The knowledge of clinicians regarding blood transfusion services may impact patient care and transfusion outcome. The wide variation in transfusion practices among clinicians leads to inappropriate blood product usage and jeopardizes patient safety. Hence, this survey study aimed to assess knowledge, attitude and practice among the residents and interns of safe blood transfusion.
MethodsThe online survey was based on self-administered questionnaires of three sections: 1. Demography; 2. Knowledge, and; 3. Attitude and Practice. One point was assigned for the correct response of each question in every section. The knowledge score was further categorized into three categories, depending on the points obtained. The participants were also divided into four groups, depending on their experience. The Kruskal-Wallis test was applied to determine the difference of knowledge and practice scores in three designated groups of residents and interns. A p-value of less than 0.05 was considered to be significant.
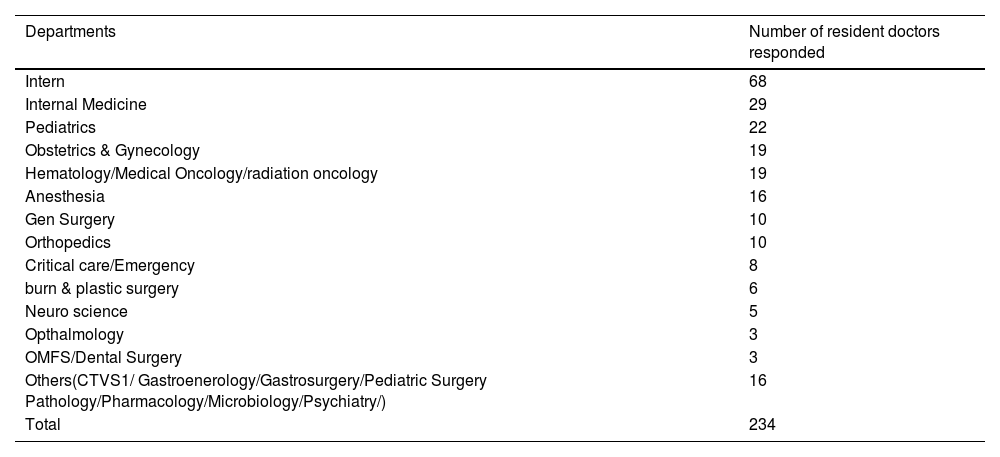
ResultA total of 247 residents and interns participated in this study. Thirteen participants had an incomplete response. Out of 234 participants, Senior Residents (SR), Junior Residents (JR), and interns were 70, 96 and 68 participants, respectively. The knowledge scores of interns were significantly low, as compared to SRs and JRs. Practice scores of interns were also significantly low, compared to the JRs. However, most of the residents and interns (85%) were aware of the pre-transfusion testing.
ConclusionTherefore, the mandatory incorporation of the transfusion medicine subject in the undergraduate curriculum can help the young budding doctors to better implement the patient blood management.
Transfusion of blood and blood components is an emergency tool in the management of acute life-saving conditions. The transfusion chain comprises complex activities, from the donor's vein to the patient's vein, involving various medical and paramedical staff.1 Hence, there is always an impending threat of transfusion error. The post-graduate course in transfusion medicine has been commenced and recognized by the Medical Council of India to improve transfusion services. Clinicians' knowledge about blood products and their preparation, storage, demands, doses and administration may profoundly impact patient care and transfusion outcomes. Wide variation in transfusion practices and inappropriate transfusion may jeopardize their safety.2 The intent of establishing transfusion medicine (TM) will go in vain if the same is not executed at the bedside by our clinician colleagues.3 Inappropriate utilization of blood components adds unnecessary costs and transfusion reactions. Optimal utilization of blood is vital to minimize alloimmunization and the spread of transfusion-transmitted infections.4 Physicians and surgeons make the majority of transfusion decisions without formal training in TM. The clinician transfusion practices are based on their individual experiences and they are mostly unaware of the error in the transfusion chain.5,6 Resident doctors from clinical specialties have an active role in blood transfusion. The best transfusion is the transfusion of the right component to the right patient at the right dose at the right time. Therefore, the same is expected from the residents and interns. But they are provided with minimal education and practical exposure, as TM is not a part of the undergraduate curriculum.7,8 Only one previous study in India and some foreign literature described inadequate TM knowledge and awareness amongst resident doctors.9-11 Hence, we planned to conduct a knowledge, attitude and practice (KAP) survey among the residents and interns about safe blood transfusion to ascertain the knowledge gap and design the educational materials.
