Hairy cell leukemia is a rare disease comprising about 2% of lymphoid neoplasms.1 This neoplasm can be confused with other hematologic diseases. Therefore, a differential diagnosis must be performed between classic hairy cell leukemia, hairy cell leukemia variant, and splenic marginal zone lymphoma (SMZL).2 According to the World Health Organization (2008), hairy cell leukemia variant was classified as a provisional entity because it has clinical and pathological features that differ from classic hairy cell leukemia.3 Among these aspects are morphological and immunophenotypic variations and resistance to conventional treatment.1 Furthermore, patients with hairy cell leukemia are treated with nucleoside analogs but these drugs have a reduced response in hairy cell leukemia variant and are even ineffective in some cases.3,4 An alternative for these patients is the association of nucleoside analogs with the monoclonal antibody rituximab (anti-CD20).5 Thus, due to differential treatment, the aim of this study was to report a case of hairy cell leukemia variant and cover some aspects related to the differential diagnosis between the classic and variant forms of the disease and SMZL. This study was approved by the Research Ethics Committee of the Universidade Federal de Santa Catarina (#913/2010).
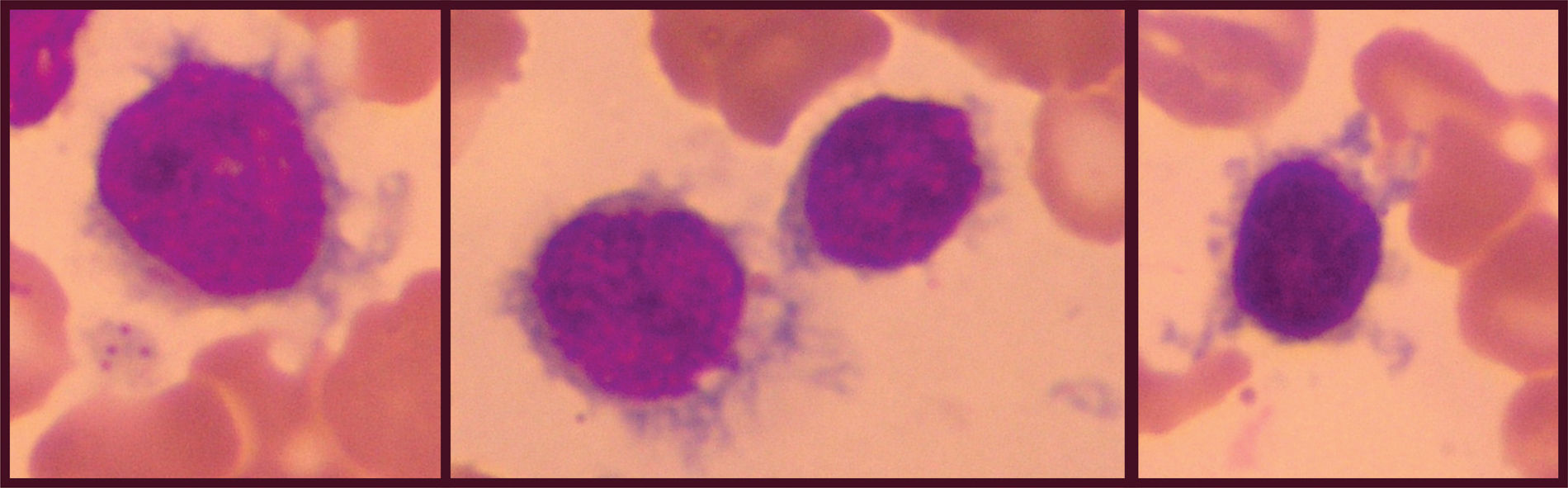
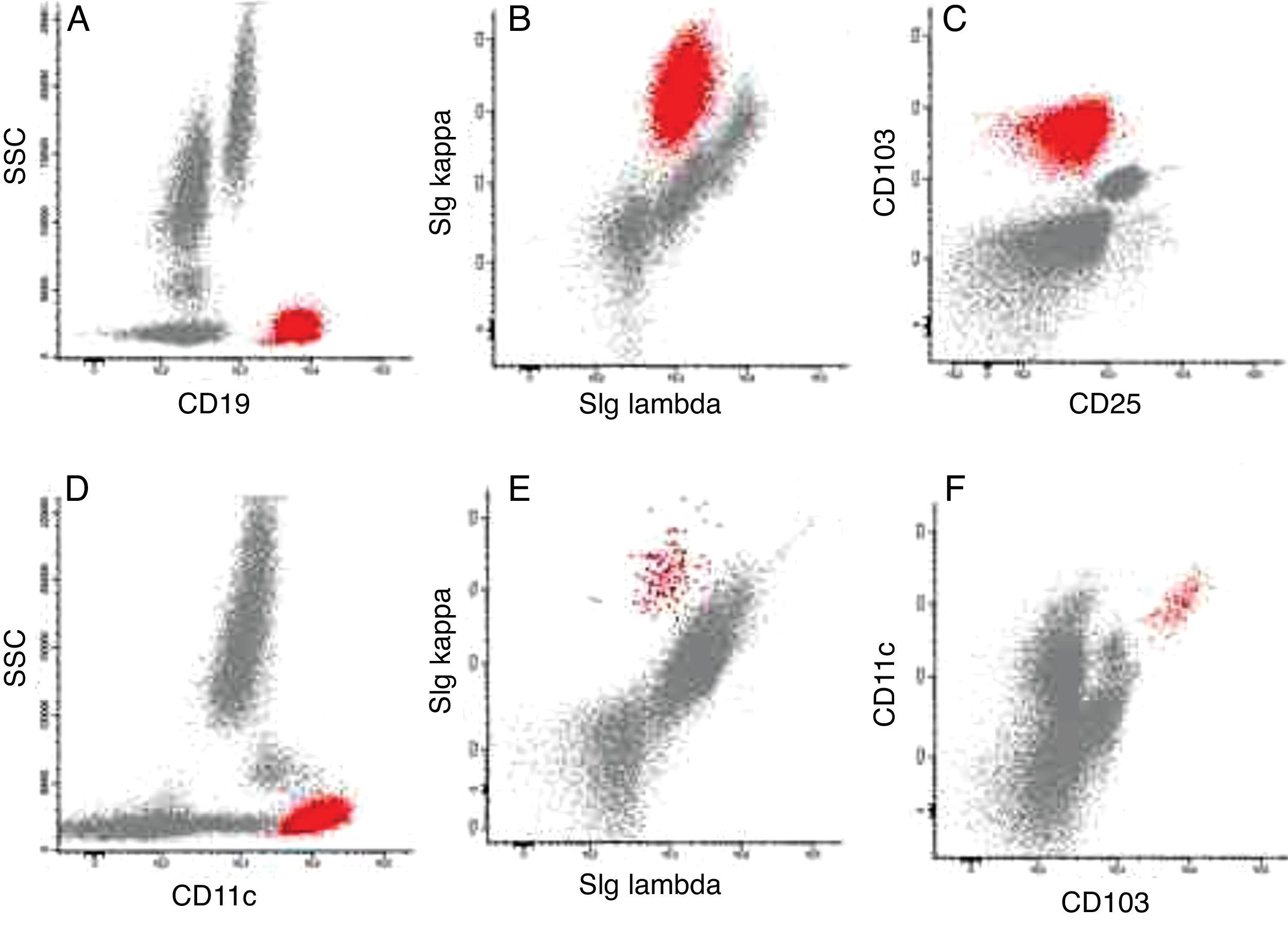
Case reportThe case of a 74-year-old male patient is reported. The presence of splenomegaly was observed since 2011, with areas of infarction in the splenic periphery evidenced by cholangiography and computed tomography. In 2012, due to the persistence of splenomegaly, a complete blood count and immunophenotyping by flow cytometry were requested. At this time, there was no lymphadenopathy. The