The aim of this study was to evaluate the prevalence of pre-sarcopenia and bone mineral density after hematopoietic stem cell transplantation.
MethodsThe study group consisted of over 18-year-old patients who had been submitted to allogeneic transplantation at least one year previously. Patients and healthy controls were matched by sex, ethnic background, age, and body mass index. Body composition and bone mineral density were measured by dual-energy X-ray absorptiometry. A 24-h food recall and food frequency survey were performed. The biochemical evaluation included calcium, parathormone and vitamin D. Eighty-seven patients (52 men; age: 37.2±12.7 years; body mass index: 25±4.5kg/m2) were compared to 68 controls [31 men; age 35.4±15.5 years (p=0.467); body mass index 25.05±3.7kg/m2 (p=0.927)].
ResultsThere was no significant difference in the dietary intake between patients and controls. The mean levels of vitamin D were 23.5±10.3ng/mL; 29 patients (41.0%) had insufficient and 26 (37.14%) deficient levels. A higher prevalence of reduced bone mineral density was observed in 24 patients (25%) compared to 12 controls (19.1% – p<0.001). Pre-sarcopenia was diagnosed in 14 (14.4%) patients and none of the controls (p=0.05). There was a higher prevalence of pre-sarcopenia (66%) in patients with grades III and IV compared to those with grades 0-II graft-versus-host disease (10.9%) (p=0.004).
Conclusionpatients submitted to transplantation had a higher prevalence of pre-sarcopenia and greater changes in bone mineral density compared to controls; the severity of graft-versus-host disease had an impact on the prevalence of pre-sarcopenia.
Hematopoietic stem cell transplantation (HSCT) is a therapeutic modality used to treat malignant or benign diseases. Scientific advances have allowed an increasing number of transplants and longer disease-free survival. Consequently, there is an increment in post-transplant comorbidities secondary to the disease, conditioning regimen or complications, such as graft-versus-host disease (GVHD). Changes in bone mineral density (BMD) may occur due to the use of glucocorticoids, reduced physical activity, low exposure to sunlight, reduction in lean body mass, and vitamin D deficiency. These changes are observed as early as the first months after HSCT or as late as ten years after the procedure.1–4 Recently, sarcopenia has been described after several types of transplants such as liver, kidney and lung, and may influence the outcome.5–8
The term sarcopenia characterizes loss of function related to loss of skeletal muscle mass. It is denominated pre-sarcopenia when only loss of muscle mass is detected. The etiology is multifactorial, but usually occurs due to neurodegenerative, endocrine or chronic diseases, malnutrition or lack of exercise, which leads to muscle atrophy.9 After HSCT, the association of pre-sarcopenia and sarcopenia with the pre-existing disease may worsen the patient's baseline condition, increasing the risk of fractures, especially when associated with reductions in BMD. The early diagnosis of sarcopenia may allow preventive and/or curative treatment of these patients. This research evaluated the prevalence of pre-sarcopenia and changes in BMD in a group of HSCT patients.
MethodsThis observational, transversal study enrolled over 18-year-old patients, regardless of ethnic background or sex, who underwent allogeneic HSCT at the Bone Marrow Transplant Unit of the Hospital de Clinicas da Universidade Federal do Paraná (STMO-HC-UFPR). The sample was selected by convenience; patients were invited to participate during their routine visit. To avoid the consequences of acute bone marrow transplantation complications, patients who had been transplanted less than one year previously were excluded, as were patients with a diagnosis of Fanconi anemia. A control group (CG) was formed of healthy subjects matched with the study group (SG) by sex, age, ethnic background, and body mass index (BMI). Patients and controls performed dual-energy X-ray absorptiometry (DXA) in a whole-body scanner (Lunar Prodigy; GE Medical Systems, Madison, WI, USA) used in conjunction with enCORE 2002 software (GE Medical Systems) to assess the body composition. The software provides data about lean body mass (bone mass plus fat-free mass), bone-free lean mass (lean mass minus fat-free mass), fat mass, and bone mineral density (BMD). Blood samples were collected for biochemical analysis, and a review of hospital records was carried out to search for data regarding the HSCT.
