Knowing the information regarding the panorama of lymphoma diagnosis in patients treated in the Brazilian Public Unified Health System from the last 10 years is a challenge for Strategic Health Planning.
ObjectiveTo characterize the Brazilian population with lymphoma treated in the Brazilian Public Unified Health System between 2008 and 2017 regarding staging, sex, residence site and mortality.
Material and methodsA descriptive, retrospective, and longitudinal trial with secondary data from DataSUS (SIA/SUS and SIM/SUS) obtained from patients with ICD-10 C81−85.
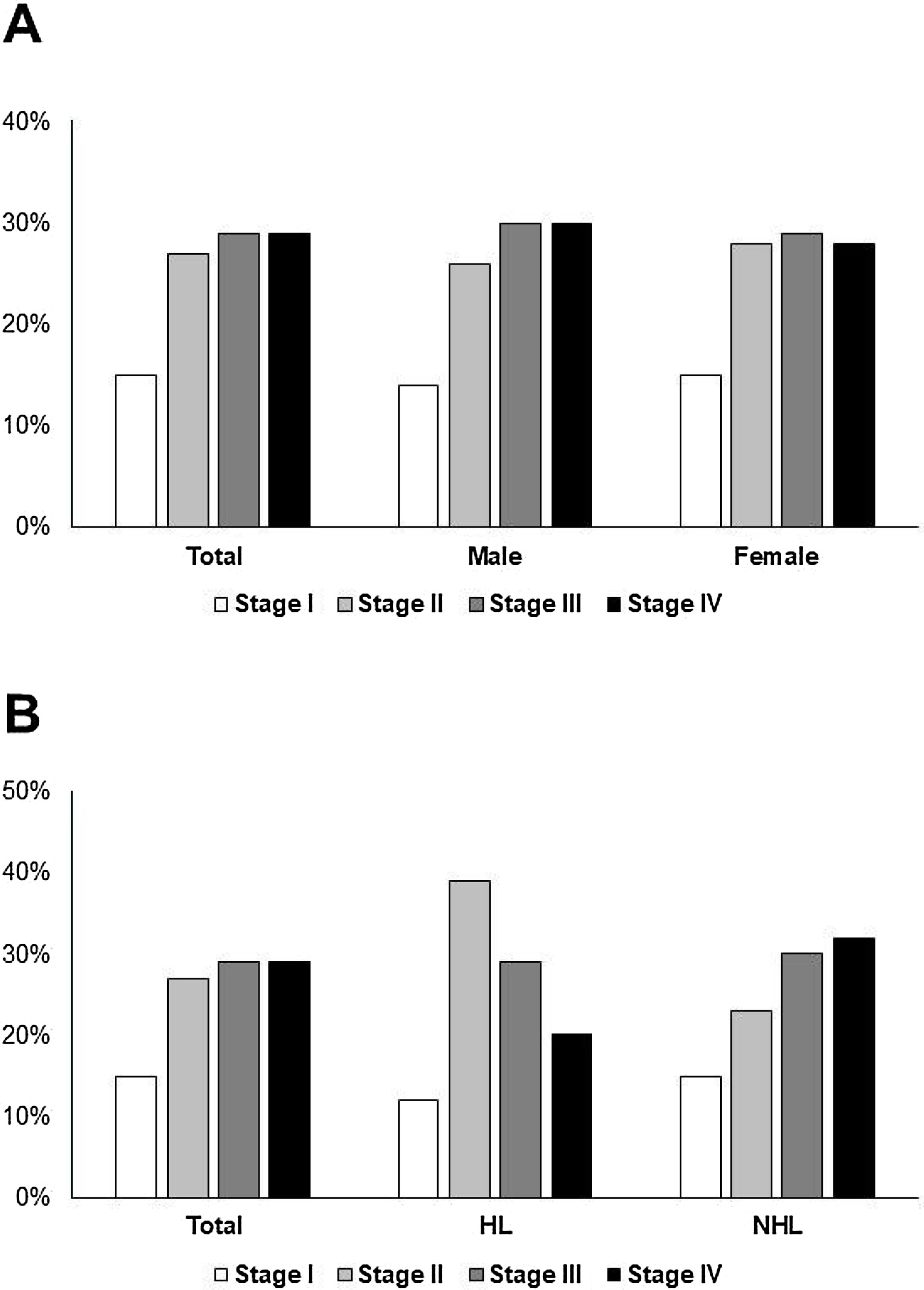
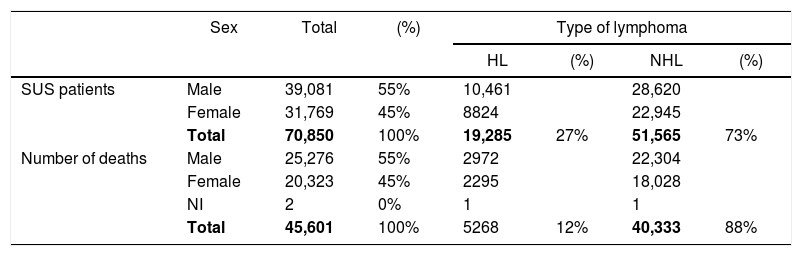
ResultsThere were 70,850 lymphoma cases between 2008 and 2017, of which 55% were male, the median age was 51 years, and 27% had Hodgkin Lymphoma. Most patients (56%) were treated outside the residence city. São Paulo State accounted for 25% of patients. Treatment initiation took more than 60 days in 27% of cases. A total of 45,601 deaths were due to lymphoma (12% Hodgkin Lymphoma and 88% Non-Hodgkin Lymphoma), with a median age 63 years, and were mainly males (55%). Staging data were inadequate in 23% of patients, and analysis was performed only on the valid records. Advanced disease was diagnosed in 58% of patients (60% male; 57% female) and was more common in Non-Hodgkin Lymphoma (62%) versus Hodgkin Lymphoma (49%).
