLBL); and FL with unusual features (uFL).10
Less than 10% of patients with FL are stage I/II, at this stage of the disease radiotherapy is usually the treatment of choice, and results in 10-year OS (Overall survival) rates of 60–80%; with a median survival of approximately 19 years, patients with high-risk FL have a median survival around 5 years. Most patients with FL have an advanced-stage disease at diagnosis. Patients with advanced-stage FL do not require immediate treatment unless they have symptomatic nodal disease, compromised end organ function, B symptoms symptomatic extranodal disease or cytopenias.6
According to Silva et al., 11–33% of NHL cases occur in the head and neck region and correspond to 2.2% of all neoplasms. In this region, the oral manifestations frequently resemble other diseases including periodontal disease, amyloidosis, osteomyelitis, and other neoplasms. The presence of a nodular lesion in the inserted mandible gums and a darkened lesion on the back of the tongue (Figure 1) are less frequent as a manifestation of lymphoma, making the diagnosis challenging and delaying the beginning of treatment.11
A systematic review conducted by Inchingolo et al. in 2011 showed that diffuse NHL DLBCL is the most common histological subtype of lymphomas in the head and neck region, being the most common type of lymphoid neoplasm in adults, accounting for 40% of cases followed by T-cell lymphoma. Other subtypes include Burkitt lymphoma (BL), lymphoblastic lymphoma, natural killer T cell lymphoma (NKTCL), marginal zone B-cell lymphoma, mantle cell lymphoma, plasmablastic lymphoma (PBL), and lymphoblastic lymphoma7
The transformation from indolent follicular type NHL to diffuse large B cell NHL, DLBCL, is expected in 10 to 70% of cases, associated with rapid progression of lymphadenopathy, presence of extranodal disease, presence of B symptoms, and elevation of LDH, corroborate the case presented where the patient evolves from a low-grade I FL, initially diagnosed via lymph node biopsy to high-grade FL NHL evidenced in oral mucosa biopsy.3,12
The histologic transformation from an indolent to a more aggressive lymphoma may occur for all histologic subtypes of indolent NHL. The risk of histologic transformation in patients who receive immediate treatment versus patients who are observed appears to be similar. The average survival of patients who have undergone disease transformation is about 12 months. In the case presented, the disease changed very quickly and had an impact on survival.2,13
Considering that diffuse FL can affect multiple organs when the disease mimics signs of involvement in the mouth, the expected facility of surgical access to the oral cavity can aid in the diagnosis and accelerate the beginning of treatment. In the case described, after the evolution of the disease was diagnosed, the patient immediately started the institutional protocol of chemotherapy with complete resolution of nodular lesions and partial resolution of blackened patches.5,7
Oropharyngeal lymphomas are the second most common malignant disease in the oral region, after squamous cell carcinoma, and the most frequent non-epithelial malignant neoplasia in the maxillofacial region. They generally occur in the Waldeyer's tonsillar ring (pharyngeal tonsil or tubal tonsil). Lymphomas within the oral cavity account for less than 5% of all oral malignancies and typically affect the palatine tonsils and the palate. The most common sites of DLBCL include the tonsils, palate, maxilla, mandible, and parotid glands where it involves both the soft tissues and bones. Clinically, DLBCL of the oral and maxillofacial regions present as single or multiple rapidly growing, painless, or symptomatic swellings with covering intact or ulcerated mucosa.6
A systematic review carried out by Silva et al. in 2016, reports that the presence of a nodular lesion on the attached gingiva of the mandible as a manifestation of lymphoma is less frequent.11 FL cells express monoclonal immunoglobulin light chain, CD19, CD20, CD10, and BCL-6, and are negative for CD5 and CD23. In virtually all cases, FL cells overexpress BCL-2 protein due to t(14;18).14
The histologic transformation is very complex with the acquisition of multiple cytogenetic abnormalities in the low-grade lymphoma cells. In this case, positive stains were CD20+, CD10+, and BLC2+ and negative stains were CD5, cyclin D1, and BCL6 (Figure 2).14
Gene expression profiling has been applied to the study of histologic transformation. Conventional chemotherapy is generally of limited benefit, although a subset of patients are long-term survivors following high-dose therapy and autologous stem cell transplantation. Patients with histological transformation have generally been treated similarly to patients with DLBCL. For patients needing therapy, most patients are treated with the protocol of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) immunochemotherapy.12,14
In the case of RCHOP-refractory, patients of advanced age, physical conditions or comorbidities, reduced dose versions, other non-standard therapies, radiation therapy, autologous stem cell transplantation (ASCT), and recently CART cell therapy may be considered. Despite the advancement of CART cells, new therapies are needed.15
Although the prognosis of FL is excellent, the disease can still be fatal in a subgroup of patients with histologic transformation remaining a major problem. In the case presented, the clinical signs suggested an aggressive disease, which was confirmed only after the oral biopsy. The outcome of patients with NHL seems to be influenced by the combination of specific tumor characteristics and the composition of the tumor microenvironment.1,13,14
NHL is uncommon in the oral cavity; it should always be considered in the differential diagnosis of intraoral malignant diseases. In most instances, dentists may be the first ones to identify intraoral NHL. Therefore, the dental surgeon, as a member of a multidisciplinary team, played a fundamental role in the diagnosis of this case, with less common oral manifestations, of this disease.1,13
Author contributionAll authors contributed equally to the writing of this case report.