MethodsStudy subjectsAll resident doctors, such as senior residents, i.e., SR (Post-MD degree residency)/ junior residents, i.e., JR (Post-M.B.B.S Residency) and interns of our institution, were surveyed using self-administered questionnaires in this descriptive cross-sectional study from February 2019 to December 2020. Active participation of residents of most specialties with high blood utilization rates, such as trauma & emergency, neurosurgery, orthopedics, surgery, obstetrics and gynecology, pediatrics, anesthesia and medicine was encouraged. Participation in the study was voluntary and confidentiality was assured.
MaterialsThe survey consisted of three sections: 1. Demography; 2. Knowledge, and; 3. Attitude and Practice. The demography section included the designation (senior resident/junior resident/intern), department and years of experience after undergraduate studies. There are 15 and 19 questions in the knowledge section and attitude/practice sections, respectively. Knowledge-based questionnaires are related to blood grouping and crossmatching (5), component therapy and storage (6), modification of component (2), transfusion-transmitted infection and reaction (2). Their attitude was also evaluated for using blood components, blood transfusion sets, pre-medication and consent before transfusion. There were 14 practice-based questions, including the related transfusion request (4), component therapy (5), pre-transfusion checks (2), blood warmer (2) and transfusion reaction (1). All the questionnaires were the closed type to avoid the problems related to scoring the open-ended responses. One option, “don't know,” was also included to prevent guessing. All the questionnaires were developed by TM specialists and reviewed by faculties of other departments. A pilot test of questionnaires was performed among a random sample of residents and interns to assess the clarity of the questions.
MethodA Google form consisting of these three sections was developed and sent to all residents and interns through standard google group mail and social media, such as WhatsApp. Three times, every four weeks, a reminder message to participants was sent along with a “thank you for participation” statement. The years of experience was categorized into four different groups: category 1: 1 year of experience in blood transfusion; category 2: 2 - 3 years; category 3: 4 - 5 years, and; category 4: more than five years. The correct response of each knowledge-based and practice/attitude-based question was assigned with one point and separate scores were calculated for the knowledge and practice/attitude-based questions as knowledge scores (KS) and practice scores (PS), respectively. The KS again was divided into three categories, as ≤ 7 (out of 15 i.e., below 50%) as poor (KC3); 8 - 11 as average (KC2), and; > 11 as good (KC1). Those who had not even completed the knowledge-based questions were excluded from the study.
Statistical analysisThe individual response was entered in Excel and analyzed by the R version 4.1.0 (2021-05-18) – “Camp Pontanezen.” The Shapiro-Wilk test checked the normalcy of the data and the non-normal data was depicted by the median and interquartile range. The Chi-square test was used to establish the association of knowledge among resident doctors and interns by comparing knowledge and experience categories with the designation groups. The Kruskal-Wallis test was applied to determine the difference of knowledge and practice scores in the three designated groups of residents and interns. The Dunn test investigated the post hoc analysis of multiple comparisons between possible pairs of designations and experiences and the Benjamini-Hochberg (BH) correction was used to adjust the p-value for multiple comparisons. The institutional ethical committee approved the study with registration no. ECR/534/Inst/OD/2014/RR-17.