DiscussionLate diagnosis interferes with mortality rates. Health promotion and cancer prevention campaigns, especially targeting the male public, and training for early diagnosis and early treatment are needed.
ConclusionEffective measures for early diagnosis and treatment are urgently needed for lymphoma control.
Data from Brazil show that cancer mortality is increasing rapidly. Between 2008 and 2016, the number of deaths from cancer experienced an average growth rate of 3.5% per year. In 10% of Brazilian cities, cancer is already the leading cause of death and, if the same scenario continues, it is estimated that by 2029 it will be the leading cause of death in the country.1–3
Regarding the epidemiology of lymphoma, these same data showed that lymphoma is among the cancers with increased mortality, in both absolute number and crude rate, as the number of deaths from lymphoma increased by 88% over 20 years (1997–2016) and 8% over 5 years (2012–2016). Over 20 years (1997–2016), the crude death rate for non-Hodgkin lymphoma (NHL) in adults, between 20 and 49 years of age and over 50 years of age, increased by 0.9% and 1.6% per year, respectively.1
Although lymphoma is not among the most common cancers in Brazil, it is estimated that there were 12,710 new cases in 2019, corresponding to 3% of all new cancer cases4 and 6 cases per 100,000 inhabitants. Thus, lymphoma has a significant healthcare impact.1
Mortality in lymphoma is known to be directly related to the disease stage at diagnosis.5 Late diagnosis also affects the health budget, as the treatment of advanced cancers generally costs 13 times more than that of early stage cancers; specifically for lymphomas, the cost in stage IV is 35% higher than that that in stage I.6
Given this context of increasing mortality from lymphoma, its considerable incidence and the higher cost of treating advanced stages, implementing actions for disease control will positively contribute to health gains. Since cancer strategies include, among other factors, prevention, screening and diagnosis, early diagnosis becomes a critical factor for cancer control and the attainment of better outcomes with treatment.5
Therefore, to delineate the action of cancer care and to outline effective strategies to improve outcomes on lymphoma care, it is necessary to know the actual diagnostic scenario. Unraveling the landscape of diagnostic staging in Brazil will provide data to support strategic health care planning by promoting management mechanisms to reduce lymphoma deaths.
The Department of Information Technology of the Brazilian Public Unified Healthcare System (DataSUS) manages open government data on population healthcare. DataSUS maintains epidemiological information systems, such as the Brazilian Public Unified Healthcare System Mortality Information System (SIM-SUS) and the Brazilian Public Unified Healthcare System Outpatient Information System (SIA-SUS), which record information on the dispensation of drugs, chemotherapy, radiotherapy and outpatient procedures.8
To determine the current situation of lymphoma diagnosis in Brazil, this trial used DataSUS data on patients diagnosed from 2008 to 2017. The primary objective of this trial was to characterize the Brazilian population with lymphoma treated in the Brazilian Public Unified Healthcare System (SUS) from 2008 to 2017, concerning diagnosis, gender, residence site, staging, age at diagnosis and mortality.
Material and methodsThis trial is descriptive, retrospective and longitudinal and is based on secondary data available online from DataSUS. The study population is composed of patients from all Brazilian States who received primary 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) diagnoses of Hodgkin Lymphoma (HL) (C81), follicular lymphoma (FL) (C82), diffuse large B-cell lymphoma (DLBCL) (C83), cutaneous and peripheral T-cell lymphoma (CPTCL) (C84) or other specified and unspecified types of non-Hodgkin lymphoma (C85), with pathological identification dates (diagnosis) from 2008 to 2017, and who underwent at least one procedure registered by the High Complexity Procedure Authorization (APAC) of Chemotherapy and Radiotherapy. The mortality assessment included deaths from 2008 to 2017 with ICD-10 of HL (C81) or NHL (C82-C85).
From the APAC databases in the SIA-SUS, it is possible to obtain the encrypted code of each patient's National Health Card (CNS), age at diagnosis, gender, residence site, diagnosis date and staging. With the CNS encrypted codes, duplicate records and/or procedures were eliminated, allowing only the first record of each patient in the evaluated period to be considered for analysis. From SIM-SUS, age of death, gender and site of death were obtained. This information was extracted from the databases using the Tabwin software version 3.2, freely available in the DataSUS.
The results are expressed as medians and minimum and maximum values and are presented as graphs and tables confectioned with the Microsoft Office Excel software (Microsoft, Redmond, Washington, USA). Associations among gender, lymphoma types, time to treatment initiation and staging were assessed by the Pearson's Chi-square test. Differences between the proportions of deaths and new diagnoses were analyzed using the Chi-square test for homogeneity.