The BMD of total body, lumbar spine (LS), and femur (neck and total) were evaluated with the results being categorized as normal or abnormal following the International Society For Clinical Densitometry (ISCD).10 The percentage of lean mass (%LM) and appendicular lean mass (ALM) were calculated.
Diagnosis of pre-sarcopeniaThe diagnosis of pre-sarcopenia was performed considering three criteria available in the literature. Patients were categorized according to BMI as normal (BMI<25kg/m2) or obese (BMI>25kg/m2). After evaluating the ALM and for those with a normal BMI, the criterion of Baumgartner et al.11 was used, which defines the reduction of appendicular skeletal muscle mass as two standard deviations (SDs) below the mean of young healthy controls, matched with the same ethnic group of the New Mexico population. Values <5.45 for women and <7.26 for men were considered positive. For individuals with BMI ≥25kg/m2, the diagnosis of pre-sarcopenia was calculated based on the criterion of Delmonico et al.12 Initially, a linear regression model was adjusted for ALM (kg) including height (m) and total fat mass (kg) as explanatory variables. The residuals of the regression were used to identify individuals with a lean mass lower than the value predicted for a given fat mass (given by an equation derived from the model). A positive residual indicates a relatively muscular individual, whereas a negative residual indicates an individual with sarcopenia. The equations derived from the model were the following: for males – ALM (kg)=−30.54+30.88×height (m)+0.0823×total fat mass (kg); and for females – ALM (kg)=−12.45+15.79×height (m)+0.1081×total fat mass (kg). The 20th percentile of the distribution of residuals was used as the cut-off point for the diagnosis of sarcopenia according to the ALM adjusted for fat mass as previously defined. In this patient sample, the cut-off point corresponded to residuals of −2.021 for men and −1.082 for women.
Finally, the ALM/BMI criterion of The Foundation for the National Institute of Health (FNIH) was used, and the values of <0.789 for men and <0.512 for women were considered pre-sarcopenia.13
Food intake was assessed in an interview conducted by a registered dietician with a 24-h recall questionnaire based on type and quantities of food consumed the day before the interview, a tool appropriate to assess the consumption of a nutrient with a specific dietary recommendation.14,15 Calcium, vitamin D, protein, and total calorie intake were calculated by AVANUTRI®, a nutritional assessment program, following the reference of the “recommended dietary allowance” (RDA) according to sex and age. The intake was considered adequate when it reached or exceeded the RDA. The RDA of calcium for ages 19–50 years is 1000mg and for >50 years, it is 1200mg; 15μg of vitamin D is recommended for individuals between 19 and 70 years.16
Biochemical analysisSerum levels of parathormone (PTH) [chemiluminescence−normal value (NV)=15–68.3pg/mL] calcium (Arzenago III−NV=8.9–10mg/dL) and vitamin D (chemiluminescence−Liaison®−25OHD) were analyzed. The 25OHD results were classified according to the latest guidelines for vitamin D levels of the Endocrine Society: deficiency below 20ng/mL, insufficiency between 21 and 29ng/mL and normal over 30ng/mL.17
Statistical analysisData are presented as means±SD except where otherwise specified. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM Corporation, Armonk, NY, USA). For the variables evaluated, the normality of the data distribution was evaluated using the Kolmogorov–Smirnov test. Student's t-test for independent samples or the nonparametric Mann–Whitney test was used to compare quantitative variables between the two groups. Fisher's exact test and the chi-square test were used to assess the association between two qualitative variables in the preliminary statistical analysis. p<0.05 were considered statistically significant. Correlations were sought using the Pearson and Spearman coefficients for variables with normal and non-parametric distributions, respectively. For all analyses, a two-sided p<0.05 was considered to indicate statistical significance. More than two groups were compared using the model of analysis of variance (ANOVA) and the least significant difference (LSD) test for multiple comparisons.