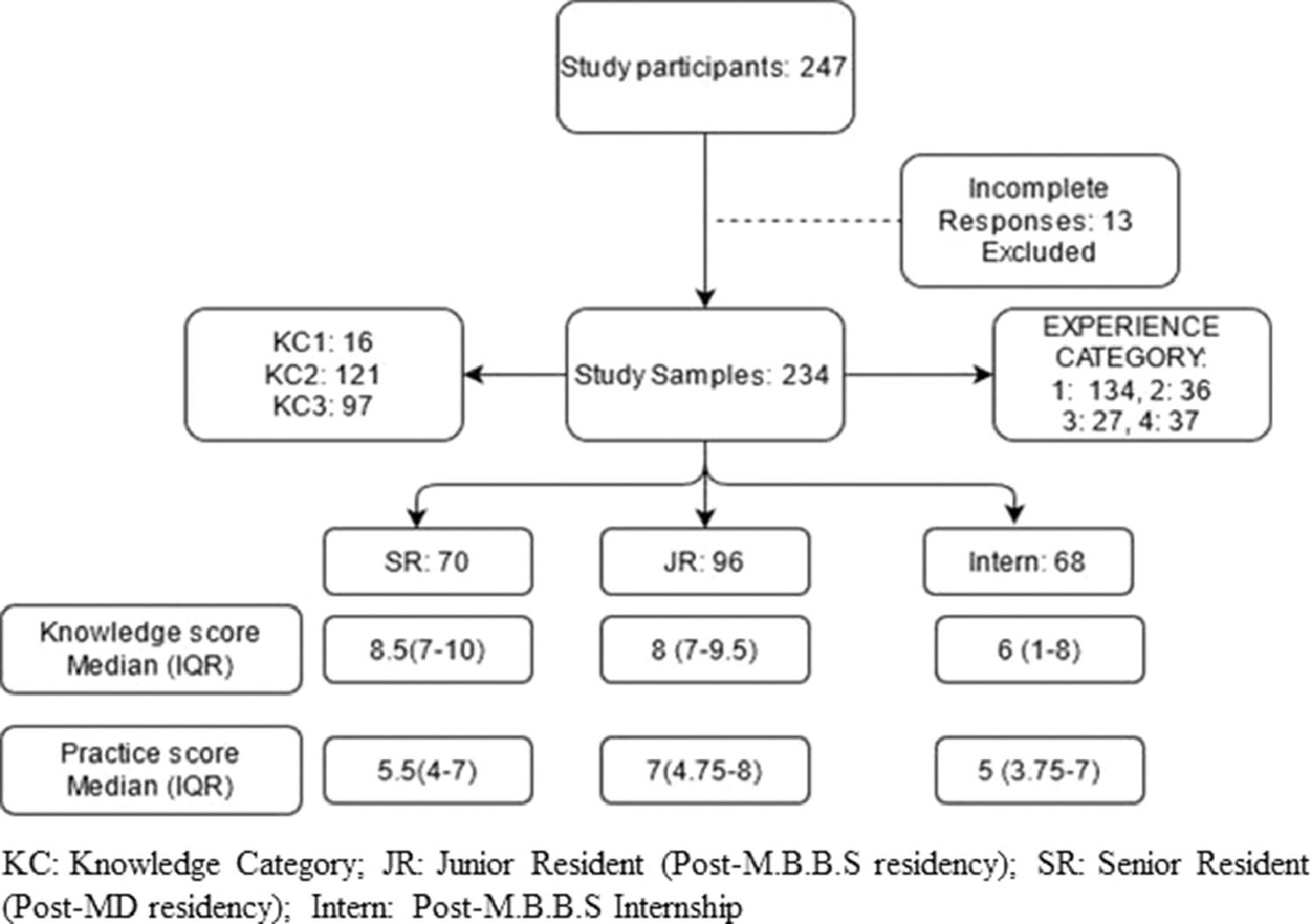
ResultA total of 247 residents and interns participated in this study. Thirteen participants were excluded because of incomplete responses. Out of 234 participants, SR, JR and interns were 70, 96 and 68 participants, respectively. The participant characteristics, median KS and PS, along with the interquartile range, are depicted in Figure 1.