This trial was approved by the Ethics Committee of the Federal University of São Paulo (CAAE 11893119.8.0000.5505; Project CEP/UNIFESP 0409/2019). The Informed Consent Form was waived because the trial was an analysis that used secondary open source data that are available to the public in the SIA-SUS platform without patient identification.
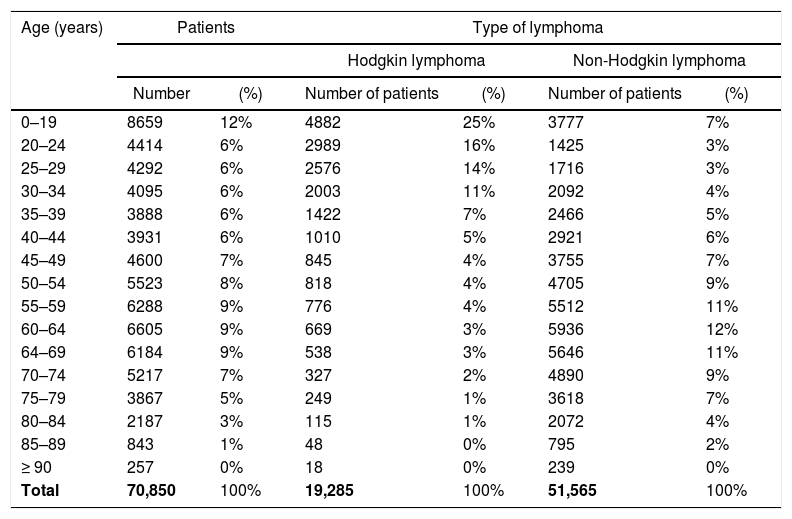
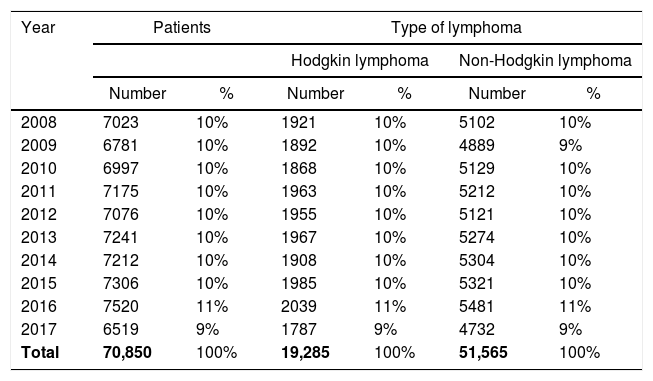
ResultsFrom the SIA/SUS data, 70,850 lymphoma patients were diagnosed from 2008 to 2017 and 39,081 (55%) were male, 19,285 (27%) had HL and 51,565 (73%) had NHL (Table 1). The median age at diagnosis was 51 years (0–99 years) and 12% were of pediatric age (Table 2). The most frequent NHL type was DLBCL (39,012; 55%), followed by FL (6289; 9%). The number of new cases detected, despite variations, remained stable over the analyzed period, with each year representing approximately 10% of the total cases of lymphoma in the period (Table 3).
Absolute numbers and proportions of patients diagnosed with lymphoma under the SUS and deaths from lymphomas in Brazil from 2008 to 2017 according to sex and type of lymphoma.
| Sex | Total | (%) | Type of lymphoma | ||||
|---|---|---|---|---|---|---|---|
| HL | (%) | NHL | (%) | ||||
| SUS patients | Male | 39,081 | 55% | 10,461 | 28,620 | ||
| Female | 31,769 | 45% | 8824 | 22,945 | |||
| Total | 70,850 | 100% | 19,285 | 27% | 51,565 | 73% | |
| Number of deaths | Male | 25,276 | 55% | 2972 | 22,304 | ||
| Female | 20,323 | 45% | 2295 | 18,028 | |||
| NI | 2 | 0% | 1 | 1 | |||
| Total | 45,601 | 100% | 5268 | 12% | 40,333 | 88% | |
HL – Hodgkin lymphoma; NHL – Non-Hodgkin lymphoma.
Absolute numbers and proportions of patients diagnosed with lymphoma from 2008 to 2017 and treated by the SUS, according to the age group at diagnosis and the type of lymphoma.
| Age (years) | Patients | Type of lymphoma | ||||
|---|---|---|---|---|---|---|
| Hodgkin lymphoma | Non-Hodgkin lymphoma | |||||
| Number | (%) | Number of patients | (%) | Number of patients | (%) | |
| 0–19 | 8659 | 12% | 4882 | 25% | 3777 | 7% |
| 20–24 | 4414 | 6% | 2989 | 16% | 1425 | 3% |
| 25–29 | 4292 | 6% | 2576 | 14% | 1716 | 3% |
| 30–34 | 4095 | 6% | 2003 | 11% | 2092 | 4% |
| 35–39 | 3888 | 6% | 1422 | 7% | 2466 | 5% |
| 40–44 | 3931 | 6% | 1010 | 5% | 2921 | 6% |
| 45–49 | 4600 | 7% | 845 | 4% | 3755 | 7% |
| 50–54 | 5523 | 8% | 818 | 4% | 4705 | 9% |
| 55–59 | 6288 | 9% | 776 | 4% | 5512 | 11% |
| 60–64 | 6605 | 9% | 669 | 3% | 5936 | 12% |
| 64–69 | 6184 | 9% | 538 | 3% | 5646 | 11% |
| 70–74 | 5217 | 7% | 327 | 2% | 4890 | 9% |
| 75–79 | 3867 | 5% | 249 | 1% | 3618 | 7% |
| 80–84 | 2187 | 3% | 115 | 1% | 2072 | 4% |
| 85–89 | 843 | 1% | 48 | 0% | 795 | 2% |
| ≥ 90 | 257 | 0% | 18 | 0% | 239 | 0% |
| Total | 70,850 | 100% | 19,285 | 100% | 51,565 | 100% |
Absolute numbers and proportions of patients diagnosed with lymphoma from 2008 to 2017 and treated by the SUS, according to the type of lymphoma and year of diagnosis.