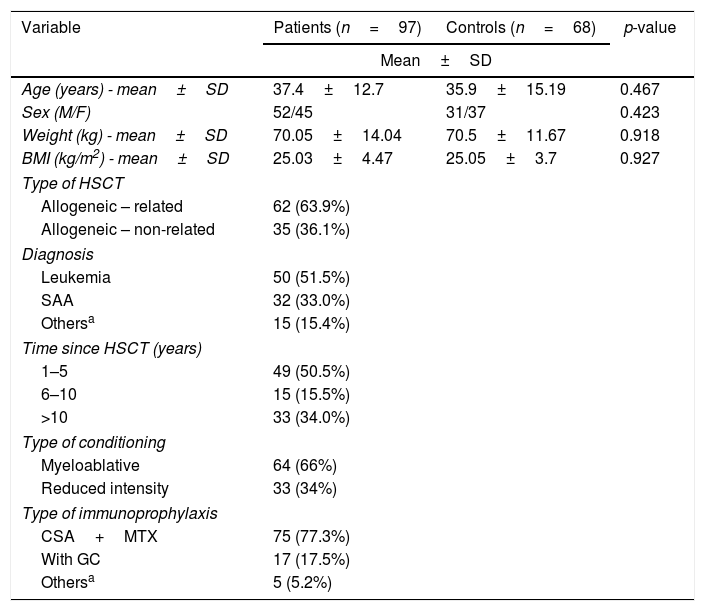
ResultsThe sample was initially composed of the first 100 patients (SG) who agreed to participate and who met the selection criteria. As three patients did not perform bone densitometry, they were excluded and the final sample size was 97 patients (n=52–53.6% male). The mean age was 37.4±12.7 years, with an average weight of 70.1±14kg, mean height of 1.67±0.09m and mean BMI of 25±4.5kg/m2. Based on the BMI, 14 (14.4%) patients were classified as obese, 29 (29.9%) overweight, four (4.1%) underweight and 50 (51.6%) normal. Twenty-three patients suffered GVHD; five patients had grade I, 12 grade II, three grade III and three grade IV. A median cumulative dose of glucocorticoids of 7181mg (55–37,275mg, equivalent of prednisone) was used by 46 out of 89 patients, and only eight patients were taking glucocorticoids at the time of this evaluation.
The CG consisted of 68 apparently healthy individuals with a mean age of 35.9±15.2 years (n=31–45.5% males). The mean BMI was 25.05±3.7kg/m2 with 39 (57.3%) controls being classified as normal, 23 (33.8%) as overweight, and six (8.9%) as obese, a distribution similar to that of the patients. Table 1 shows the clinical characteristics of patients and controls and diagnosis of the underlying disease.
Clinical characteristics of patients and controls.
| Variable | Patients (n=97) | Controls (n=68) | p-value |
|---|---|---|---|
| Mean±SD | |||
| Age (years) - mean±SD | 37.4±12.7 | 35.9±15.19 | 0.467 |
| Sex (M/F) | 52/45 | 31/37 | 0.423 |
| Weight (kg) - mean±SD | 70.05±14.04 | 70.5±11.67 | 0.918 |
| BMI (kg/m2) - mean±SD | 25.03±4.47 | 25.05±3.7 | 0.927 |
| Type of HSCT | |||
| Allogeneic – related | 62 (63.9%) | ||
| Allogeneic – non-related | 35 (36.1%) | ||
| Diagnosis | |||
| Leukemia | 50 (51.5%) | ||
| SAA | 32 (33.0%) | ||
| Othersa | 15 (15.4%) | ||
| Time since HSCT (years) | |||
| 1–5 | 49 (50.5%) | ||
| 6–10 | 15 (15.5%) | ||
| >10 | 33 (34.0%) | ||
| Type of conditioning | |||
| Myeloablative | 64 (66%) | ||
| Reduced intensity | 33 (34%) | ||
| Type of immunoprophylaxis | |||
| CSA+MTX | 75 (77.3%) | ||
| With GC | 17 (17.5%) | ||
| Othersa | 5 (5.2%) | ||
SD: standard deviation; M: male; F: female; BMI: body mass index; HSCT: hematological stem cell transplantation; SAA: severe aplastic anemia; CSA: cyclosporine; MTX: methotrexate.