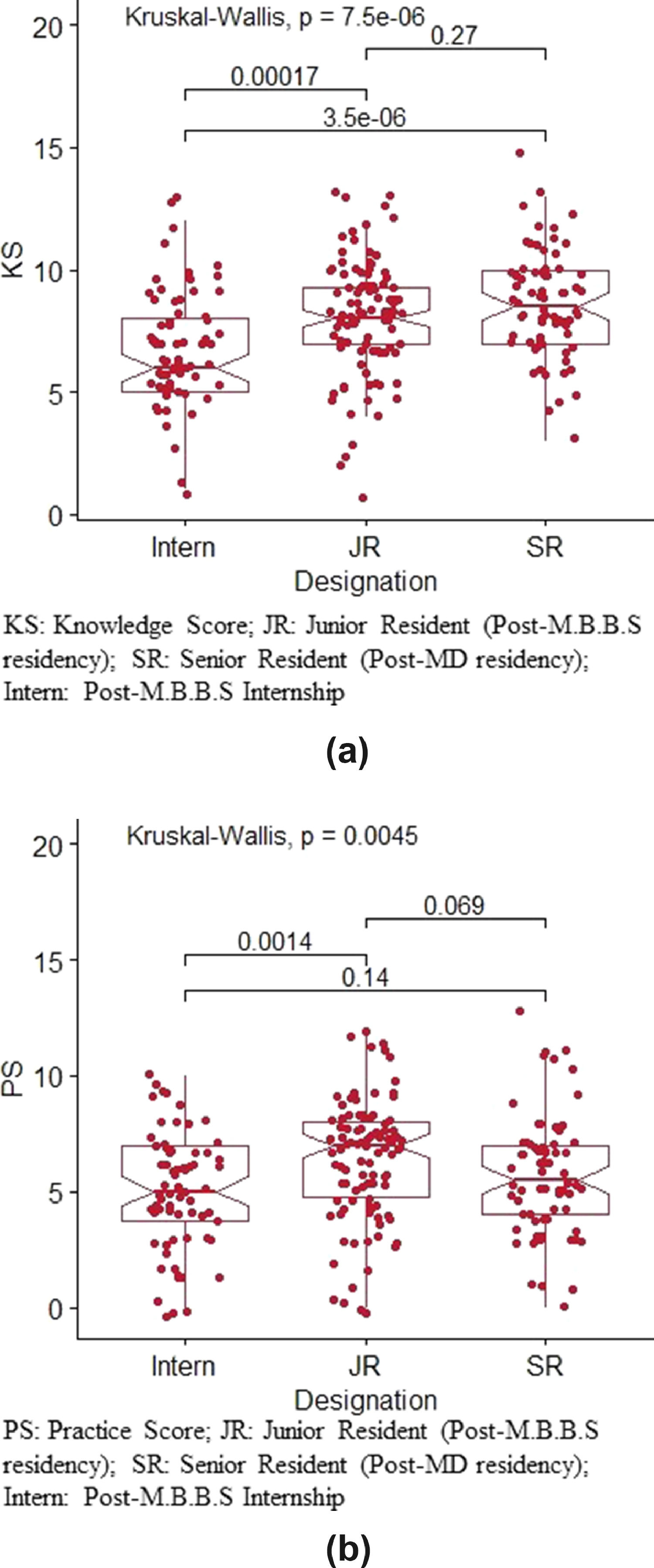
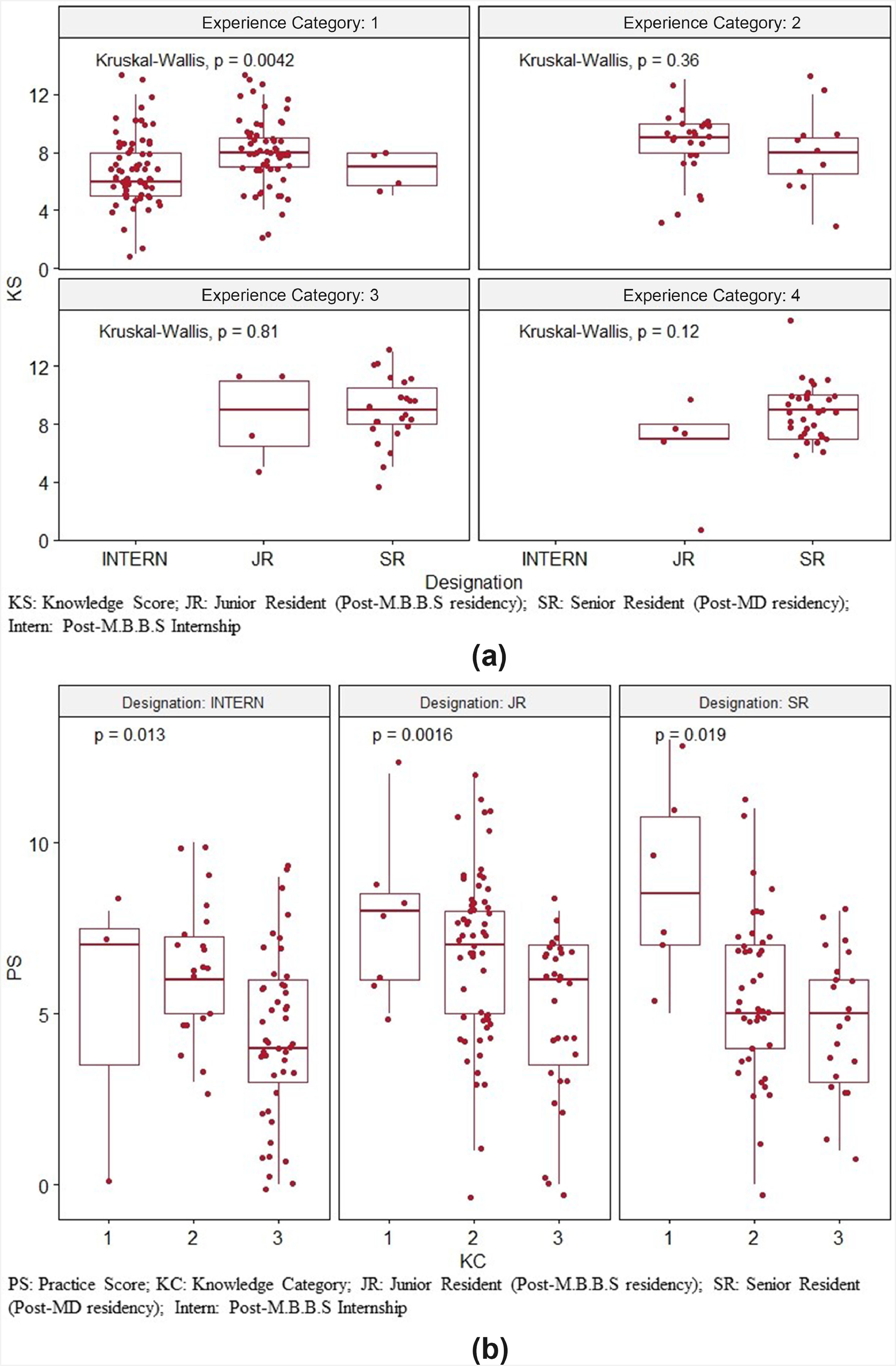
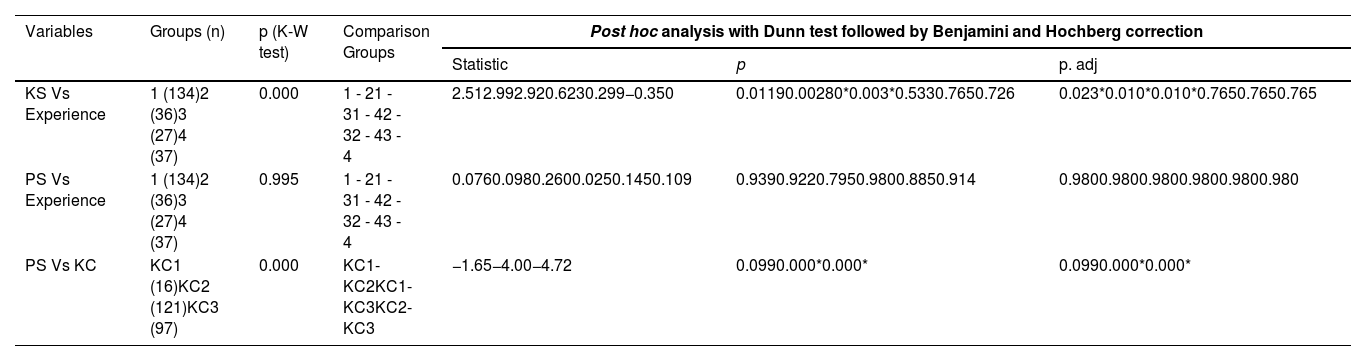
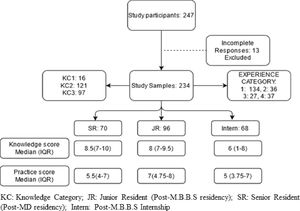
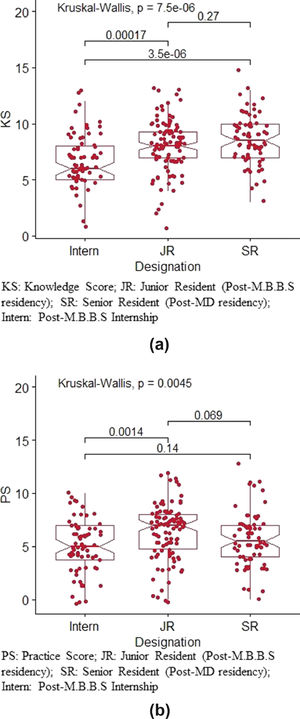
The median KS was highest among the SR and lowest among interns. The categorization of the KS showed only 16 participants (6.8%) had good knowledge (KC1). The Kruskal-Wallis test detected a significant difference in knowledge and practice scores among designation groups. The KS of JR and SR were significantly increased, as compared to interns. (Figure 2a) However, the difference in PS was significant only between JR and interns, with better scores among JRs than interns, as shown in Figure 2b. Furthermore, the post hoc analysis using the Dunn test showed a significant difference in the KS of SR and JR with Interns. However, the difference in the PS was significant only between the JR and interns and not between the SR vs. JR or the SR vs. interns. The