| Year | Patients | Type of lymphoma | ||||
|---|---|---|---|---|---|---|
| Hodgkin lymphoma | Non-Hodgkin lymphoma | |||||
| Number | % | Number | % | Number | % | |
| 2008 | 7023 | 10% | 1921 | 10% | 5102 | 10% |
| 2009 | 6781 | 10% | 1892 | 10% | 4889 | 9% |
| 2010 | 6997 | 10% | 1868 | 10% | 5129 | 10% |
| 2011 | 7175 | 10% | 1963 | 10% | 5212 | 10% |
| 2012 | 7076 | 10% | 1955 | 10% | 5121 | 10% |
| 2013 | 7241 | 10% | 1967 | 10% | 5274 | 10% |
| 2014 | 7212 | 10% | 1908 | 10% | 5304 | 10% |
| 2015 | 7306 | 10% | 1985 | 10% | 5321 | 10% |
| 2016 | 7520 | 11% | 2039 | 11% | 5481 | 11% |
| 2017 | 6519 | 9% | 1787 | 9% | 4732 | 9% |
| Total | 70,850 | 100% | 19,285 | 100% | 51,565 | 100% |
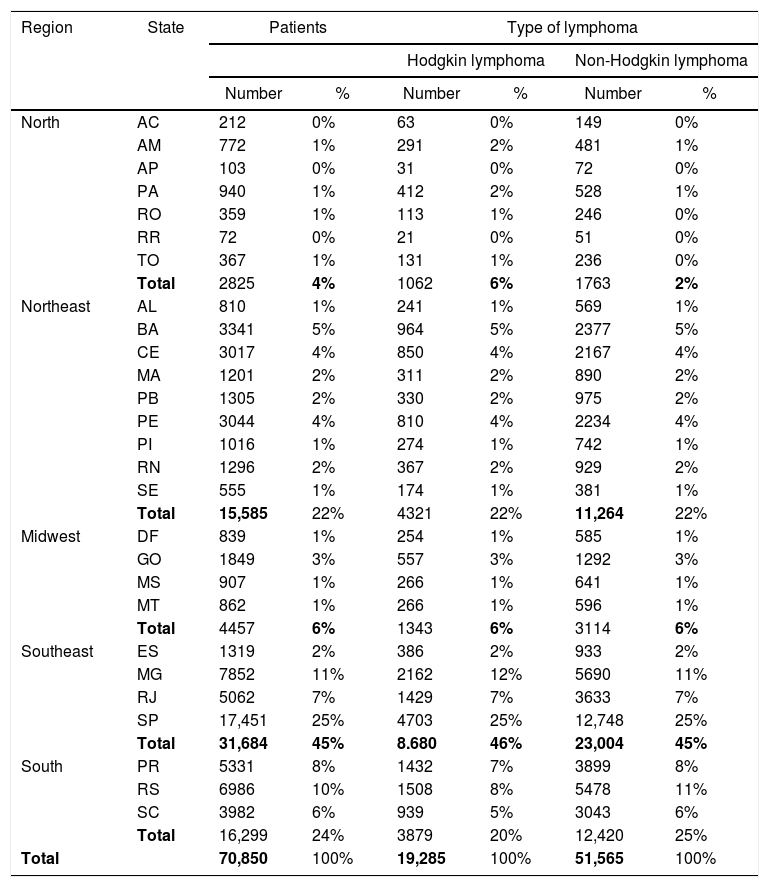
Most patients (39,975; 56%) received treatment outside their city of residence and 2058 (3%) outside their state of residence. São Paulo State accounted for 25% of the total patients, followed by Minas Gerais (11%) and Rio Grande do Sul (10%) (Table 4).