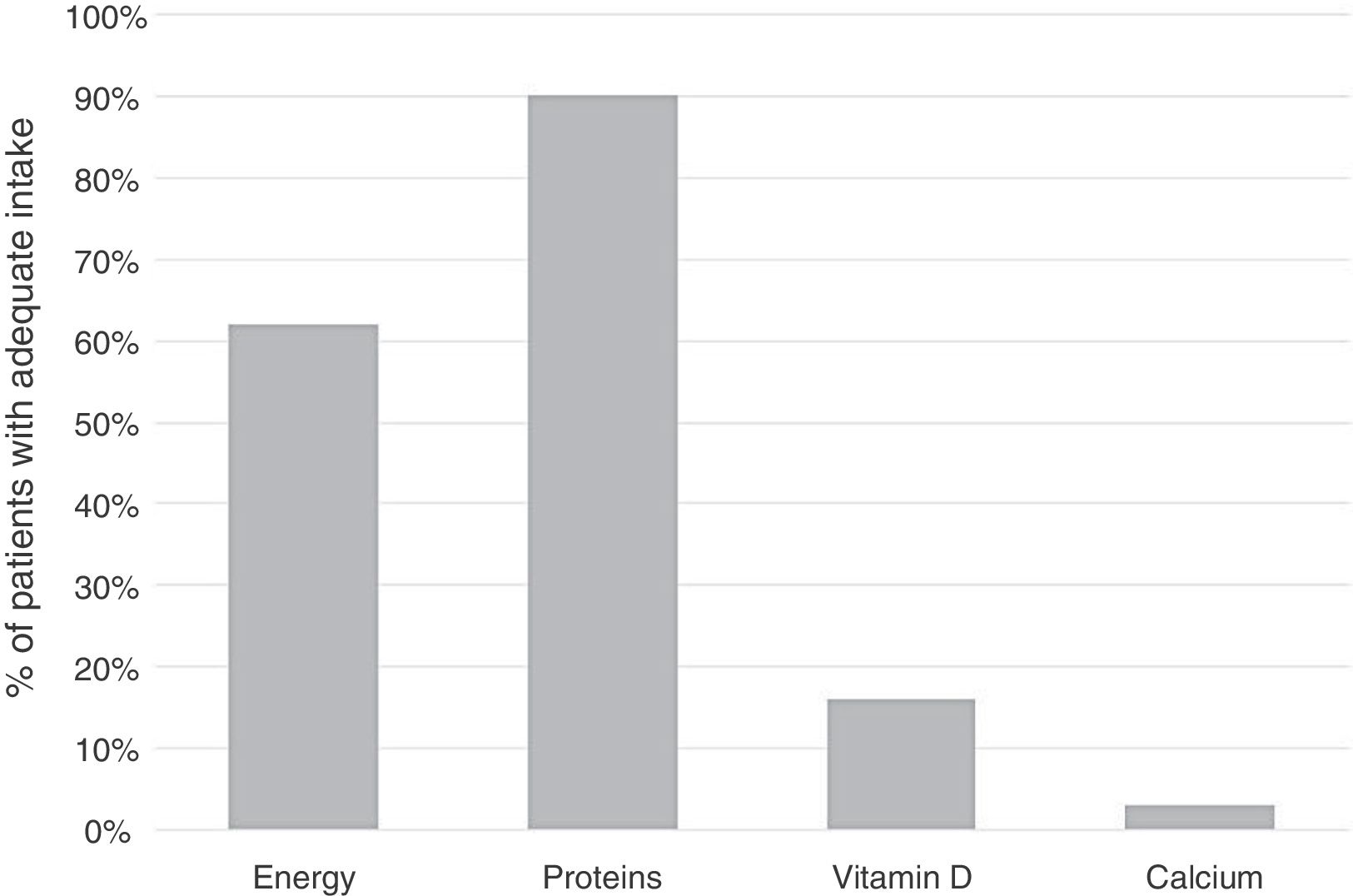
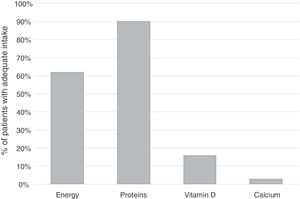
The mean consumption of protein was 78.7±38g/day (1.2±0.6g/kg), which was appropriate in 80.4% of patients. The average daily calorie intake was 1892±852kcal, a suitable total energy expenditure (TEE) in 36% and greater than the necessity in 26% of the patients. The mean daily intake of calcium was 456±347mg and the median intake of vitamin D was 1.91±6.95μg considered insufficient according to the RDA in 96.4% and 83.5% of patients, respectively (Figure 1).