multiple pairwise comparisons of the KS among experience categories using the Dunn test and BH correction found a significant difference only between the experience category 1 versus the rest with better KS among the JR and SR, compared to the interns in the experience category 1. [Table 1 and Figure 3a] However, no difference was noted in pairwise comparisons of PS among experience categories. (Table 1) Among knowledge categories, the PS were significantly different in KC1-KC3 and KC2-KC3 pairs. (Table 1) Moreover, the comparison of PS among three KC groups separately in all designation groups was significant with better PS in the good knowledge category in all three designations, as shown in Figure 3b. The proportionate distribution of knowledge, attitude and practice-based responses is described below under separate headings (Table 2).
Showing pairwise multi-comparison of knowledge and practice score among designation, experience and knowledge category.
| Variables | Groups (n) | p (K-W test) | Comparison Groups | Post hoc analysis with Dunn test followed by Benjamini and Hochberg correction | ||
|---|---|---|---|---|---|---|
| Statistic | p | p. adj | ||||
| KS Vs Experience | 1 (134)2 (36)3 (27)4 (37) | 0.000 | 1 - 21 - 31 - 42 - 32 - 43 - 4 | 2.512.992.920.6230.299−0.350 | 0.01190.00280*0.003*0.5330.7650.726 | 0.023*0.010*0.010*0.7650.7650.765 |
| PS Vs Experience | 1 (134)2 (36)3 (27)4 (37) | 0.995 | 1 - 21 - 31 - 42 - 32 - 43 - 4 | 0.0760.0980.2600.0250.1450.109 | 0.9390.9220.7950.9800.8850.914 | 0.9800.9800.9800.9800.9800.980 |
| PS Vs KC | KC1 (16)KC2 (121)KC3 (97) | 0.000 | KC1-KC2KC1-KC3KC2-KC3 | −1.65−4.00−4.72 | 0.0990.000*0.000* | 0.0990.000*0.000* |
KS: Knowledge score, PS: Practice score, KC: Knowledge Category, K-W test: Kruskal-Wallis test.
Participants (JRs and SRs) from various departments.
JR: Junior Resident (Post-M.B.B.S residency); SR: Senior Resident (Post-MD residency).
