Autologous hematopoietic stem cell transplantation (ASCT) is the long-term consolidation treatment for various hematological malignancies. The collection of hematopoietic stem cell yield is critical to successful ASCTs, but not always achieved due to hematopoietic stem cell mobilization failure (HSCMF). Details regarding the cell collection and outcomes of those who fail mobilization are still lacking. Therefore, this study aimed to yield data on clinical outcomes and cellular products after HSCMF.
MethodsRetrospective, unicentric study assessing clinical outcomes and characteristics of collected progenitor cells. The data were collected from patient databases. The results were reported in median, rates and percentages and absolute values. Patients older than 18 years of age at the time of mobilization and HSCMF were included.
ResultsFive hundred ninety-nine patients underwent mobilization protocols. Thirty-five (5.8%) of them failed in the mobilization and fourteen (40%) died. Median time to death was eight months. Disease progression and infection were responsible for all deaths. Median relapse-free survival was 6.5 months (20 patients, 57%). Seven (20%) survivors were receiving salvage therapy and five (14%) were being followed clinically. Six (20.6%) participants underwent collection by apheresis, with insufficient cell collection. The median quantity of peripheral CD34+ cells in those patients was 10.5/mm3. The median CD34+ quantity collected was 0.86 × 106 CD34+ cells/kg.
ConclusionsThe mobilization failure was associated with limited survival. Nonetheless, collected products offered perspectives for ex vivo expansion. Further studies should investigate the feasibility of expanding collected CD34+ cells to use as grafts for ASCT.
The autologous hematopoietic stem cell transplantation (ASCT) is currently the long-term consolidation treatment for various hematological malignancies.1 The collection of adequate hematopoietic stem cell yield is critical to a successful ASCT, but not always achieved due to the hematopoietic stem cell mobilization failure (HSCMF). Several risk factors have been associated with the HSCMF in patients preparing for the ASCT, such as the number of chemotherapy cycles before mobilization, increased interval between the granulocyte colony-stimulating factor (G-CSF) administration and peripheral blood stem cell collection, peripheral blood mononuclear cell count upon collection, thrombocytopenia before mobilization, low quantity of peripheral CD34+ cells prior to collection and previous mobilization failures.2 Despite the broad understanding of the factors involved in the process of the HSCMF and the available rescue measures to improve mobilization success rates (e.g., plerixafor),3 details regarding the cell collection and outcomes of patients who failed in the mobilization are still lacking.4
The previous data analyzing traditional, steady state mobilization protocols using single-agent G-CSF reported failure rates up to 38%. The plerixafor + G-CSF combination has been associated with improved cell yield, lower failure rate and resource utilization, when compared to the cyclophosphamide + G-CSF, cyclophosphamide alone and G-CSF alone. The preemptive addition of plerixafor to the mobilization protocol of patients with low peripheral blood CD34+ cells on pre-apheresis and/or with poor collection on the first day of apheresis improved mobilization failure rates (from as high as 22% to 2–3%); it was also associated with cost reduction5 and improved collection efficiency. Among remobilization protocols, the combination of plerixafor + G-CSF demonstrated superior performances, with failure rates consistently below 30%. Nevertheless, failure still occurs.6
The investigation of alternative methods to improve failure rates among poor mobilizers led to the discovery of novel molecules of interest. In recent studies, the UM171 and SR1 were found to promote in vitro expansion of human pluripotent stem cells. It has been demonstrated that culturing hematopoietic progenitors with the UM171 promotes the expansion of the CD34+ (68.97 ± 6.91%), CD34+ CD38− (44.10 ± 9.20%) and CD34+CD38−CD45RA−CD90+ LT-HSCs (3.05 ± 2.08%), cell populations that are phenotypically similar to those found in early progenitor cells. These results may aid researchers towards the development of protocols and techniques directed to patients who have failed in the mobilization. Of note, the SR1 experiments exhibit only discrete in vitro results, when compared to the UM171.7
Describing the outcome of these patients following the HSCMF is the first step towards a better understanding of this complex scenario, aiding multiprofessional teams to manage the complications associated with the care in this population. Therefore, this study yields data about clinical outcomes after the HSCMF and cellular products collected by apheresis in those patients.
MethodsWe performed a retrospective, unicentric, observational study that assessed overall survival and relapse-free survival following the HSCMF, clinical outcomes of survivors, median quantity of peripheral CD34+ before collection and median quantity of CD34+ collected in those who underwent at least one collection via apheresis, regardless of the total quantity of CD34+ collected. All participants were older than 18 years of age at the time of mobilization and the HSCMF had been documented in the center databases from January 2014 to July 2020. The informed consent for the mobilization was obtained from all patients and the study protocol was approved by the local ethics committee. The mobilization failure was defined as the inability to provide a peripheral stem cell collection greater than 2.0 × 106 CD34+ cells/kg. Patients who had successfully mobilized during the inclusion criteria period and collected adequate peripheral CD34+ were excluded, regardless of previous failures.