Numbers of patients diagnosed with lymphoma treated by the SUS from 2008 to 2017, according to the type of lymphoma, state of residence and geographic region.
| Region | State | Patients | Type of lymphoma | ||||
|---|---|---|---|---|---|---|---|
| Hodgkin lymphoma | Non-Hodgkin lymphoma | ||||||
| Number | % | Number | % | Number | % | ||
| North | AC | 212 | 0% | 63 | 0% | 149 | 0% |
| AM | 772 | 1% | 291 | 2% | 481 | 1% | |
| AP | 103 | 0% | 31 | 0% | 72 | 0% | |
| PA | 940 | 1% | 412 | 2% | 528 | 1% | |
| RO | 359 | 1% | 113 | 1% | 246 | 0% | |
| RR | 72 | 0% | 21 | 0% | 51 | 0% | |
| TO | 367 | 1% | 131 | 1% | 236 | 0% | |
| Total | 2825 | 4% | 1062 | 6% | 1763 | 2% | |
| Northeast | AL | 810 | 1% | 241 | 1% | 569 | 1% |
| BA | 3341 | 5% | 964 | 5% | 2377 | 5% | |
| CE | 3017 | 4% | 850 | 4% | 2167 | 4% | |
| MA | 1201 | 2% | 311 | 2% | 890 | 2% | |
| PB | 1305 | 2% | 330 | 2% | 975 | 2% | |
| PE | 3044 | 4% | 810 | 4% | 2234 | 4% | |
| PI | 1016 | 1% | 274 | 1% | 742 | 1% | |
| RN | 1296 | 2% | 367 | 2% | 929 | 2% | |
| SE | 555 | 1% | 174 | 1% | 381 | 1% | |
| Total | 15,585 | 22% | 4321 | 22% | 11,264 | 22% | |
| Midwest | DF | 839 | 1% | 254 | 1% | 585 | 1% |
| GO | 1849 | 3% | 557 | 3% | 1292 | 3% | |
| MS | 907 | 1% | 266 | 1% | 641 | 1% | |
| MT | 862 | 1% | 266 | 1% | 596 | 1% | |
| Total | 4457 | 6% | 1343 | 6% | 3114 | 6% | |
| Southeast | ES | 1319 | 2% | 386 | 2% | 933 | 2% |
| MG | 7852 | 11% | 2162 | 12% | 5690 | 11% | |
| RJ | 5062 | 7% | 1429 | 7% | 3633 | 7% | |
| SP | 17,451 | 25% | 4703 | 25% | 12,748 | 25% | |
| Total | 31,684 | 45% | 8.680 | 46% | 23,004 | 45% | |
| South | PR | 5331 | 8% | 1432 | 7% | 3899 | 8% |
| RS | 6986 | 10% | 1508 | 8% | 5478 | 11% | |
| SC | 3982 | 6% | 939 | 5% | 3043 | 6% | |
| Total | 16,299 | 24% | 3879 | 20% | 12,420 | 25% | |
| Total | 70,850 | 100% | 19,285 | 100% | 51,565 | 100% | |
Treatment initiation after diagnostic confirmation occurred within 30 days for 36,285 (51%) patients, between 30 and 60 days for 15,238 (22%) and after 60 days for 19,327 (27%).
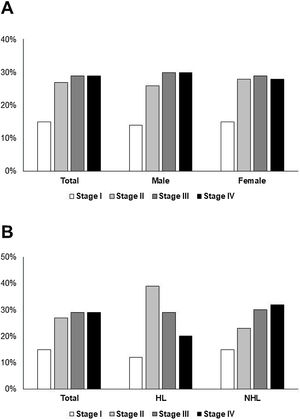
Considering all patients, for 15,976 (23%) patients, the staging records were incomplete or incorrect (recorded as stage 0). Therefore, 54,874 valid records were considered for staging analysis at diagnosis. Advanced disease (stages III and IV) was found in 58% of patients (60% male, 57% female; Figure 1A). More NHL patients were diagnosed with stages III and IV (62%) and 49% of HL patients were diagnosed in advanced stage (Figure 1B).
Association analysis considered only valid records. This analysis showed that gender was associated with the stage at diagnosis (X2 = 48,864, p < 0.001), with men presenting a higher proportion of advanced disease (stages III and IV), compared to that of women (with a higher proportion of stages I and II).
Lymphoma type was also associated with the stage at diagnosis (X2 = 1,696,764, p < 0.001). NHL patients had a higher proportion of diagnoses in stages III and IV, while those with HL had a higher proportion of diagnoses in stages I and II. Lymphoma type was also associated with the time to treatment initiation (X2 = 6,858, p < 0.05). NHL was associated with treatment initiation within 30 days, while HL was associated with treatment initiation within 30–60 days.
The lymphoma stage at diagnosis was associated with the time to treatment initiation (X2 = 128,499, p < 0.001). Patients with stages III and IV had a higher proportion of treatment initiation within 30 days, while those with stages I and II were associated with higher proportions of treatment initiation between 30 and 60 days and over 60 days.
From the SIM/SUS data, 45,601 deaths due to lymphoma were identified, with a median age of 63 years (0–111 years) and a higher predominance of mortality in male patients (55%). HL was the cause of death in 5266 (12%) patients and NHL was the cause of death in 40,335 (88%) patients (Table 1).