The correct responses to knowledge-based questionnaires were documented. Most of the residents and interns (85%) knew that the blood unit is issued after the transfusion transmissible infections (TTI) testing, grouping and cross-matching. Among them, 72.6% had correctly responded about the five mandatory TTI tests (HIV, HBV, HCV, Malaria and syphilis). In emergency life-saving situations, a blood unit is issued after an immediate spin cross-match. This fact is known to 66.6% of our doctors. Only 53.4% of the participants knew that simultaneous infusion of fluid (such as dextrose/ringer lactate) other than normal saline through the same intravenous access is not compatible with packed red blood cells (PRBCs). Leukofiltration and irradiation prevent the febrile non-hemolytic transfusion reaction (FNHTR) and graft vs. host disease (GVHD), respectively, which was correctly responded by only 48.7% of the participants. The appropriate storage temperature and shelf-life of blood components were responded by 59.8% and 57.2% of the total participants, respectively. Most of the participants (85%) knew about the Bombay blood group having the anti-H in the serum and no other next compatible PRBC exists for the Bombay blood group patients.
AttitudeAn attitude of the resident doctors and interns towards taking consent, using the blood transfusion (BT) set primed for transfusion of components, blood component therapy and pre-medication, was assessed. Only 69.6% of the participants were aware of the informed consent before blood transfusion and only 45.3% utilized the BT set for random donor platelets (RDP) or fresh frozen plasma (FFP) transfusion. Almost half of the resident doctors (51.7%) prefer whole blood transfusion for bleeding patients and only 30% are aware of the use of blood components. A total of 67.95% of the participants do not give pre-medication. Only 27.7% of residents and interns think that they need training and 53.1% of the participants believe that they have acquired the basic transfusion knowledge from their seniors/teachers.
PracticeThe median PS of the participant doctors was 6 out of 14. A total of 69.2% of the participant sent a properly filled out requisition with the properly labeled EDTA and clotted vial. But on the platelet requisition, 25.2% of doctors still write 'grouping and cross-matching' to be done, though we do not routinely employ platelet cross-matching. Only 36.7% of the doctors were aware of initiating the PRBC transfusion as soon as possible after receiving the unit. Still, 52.9% of the participants had the misbelief of warming or keeping at room temperature for one hour. To warm the blood unit, only 25.2% of participants had the idea of using a blood warmer. Only 27.7% and 36.3% of the participants had the good practice of immediately returning the RDP and FFP, respectively, to the blood bank, if not utilized for any circumstances. Around 41% of the participants do not know that cryoprecipitate can be transfused across the ABO blood group. Only approximately half of the participants (46.6%) had the good practice of informing the blood bank about the transfusion reaction after stopping the transfusion and giving the medication as needed.
DiscussionThis KAP study found a statistically significant difference in patient safety knowledge related to blood transfusion among the designated groups between residents and interns. Both senior, as well as junior residents, had better knowledge scores than interns. This knowledge level was also reflected in their practice score and the comparison of the practice score with three knowledge categories was significant among SR, JR and interns, as shown in Figure 3b. However, the PS was not significantly different between JR, SR and interns, when compared with their experience categories. In general, interns and JR were following the instruction given by their SR; thus, despite the significant variation in their KS, the PS was not different. One more reason could be the low sample size of the JR and SR in the 2, 3 and 4 experience categories and the statistical analysis may not be true in such a situation. The attenuation of knowledge, which reflects their practice score in subsequent years among the SR, compared to the JR, may be another possibility of not getting a significant difference and this reason was highlighted by previous studies.3,6,9
Residents and interns are the backbones of hospital services. They are actively involved in ordering blood components, transfusing them at the bedside and managing any untoward events due to transfusion. The lack of knowledge among them endangers patient safety. As per the SHOT report, 2020, approximately 30.7% of incorrect blood component transfusion errors occur at blood ordering.12 Most of the survey focused on the attitudes and bedside transfusion practices limited to post-analytical activities of the nurses and clinicians. We conducted this study analyzing knowledge levels among different categories of residents and interns involved in blood transfusion services and their actual bedside practices. Our single-center study highlighted an existing knowledge gap among the residents.