blood count showed alterations in red blood cells (poikilocytosis, acanthocytes and squizocytes), anemia (hemoglobin 10.1g/dL), thrombocytopenia (100×103/mL), and mild leukocytosis (11.03×103/mL). A white blood cell differential revealed the following: 2.86×103neutrophils/mL (25.9%), 4.67×103lymphocytes/mL (42.3%), 1.16×103monocytes/mL (10.5%), 1.73×103eosinophils/mL (15.7%), 0.07×103basophils/mL (0.6%) and 0.55×103lymphocytes/mL (5.0%) with cytoplasmic projections (Figure 1). Immunophenotyping of peripheral blood (Figure 2) showed 23.2% of B lymphocytes (CD19+), monoclonal (sIg Kappa+), CD103+, CD11c+, CD20++, CD22+, IgM+/++ FMC7++, CD79b++, BCL2+ and no expression of sIg Lambda, CD3, CD4, CD5, CD8, CD10, CD23, CD24, CD25, CD27, CD38, CD43, and CD123. Assessment of sIgD, sIgG, and sIgA expression on the pathological lymphocytes was not performed. The bone marrow was not evaluated and staging was not performed during diagnosis. The treatment was four intravenous doses of rituximab 600mg. After the first dose, the patient was discharged and the response was monitored in the outpatient clinic. At the end of the treatment, the patient returned to the hospital and underwent a bone marrow aspiration for immunophenotyping, myelogram, and immunohistochemistry. Immunophenotyping showed 1.1% of B lymphoid cells with a similar phenotype to that found at diagnosis (Figure 2). The myelogram showed hypercellularity for the age, normal myeloid:erythroid ratio, as well as normality for all other myelogram parameters. Immunohistochemistry revealed aggregates of small lymphocytes CD20+ and DBA44−/+ and the result of TRAP staining was indeterminate. Currently, the patient is being treated in the outpatient clinic and undergoes periodic laboratory tests to monitor the disease.