The digital and physical data were collected from Hospital das Clínicas da FMUSP patient database and medical records. The study data were collected and managed using REDCap electronic data capture tools hosted at our institution.89 The sensitive information and personal data were kept anonymous to preserve the confidentiality of the participants. The results were reported in median, rates and percentages and absolute values. The measures of association between characteristics and outcomes were not reported due to the small number of patients.
ResultsFive hundred and ninety-nine patients underwent at least one mobilization protocol during the preparation for the ASCT at our service from January 2014 to July 2020. Thirty-five (5.8%) of them failed in the mobilization of peripheral stem cells. The median age in this group was 53 years old (youngest was 28, oldest 70). Twenty-three (65.7%) were males and twelve (34.2%) were females. Baseline oncologic diseases in the studied population included: non-Hodgkin lymphoma (12), multiple myeloma (11), germ cell tumor (5), acute myeloid leukemia (1) and Hodgkin lymphoma (6). The following risk factors for mobilization failure previously described and present in our cohort were: advanced stage of baseline disease (63%), age > 60 years old (34%), thrombocytopenia (27%), history of radiotherapy (17%) and ≥ 3 lines of treatment (24%).
Fourteen (40%) patients who failed in the mobilization died during the study period. The median time to death was eight months, varying from one to thirty months. The disease progression was responsible for ten deaths and infection (regardless of the nature) was responsible for four deaths. Twenty (57%) patients had relapsed, with a median relapse-free survival of 6.5 months (1–29 