As detailed in the results, interns have alarmingly poor knowledge about various aspects of blood transfusion services. A total of 41.5% of the residents had poor knowledge, which is similar to some other studies.9,13 This could be explained by the fact that there are significantly fewer, only three-hour educational sessions on transfusion medicine during the entire undergraduate Bachelor of Medicine, Bachelor of Surgery (MBBS) course.8,9 As per the national blood policy, transfusion medicine must be integrated into undergraduate courses to encourage appropriate clinical use of blood and blood components.14 With increased years of experience, the JR and SR have more knowledge, but there is no statistically significant difference. Haspel RL et al. found that the third and fourth year postgraduates had statistically higher scores than those in their first year, but the difference was less than 7% [9].
The purpose of pretransfusion compatibility testing is to prevent an incompatible red blood cell transfusion, leading to a hemolytic transfusion reaction. Immediate spin (IS) cross-matching is performed to avoid an ABO-mismatch. Antihuman globulin (AHG) cross-matching detects antibodies against minor blood group antigens, thus, preventing a delayed hemolytic transfusion reaction.15 The AHG (Coomb's phase) cross-matching requires a longer time. The clinician and transfusion medicine consultant's decision to omit the AHG cross-matching depends on the urgency of the situations. The compatibility form provided along with the blood unit details the type of cross-matching performed. Thus, the resident doctors should know about adequately filling out the blood requisition, mentioning the name, registration number, bed number, ward and the urgency or elective transfusion schedule. They also should check the compatibility form before administration of the PRBC to avoid the most common transfusion error and chaotic situation. The blood component modification, such as leukoreduction, irradiation, washing to prevent transfusion reactions, i.e., FNHTR, GVHD, allergy, respectively, should be mentioned in the requisition as per the patient need.16 Here in our study, more than half of the participants were not aware of the above facts. Most residents knew about the type of component prepared in the blood bank from the whole blood unit and its storage temperature and shelf-life. Nevertheless, there was little knowledge on single-donor apheresis platelets, which are ordered frequently.
The TTI testing before the release of blood components and informed written consent before transfusion are obligatory in India. Most of the participants (69.6%) had the perception of taking consent before transfusion and approximately 63.6% had the good practice of taking vitals before, during and after transfusion. In contrast, many studies in the literature found poor documentation of informed consent and vitals and improper patient identification as the major drawbacks in bedside transfusion practice.17,18 The use of a blood warmer is indicated for exchange transfusion in neonates, massive transfusion and rapid transfusion procedures. Improper warming methods may contribute to hemolysis and bacterial infections.17,19 The bedside transfusion checks prior to blood component administration are the final crucial step in the prevention of untoward events. Transfusion practices at the bedside help to generate information to establish evidence-based transfusion guidelines.20-23 Adequate knowledge and timely recognition of possible transfusion-related complications at the bedside help to ensure the best patient outcomes. However, our study reflected poor practice among the interns, as compared to the JR and SR. These findings could be due to poor knowledge of transfusion medicine and lesser educational or training session exposure. There was a significant difference in transfusion practice between different knowledge categories. Most of them acquire the knowledge from their seniors and have not been familiarized with the actual procedure and guidelines. Our residents and interns also favored continuous induction training to enhance their knowledge and good bedside transfusion practice.
The previous literature has focused on the transfusion practice of nurses and many of the studies included very few doctors. The strength of the study is that this study reflects the knowledge level and practice pattern of blood transfusion focusing on patient safety, mainly among resident doctors and interns. Most of the residents involved in bedside transfusion practices have participated in this study. However, it is a single-center study and a questionnaire-based KAP study. Hence, the real-time auditing of bedside practices was not performed.
ConclusionIn conclusion, the transfusion practices depend on the knowledge of the residents. Adequate knowledge of various aspects of transfusion medicine is a necessity for a successful patient blood management system. The introduction of the transfusion medicine course in the undergraduate curriculum can aid the young budding doctors in implementing the patient blood management system early and in an effective way in their practices. Undergraduate students and interns should understand the importance of blood transfusion in patient safety and transfusion medicine needs to be integrated into their study curriculum. Induction and continuous training sessions at regular intervals of all residents and staff, emphasizing the evidence-based transfusion approach, pre-transfusion checks, bedside blood administration practices, recognition and management of transfusion reactions, will help optimize patient safety.