No significant difference was found in the food consumption between patients and controls. In addition, no difference was observed in the food consumption between patients with abnormal or normal BMD. The mean calorie intake was 1742±513kcal/day and 1951±938kcal/day in patients with abnormal and normal BMD, respectively (p=0.989). Protein intake was 73.7±38.1 and 80.7±38.2g/day in those with abnormal BMD and normal BMD, respectively (p=0.441). Calcium intake was 387±323 and 473±353mg/day in patients with abnormal and normal BMD, respectively (p=0.294) and the intake of vitamin D was 1.89±4.13 and 1.88±7.73μg/day in patients with abnormal and normal BMD, respectively (p=0.991).
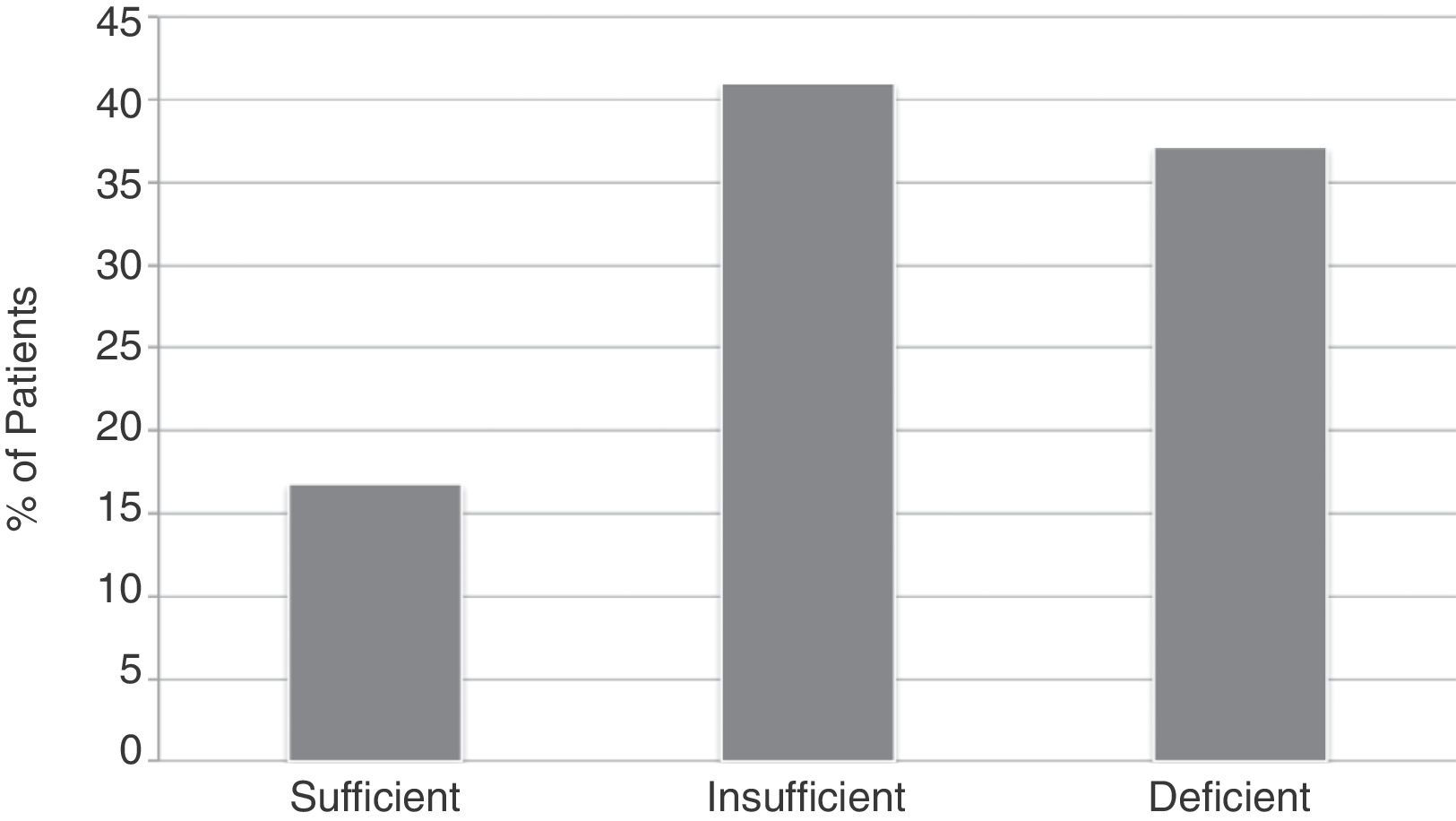
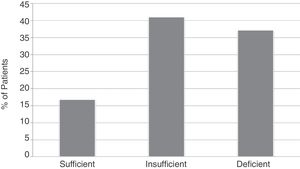
The mean serum level of vitamin D was 23.5±10.3ng/mL. The levels were sufficient in 16 (22.8%) patients, with an average of 37.59±8.19ng/mL; insufficient in 29 (41%), with a mean of 23.98±2.60ng/mL; and deficient in 26 (37.14%), with an average of 13.65±4.85ng/mL (Figure 2). The mean level of PTH was 85.7ng/mL (range: 29.9–179.0) and the mean serum calcium was 9.4±0.5mg/dL.
Considering the criteria of Baungartner and Delmonico, pre-sarcopenia was diagnosed in 33 (34%) patients and in only three (4.6%) controls (p<0.001) with no significant difference in respect to sex – 18 (40%) women and 15 (28.8%) men (p=0.287). A tendency was observed for fewer diagnoses over time after HSCT: pre-sarcopenia was present in 44.9%, 26.7% and 21.2% of cases 1–5 years, 6–10 years and more than 10 years after HSCT, respectively (p=0.069). Using these diagnostic criteria, the prevalence of pre-sarcopenia was higher among patients who underwent unrelated (46.9%) compared to related (24.6%) allogeneic HSCT (p=0.037). The prevalence of pre-sarcopenia did not change with the type of conditioning, immunoprophylaxis, diagnosis, serum calcium, vitamin D and PTH levels, or in relation to dietary intake of calcium, vitamin D, calories or protein.