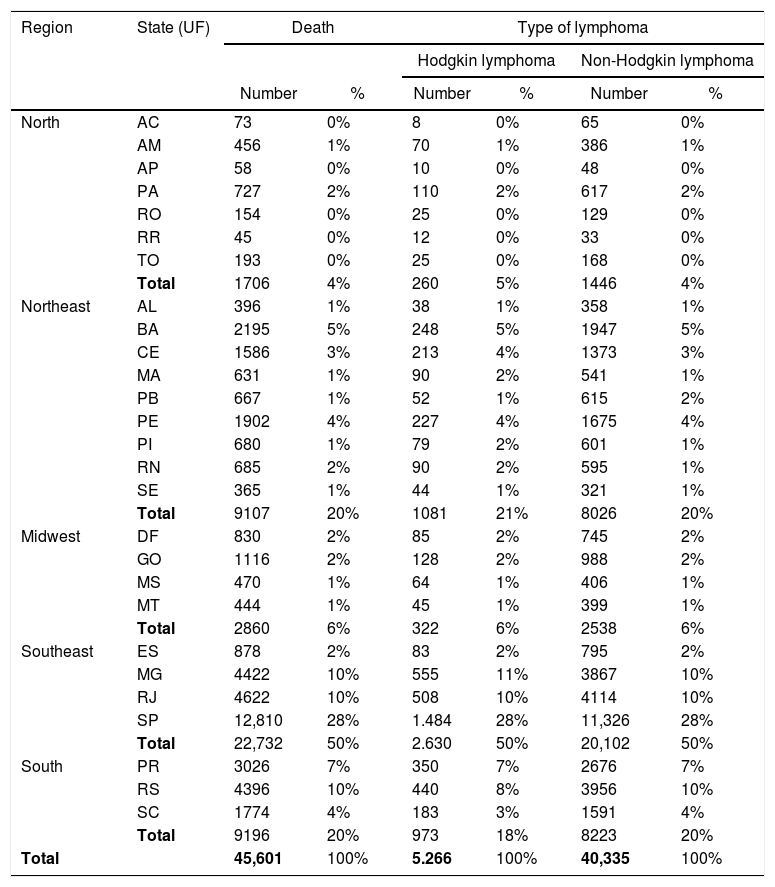
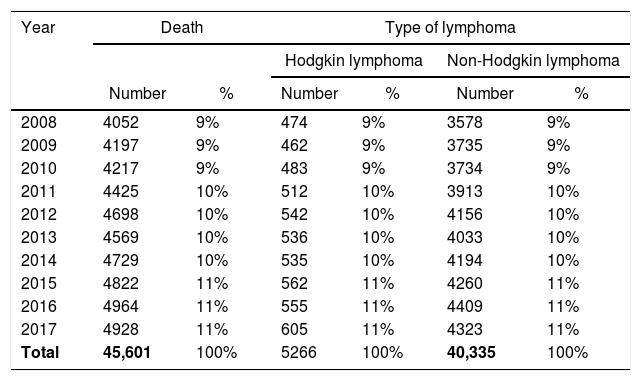
The state with the highest number of deaths was São Paulo (28%), followed by Minas Gerais, Rio Grande do Sul and Rio de Janeiro, each with 10% of the total deaths (Table 5). The number of lymphoma deaths increased from 4052 in 2008 (9% of total deaths) to 4928 in 2017 (11% of total deaths) (Table 6).
Absolute numbers and proportions of deaths from lymphoma in Brazil from 2008 to 2017, according to the type of lymphoma, state of residence and geographic region.
| Region | State (UF) | Death | Type of lymphoma | ||||
|---|---|---|---|---|---|---|---|
| Hodgkin lymphoma | Non-Hodgkin lymphoma | ||||||
| Number | % | Number | % | Number | % | ||
| North | AC | 73 | 0% | 8 | 0% | 65 | 0% |
| AM | 456 | 1% | 70 | 1% | 386 | 1% | |
| AP | 58 | 0% | 10 | 0% | 48 | 0% | |
| PA | 727 | 2% | 110 | 2% | 617 | 2% | |
| RO | 154 | 0% | 25 | 0% | 129 | 0% | |
| RR | 45 | 0% | 12 | 0% | 33 | 0% | |
| TO | 193 | 0% | 25 | 0% | 168 | 0% | |
| Total | 1706 | 4% | 260 | 5% | 1446 | 4% | |
| Northeast | AL | 396 | 1% | 38 | 1% | 358 | 1% |
| BA | 2195 | 5% | 248 | 5% | 1947 | 5% | |
| CE | 1586 | 3% | 213 | 4% | 1373 | 3% | |
| MA | 631 | 1% | 90 | 2% | 541 | 1% | |
| PB | 667 | 1% | 52 | 1% | 615 | 2% | |
| PE | 1902 | 4% | 227 | 4% | 1675 | 4% | |
| PI | 680 | 1% | 79 | 2% | 601 | 1% | |
| RN | 685 | 2% | 90 | 2% | 595 | 1% | |
| SE | 365 | 1% | 44 | 1% | 321 | 1% | |
| Total | 9107 | 20% | 1081 | 21% | 8026 | 20% | |
| Midwest | DF | 830 | 2% | 85 | 2% | 745 | 2% |
| GO | 1116 | 2% | 128 | 2% | 988 | 2% | |
| MS | 470 | 1% | 64 | 1% | 406 | 1% | |
| MT | 444 | 1% | 45 | 1% | 399 | 1% | |
| Total | 2860 | 6% | 322 | 6% | 2538 | 6% | |
| Southeast | ES | 878 | 2% | 83 | 2% | 795 | 2% |
| MG | 4422 | 10% | 555 | 11% | 3867 | 10% | |
| RJ | 4622 | 10% | 508 | 10% | 4114 | 10% | |
| SP | 12,810 | 28% | 1.484 | 28% | 11,326 | 28% | |
| Total | 22,732 | 50% | 2.630 | 50% | 20,102 | 50% | |
| South | PR | 3026 | 7% | 350 | 7% | 2676 | 7% |
| RS | 4396 | 10% | 440 | 8% | 3956 | 10% | |
| SC | 1774 | 4% | 183 | 3% | 1591 | 4% | |
| Total | 9196 | 20% | 973 | 18% | 8223 | 20% | |
| Total | 45,601 | 100% | 5.266 | 100% | 40,335 | 100% | |
Absolute numbers and proportions of deaths from lymphoma in Brazil from 2008 to 2017, according to the year of death and type of lymphoma.