mo.), from the first day of mobilization to the date of laboratorial/radiologic confirmation of relapse. When more than one mobilization protocol was used, the date of the first mobilization attempt was considered. Seven (33.3%) patients among the twenty-one survivors who failed in the mobilization were receiving salvage therapy and five (23.8%) were being followed clinically. The median follow-up time was 24 months.
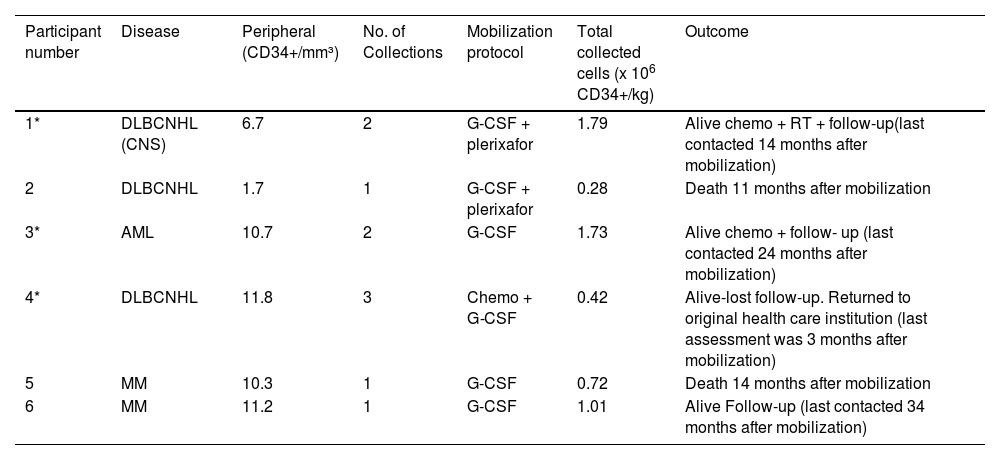
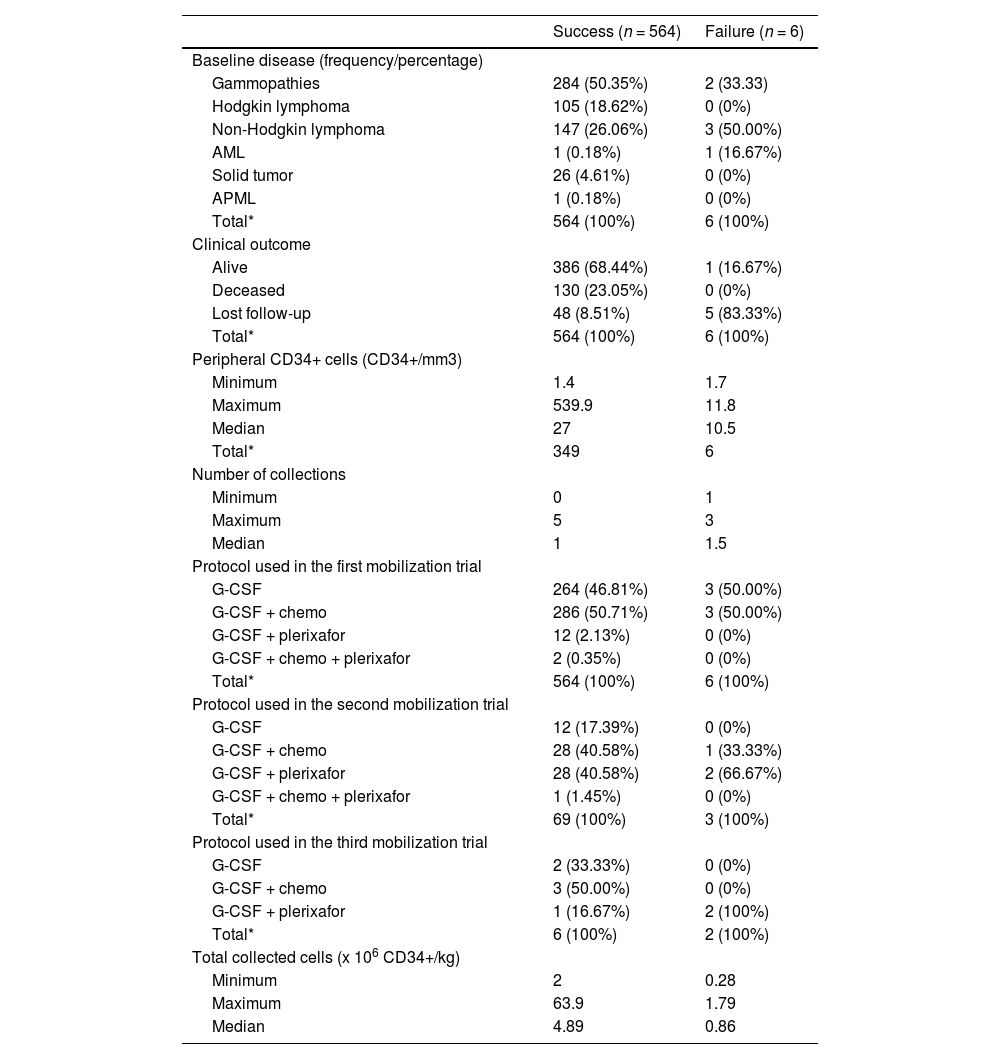
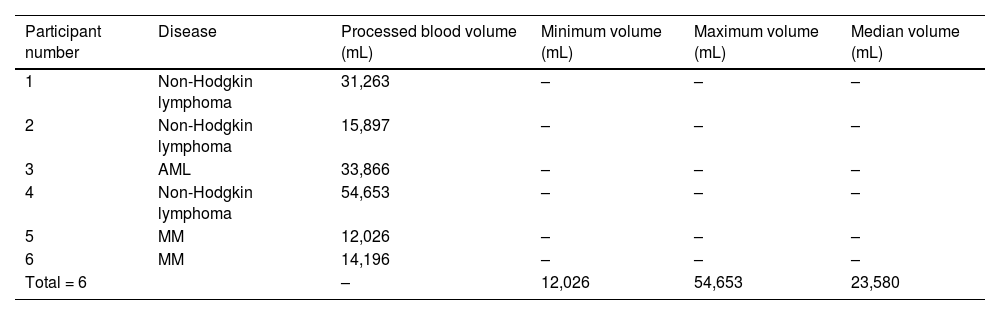
Six (17.1%) participants underwent peripheral stem cell collection by apheresis, with insufficient cell collection. The clinical and laboratorial information regarding these patients is available in Table 1. The median quantity of peripheral CD34+ cells in those patients was 10.5/mm3 and 1.7/mm3, in patients who did not undergo apheresis. Among those who underwent collection (six participants), the median quantity of CD34+ collected was 0.86 × 106 CD34+ cells/kg. Two of them had used plerixafor. One had received chemotherapy as part of the mobilization protocol (Table 1). A comparison between the group that failed in the mobilization, but underwent collection and the group that successfully mobilized and collected CD34+ cells can be found in Table 2 and information regarding processed blood volume in those six participants who failed in the mobilization, but underwent collection, is available in Table 3.
Characteristics of patients and collected cells in patients who failed in the CD34+ cell mobilization.
MM = multiple myeloma; DLBCNHL = diffuse large B cell non-Hodgkin lymphoma; CNS = central nervous system; AML = acute myeloid leukemia; chemo = chemotherapy; RT = radiotherapy; *patients who had ≥ 2 collections.