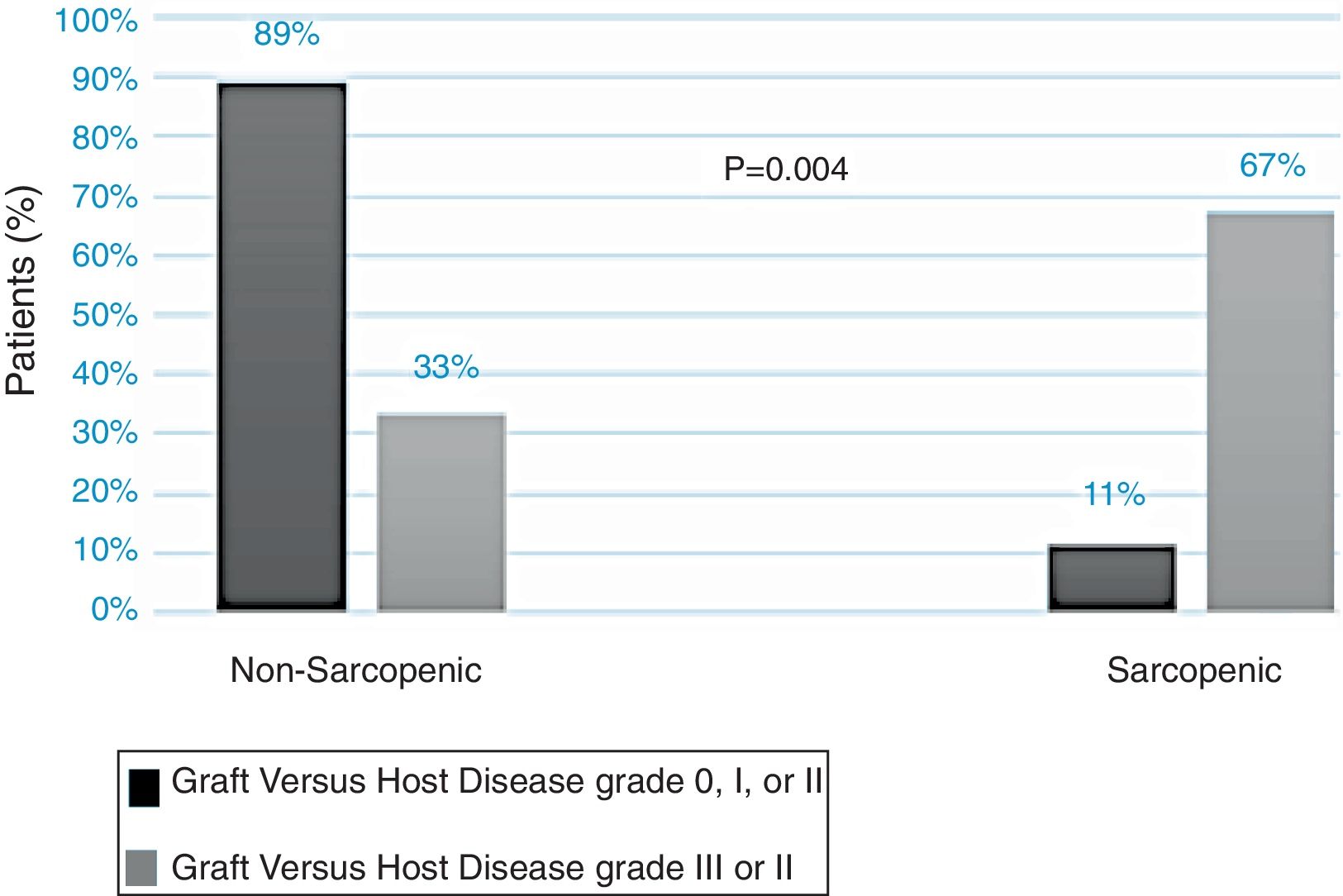
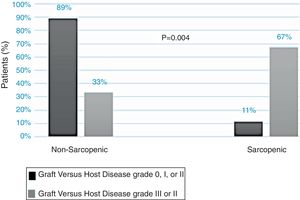
Regarding assessments using the diagnostic criterion of the FNIH, there were few diagnoses of pre-sarcopenia: 14 (14.4%) of the SG and none of the CG (95% confidence interval: 7.4–21.4%; p=0.05). In addition, no difference was observed between sex [9 (11.2%) women and 6 (7.3%) men; p=0.428] and time after HSCT, type of HSCT, type of conditioning, immunoprophylaxis, diagnosis, or other variables. The prevalence of pre-sarcopenia was different according to the severity of the GVHD: found in 67% of patients with GVHD grade III and IV and in only 11% of those with grade I and II (p=0.004) (Figure 3).