| Year | Death | Type of lymphoma | ||||
|---|---|---|---|---|---|---|
| Hodgkin lymphoma | Non-Hodgkin lymphoma | |||||
| Number | % | Number | % | Number | % | |
| 2008 | 4052 | 9% | 474 | 9% | 3578 | 9% |
| 2009 | 4197 | 9% | 462 | 9% | 3735 | 9% |
| 2010 | 4217 | 9% | 483 | 9% | 3734 | 9% |
| 2011 | 4425 | 10% | 512 | 10% | 3913 | 10% |
| 2012 | 4698 | 10% | 542 | 10% | 4156 | 10% |
| 2013 | 4569 | 10% | 536 | 10% | 4033 | 10% |
| 2014 | 4729 | 10% | 535 | 10% | 4194 | 10% |
| 2015 | 4822 | 11% | 562 | 11% | 4260 | 11% |
| 2016 | 4964 | 11% | 555 | 11% | 4409 | 11% |
| 2017 | 4928 | 11% | 605 | 11% | 4323 | 11% |
| Total | 45,601 | 100% | 5266 | 100% | 40,335 | 100% |
Referring to the proportion of new cases, the Chi-square test showed differences in the proportions of deaths according to the lymphoma type (X2 = 5,524,050, p < 0.001). The proportion of deaths due to HL was lower than the proportion of new cases, while that of NHL was higher.
DiscussionThe proportions of NHL and HL patients treated in the Brazilian Public Unified Healthcare System (SUS) were different from those reported in the literature, in which 11% of lymphoma cases are expected to be HL.9 In Brazil, 27% of the cases were HL and 73% were NHL.
For lymphoma patients, the median age at diagnosis was 51 years, with 12% of the cases occurring in children under 19 years old. Data from the Global Cancer Incidence, Mortality and Prevalence (Globocan) in 2018 estimated that the incidence of lymphoma in patients of pediatric age was 6%.10 In turn, HL can be seen as a disease that is predominant among the youngest populations (25% in patients 0–19 years old and 41% in patients 20–34 years old), the median age at diagnosis being 28 years. The Globocan 2018 world data estimate that 17% of HL cases occur in the pediatric age group and 25% between 20–34 years of age;10 thus, we can conclude that HL affects a greater proportion of young patients in Brazil.
The Brazilian Ministry of Health has 317 registered services as Centers and Units of High Complexity Assistance in Oncology (CACON and UNACON).11 This structure allows most patients to receive treatment in the same state where they live. However, as expected, most treatments occur outside the city of residence because not all cities have registered services for cancer care. Almost ¼ of SUS lymphoma patients receive treatment in São Paulo State, where a large portion (22%) of the Brazilian population is located.
These data seem to be in line with the established oncology care policies, which define that regionalization of care must be performed according to the territorial limits of the states, establishing a specialized intrastate care network, according to the local demography.7
However, efforts are still needed to anticipate treatment initiation, since 49% of patients take more than 30 days to start treatment.
This trial confirms the hypothesis that lymphoma diagnosis is late under SUS, as 62% (NHL) and 49% (HL) of valid records were detected in stages III and IV, respectively. Data from high-income countries show that an early diagnosis of lymphoma is possible; the Surveillance, Epidemiology and End Results (SEER) data indicate that in the United States, from 2009 to 2015, 50% of NHL patients and 41% of HL were diagnosed late.12 Therefore, for Brazil, it would be acceptable to project a reduction target of approximately 10% of late diagnoses of lymphoma.
Robust evidence from the literature shows that late diagnosis is associated with worse prognosis and, consequently, higher mortality.5,13,14 Our results demonstrated that, from 2008 to 2017, the number of new lymphoma patients treated by the SUS remained stable each year. In the same period, there was an important increase in the crude mortality rate due to lymphomas, which may be an indicator of the system's failure to achieve curative treatment and/or to prolong survival. However, it should be noted that the death data provided by the SIM-SUS do not identify patients’ origin – SUS, private systems or others – although these data do not invalidate our inference about the failure of the system in recovering patients’ health.
In Brazil, lymphomas are responsible for 0.4% of total deaths and for 2.4% of cancer deaths, occupying position number 12 in the death ranking among all cancers (according to the SIM-SUS, 11,992,831 deaths were from all causes, 1,940,623 deaths, from all neoplasms and 45,601 deaths, from lymphomas).15 Overall, the median age of death was 63 years, with the vast majority due to NHL. São Paulo State accounted for 28% of total deaths, probably because this state treats the largest number of patients.