Clinical and hematological characteristics of the studied population.
| Success (n = 564) | Failure (n = 6) | |
|---|---|---|
| Baseline disease (frequency/percentage) | ||
| Gammopathies | 284 (50.35%) | 2 (33.33) |
| Hodgkin lymphoma | 105 (18.62%) | 0 (0%) |
| Non-Hodgkin lymphoma | 147 (26.06%) | 3 (50.00%) |
| AML | 1 (0.18%) | 1 (16.67%) |
| Solid tumor | 26 (4.61%) | 0 (0%) |
| APML | 1 (0.18%) | 0 (0%) |
| Total* | 564 (100%) | 6 (100%) |
| Clinical outcome | ||
| Alive | 386 (68.44%) | 1 (16.67%) |
| Deceased | 130 (23.05%) | 0 (0%) |
| Lost follow-up | 48 (8.51%) | 5 (83.33%) |
| Total* | 564 (100%) | 6 (100%) |
| Peripheral CD34+ cells (CD34+/mm3) | ||
| Minimum | 1.4 | 1.7 |
| Maximum | 539.9 | 11.8 |
| Median | 27 | 10.5 |
| Total* | 349 | 6 |
| Number of collections | ||
| Minimum | 0 | 1 |
| Maximum | 5 | 3 |
| Median | 1 | 1.5 |
| Protocol used in the first mobilization trial | ||
| G-CSF | 264 (46.81%) | 3 (50.00%) |
| G-CSF + chemo | 286 (50.71%) | 3 (50.00%) |
| G-CSF + plerixafor | 12 (2.13%) | 0 (0%) |
| G-CSF + chemo + plerixafor | 2 (0.35%) | 0 (0%) |
| Total* | 564 (100%) | 6 (100%) |
| Protocol used in the second mobilization trial | ||
| G-CSF | 12 (17.39%) | 0 (0%) |
| G-CSF + chemo | 28 (40.58%) | 1 (33.33%) |
| G-CSF + plerixafor | 28 (40.58%) | 2 (66.67%) |
| G-CSF + chemo + plerixafor | 1 (1.45%) | 0 (0%) |
| Total* | 69 (100%) | 3 (100%) |
| Protocol used in the third mobilization trial | ||
| G-CSF | 2 (33.33%) | 0 (0%) |
| G-CSF + chemo | 3 (50.00%) | 0 (0%) |
| G-CSF + plerixafor | 1 (16.67%) | 2 (100%) |
| Total* | 6 (100%) | 2 (100%) |
| Total collected cells (x 106 CD34+/kg) | ||
| Minimum | 2 | 0.28 |
| Maximum | 63.9 | 1.79 |
| Median | 4.89 | 0.86 |
Missing data were independently excluded from the report of each variable of interest, accounting for different values in the total number of observations reported for a given group. Patients who have not been subjected to collection were not reported in this table.
Success = patients who successfully mobilized CD34+ cells; Failure = patients who failed to mobilize CD34+ cells, but underwent collection. G-CSF = granulocyte-colony stimulating factor; chemo = chemotherapy.
Processed blood volume among patients who failed in the mobilization of CD34+ cells.
Our results reinforce the hypothesis that patients who failed in the mobilization of peripheral CD34+ cells during the ASCT may experience limited overall survival rates and relapse-free survival. As expected, most of them had at least one risk factor for mobilization failure and almost half of them (40%) had died by the end of the data collection. Nonetheless, the results obtained from analysis of the material collected via apheresis offer some perspective of future advances. The recent data involving the expansion of peripheral blood CD34+ cells using the UM171 suggested the ex vivo expansion as a feasible alternative for achieving adequate numbers of CD34+ cells in patients who failed in the mobilization.10 Currently, most studies using the UM171 have explored its effectiveness in expanding cord blood-derived CD34+ cells11 and its use in peripheral blood-derived CD34+ cells may also be a reasonable alternative for patients who underwent the HSC apheresis collection with an insufficient quantity of CD34+ yield to perform the ASCT. For instance, six participants from our study were able to collect minor amounts of peripheral CD34+, with a median of 0.86 × 106 CD34+ cells/kg, representing 17.1% of those who failed in the mobilization. It is still unclear what amount of collected peripheral CD34+ cells should be sufficient for the ex vivo expansion and further studies should be performed to answer this and other feasibility questions.
ConclusionTherefore, we strongly believe that there is a broad perspective of improving our ability to expand the HPSCs in patients with similar conditions and provide an adequate consolidation therapy for patients with the ASCT indication.