Abnormal BMD was observed in 24 (25%) of patients in the SG and in 12 patients (19.1%) in the CG (p=0.441). Compared to men, more women in both groups had abnormal BMD [18–40% women and 6–11.76% men in SG (p=0.002) and 11–31.4% women and 1–3.6% man in the CG (p=0.008)]. All women were amenorrheic after HSCT. There was no association of BMD with the diagnosis of the underlying disease (p=0.09), type of HSCT (p=0.805), conditioning regimen (p=0.329), immunoprophylaxis (p=0.126), presence of GVHD (p=0.417), cumulative dose of corticosteroid (p=0.416) or any parameter of food intake or body composition evaluated (p>0.05).
DiscussionThis study evaluated lean mass, BMD, and food intake in patients after HSCT with the results showing a high prevalence of decreased BMD and pre-sarcopenia, especially in patients with GVHD and low levels of vitamin D.
Abnormal BMD was present in 25% of the SG, higher in women (40%), and similar to the prevalence observed in climacteric women after liver transplantation (14.6% of osteoporosis and 35.4% of low bone mass).18 Various mechanisms explain changes in bone metabolism after allogeneic HSCT such as the decreased bone formation related to the pre-HSCT conditioning regimen, as well as medications such as cyclosporine and glicocorticoides,19 besides the severity of the underlying disease, that can compromise bone mineral density and muscle strength.20,21 Nevertheless, in this study neither the underlying disease nor the use of glucocorticoids or any variable related to the HSCT was correlated to the BMD. Another factor that may explain the higher prevalence of BMD changes in women is that the use of alkylating agents such as cyclophosphamide, methotrexate, and busulfam, with or without ovarian radiation, leads to premature ovarian failure, as noted in 18 patients in this study. Both chemotherapy and radiotherapy in under 20-year-old women are associated with a higher prevalence of early menopause: 42% of patients by age 31 compared to 5% in controls.22,23
The SG patients had low serum levels of vitamin D with secondary hyperparathyroidism, and 60% of patients reported sporadic sun exposure following medical advice to prevent GVHD after HSCT.24 This high prevalence of vitamin D deficiency (77.2%) is similar to that found in renal transplant patients (79%), also justified by low exposure to sun.25
Independent of the criterion used, the diagnosis of pre-sarcopenia was more frequent in the SG and in those who underwent unrelated HSCT, similar to what was observed in 54 patients aged between 5 and 25 years old, who performed HSCT during childhood.26
Although the literature associates sarcopenia with advanced age, the patients in this study were young (37.4±12.7 years) and pre-sarcopenia was present in 15–34%, which can have a great impact on the quality of life. Estimations of the prevalence of sarcopenia vary with age, from 30% in over 65-year olds to more than 50% in those aged 80 or more.25 Although few data are available on the prevalence of sarcopenia in the Brazilian population, it is clear that the study population had sarcopenia at a lower age and it was more prevalent in the first five years after transplantation. Studies on humans and animals have shown muscle wasting and cachexia related to cancer27–29 possibly due to the oxidative stress and chronic inflammation immediately after HSCT. In this study, the exclusion of patients who underwent HSCT less than one year prior to the evaluation was an attempt to eliminate the impact of acute complications of HSCT on sarcopenia and BMD. Sarcopenia was observed in 66.2% patients before liver transplantation, with 75% of patients without sarcopenia before the transplant developing the disease after within a mean of 19.3±9 months; no association between nutritional status and post-transplant factors such as the immunosuppression regimen were identified.30 In this study, we did not find any relationship of the conditioning regimen or the use of immunosuppression with the prevalence of sarcopenia.
The diagnostic criteria were concordant with a higher prevalence of pre-sarcopenia in the SG. However, the method proposed by the FINH proved to be more conservative in both groups, compared to the Baungartner and Delmonico criteria. Furthermore, the clinical correlation observed between the severity of GVHD and the diagnosis of pre-sarcopenia was observed only with the FNIH method, which has important clinical relevance for these patients.
ConclusionPatients undergoing allogeneic HSCT had a higher prevalence of BMD changes and higher pre-sarcopenia rates when compared to the controls. Concerning the factors related to HSCT, the presence of severe GVHD was associated with a higher prevalence of pre-sarcopenia.
Conflicts of interestThe authors declare no conflicts of interest.