Considering that diagnosis was more frequent in men, with higher rates of disease in late stage and mortality, we reinforce the need for health promotion and cancer education campaigns aimed at the male public, whose worst indexes related to men's health have been debated in the literature. Since the 1990s, several studies have noted the different patterns of illness and mortality between men and women.16
The proportion of NHL deaths was higher than its proportion of cases (88% of deaths and 73% of cases). These findings are in line with the literature, which shows higher mortality from NHL.5,17 Nevertheless, our results show a higher proportion of NHL late diagnosis of NHL, which may also be related to its higher mortality. The median age of death in lymphoma patients was 63 years, that is, at an active age.18
The southeastern region of Brazil had a high number of lymphoma patients being treated by the SUS and a higher number of deaths, possibly due to its large population. In addition to demographics, socioeconomic factors and the structure of health services can also explain the differences between Brazilian states. A recent study showed that the human development index (HDI), income inequality (Gini’s index) and hospital bed rate per thousand habitants of the Brazilian states are associated with respective NHL morbimortality.19 In this study, Brazilian states with a higher HDI, lower Gini’s index and higher hospital bed rate per thousand inhabitants presented lower NHL mortality to incidence ratio (survival estimate).19
Since lymphomas can be curable if diagnosed early,5,20 it is important to determine the lethality rate of lymphoma (number of deaths in the period/prevalence in the period) in Brazil. Thus, the size of this healthcare problem can be scaled, allowing for the measurement of the urgency for prevention and control measures and monitoring of the effectiveness of the implemented actions over time. The currently available databases do not reflect this real-world evidence. Efforts must be made to improve cancer registries so that national indexes, such as lethality rate, survival rate and mortality rate, can be obtained to better target public health actions.
Healthcare managers should pay special attention to these findings and prioritize the adoption of measures to anticipate the diagnosis and initiation of treatment for lymphomas, as this is an important aspect for cancer control, in addition to the adoption of prevention measures. Although our results alone cannot support this statement, the increase in lymphoma mortality highlights the importance of the discussion and the need for a revision of cancer education and care policies in Brazil.
Despite the remarkable effort that has been made to strengthen public policies to fight cancer, the National Cancer Institute (INCA) highlights that there are still many challenges for the effective control of the disease. The INCA also notes that the greatest challenge for the development of the cancer surveillance system is to put into practice the use of information about the real situation in the country, so that the needs of the population are prioritized and covered by the public sector.4
As previously mentioned, the production of indicators, such as the lethality rate and survival/mortality rate, will be of great value as tools to outline strategies to improve the quality of the service offered.
However, the findings of this trial indicate that to change the history of lymphomas in Brazil, it is mandatory that prevention and detection strategies be strengthened, showing that immediate measures must be taken to (i) improve basic care delivery, allowing for the suspicion of lymphoma always to be considered, in a compatible clinical scenario, and; (ii) streamline the reception of specialized care, by which the patient must have his or her diagnosis confirmed and therapy initiated in the shortest possible time.
These findings may also provide relevant data for the formulation of the State Plan for Oncological Care and the National Curriculum Guidelines for the Medical Graduation Course to improve the care of lymphoma patients, promoting structural improvements in the healthcare system and to corroborate the anticipation of disease detection and treatment initiation.
In addition, this study provides a comprehensive overview about lymphoma diagnosis and mortality. Nevertheless, other complementary studies may be conducted based on these findings to investigate in depth the impact of socioeconomic factors and structure of health services on the lymphoma outcomes in different Brazilian states, as well as to determine whether there are additional costs for the system with the diagnostic panorama found; to measure the cost of early lymphoma deaths; to establish the correlation between the stage at diagnosis and the outcome achieved (death occurrence and length of stay in the system or cure), and; to expand this analysis to patients in the private system to identify possible inequalities and describe the differences found between the two health systems.
ConclusionThe situation of lymphoma diagnosis is a critical and serious problem for the Brazilian public healthcare system. In Brazil, a large proportion of lymphoma patients are diagnosed in late stage and, despite late stage at diagnosis being associated with an earlier treatment initiation, a significant proportion of patients start treatment belatedly. This scenario is especially serious for NHL and male patients and it is related to the higher mortality reported for these groups.
The results of present study highlight the importance of lymphoma prevention and early diagnosis strategies and provide relevant data to support strategic health care planning.
FundingThis work was supported by the Associação Brasileira de Linfoma e Leucemia (ABRALE). It did not receive any specific grants from funding agencies in the public, commercial or non-profit sectors.
Authors’ contributionsDenise Pires Martins was responsible for the conception and design of the study, analysis and interpretation of data, the drafting of the article, critical revision for important intellectual content and final approval of the version submitted.
Nelson Francisco Correa-Netto was responsible for the acquisition of data, analysis and interpretation of data, critical revision for important intellectual content and final approval of the version submitted.
Nina Melo was responsible for the interpretation of data, critical revision for important intellectual content and final approval of the version submitted.
Sandra Regina Loggetto was responsible for the drafting of the article, critical revision for important intellectual content and final approval of the version submitted.
Marcia Mello Costa De Liberal was responsible for the conception and design of the study, critical revision for important intellectual content and final approval of the version submitted.
Conflicts of interestThe authors declare no conflicts of interest.