Representative dot plots of peripheral blood immunophenotyping. (A) Pathological cells (red) CD19+ at diagnosis; (B) pathological cells (red) sIg Kappa+ and sIg Lambda− at diagnosis; (C) pathological cells (red) CD103+ and CD25− at diagnosis; (D) pathological cells (red) CD11c+ at diagnosis; (E) pathological cells (red) sIg Kappa+ and sIg Lambda− in minimal residual disease; (F) pathological cells (red) CD103+ and CD11c+ in minimal residual disease.
Classic hairy cell leukemia, hairy cell leukemia variant, and SMZL share some common features, including malignant lymphocytic infiltration in bone marrow and peripheral blood, splenomegaly, and B lymphocytes with a similar immunophenotype.5 Unlike classic hairy cell leukemia, the variant form affects older individuals.1
Anemia and/or thrombocytopenia and leukocytosis are common at diagnosis of hairy cell leukemia variant, while pancytopenia, granulocytopenia, and monocytopenia are more common in classic hairy cell leukemia. The patient in this study presented with anemia, thrombocytopenia, and mild leukocytosis due to monocytosis, eosinophilia and the presence of pathological lymphocytes.
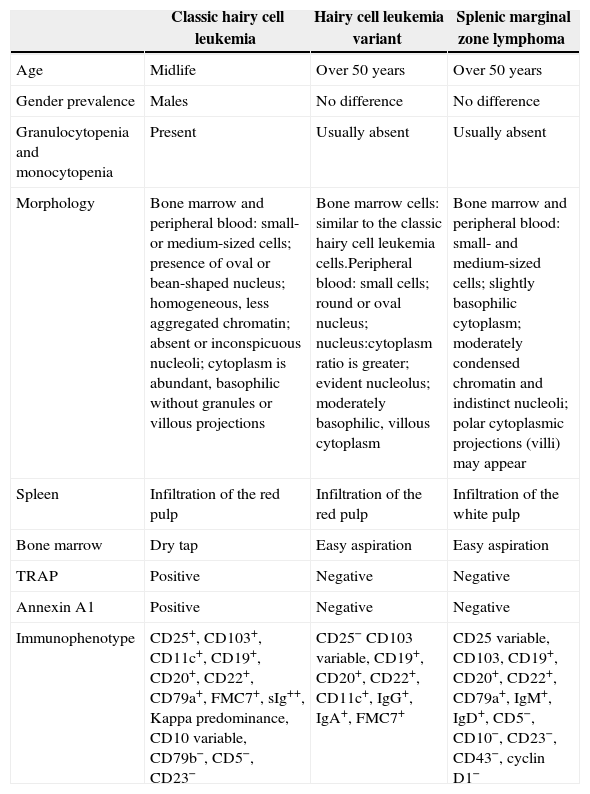
Immunophenotyping by flow cytometry contributes to differential diagnosis, although it must also be associated with immunohistochemistry and clinical data (Table 1). Classic hairy cell leukemia cells are always positive for CD25 and CD103 and hairy cell leukemia variant cells are always negative for CD25 and occasionally positive for CD103. In SMZL, on the other hand, CD103 is negative and CD25 may be positive or negative.3,5 Classic hairy cell leukemia and the variant form are also differentiated by the expression of CD123, which is positive in the classic form and negative in the variant form.6 Evaluation of immunoglobulin heavy chain isotype expression is another way to possibly differentiate hairy cell leukemia variant from SMZL. An unusual feature of hairy cell leukemia variant, not typically observed in other B-cell lymphoproliferative disorders, is the expression of pre-switched IgM/IgD and post-switched IgG/IgA immunoglobulins by the same cells in approximately 40% of cases. In contrast, SMZL cells characteristically express IgM with IgD and lack IgG or IgA.7 Unfortunately in this case the IgG, IgA and IgD immunoglobulins were not available for evaluation. Thus, the results of immunophenotypic analysis of peripheral blood here were consistent with hairy cell leukemia variant.
Comparison between classic hairy cell leukemia, hairy cell leukemia variant, and SMZL.
| Classic hairy cell leukemia | Hairy cell leukemia variant | Splenic marginal zone lymphoma | |
|---|---|---|---|
| Age | Midlife | Over 50 years | Over 50 years |
| Gender prevalence | Males | No difference | No difference |
| Granulocytopenia and monocytopenia | Present | Usually absent | Usually absent |
| Morphology | Bone marrow and peripheral blood: small- or medium-sized cells; presence of oval or bean-shaped nucleus; homogeneous, less aggregated chromatin; absent or inconspicuous nucleoli; cytoplasm is abundant, basophilic without granules or villous projections | Bone marrow cells: similar to the classic hairy cell leukemia cells.Peripheral blood: small cells; round or oval nucleus; nucleus:cytoplasm ratio is greater; evident nucleolus; moderately basophilic, villous cytoplasm | Bone marrow and peripheral blood: small- and medium-sized cells; slightly basophilic cytoplasm; moderately condensed chromatin and indistinct nucleoli; polar cytoplasmic projections (villi) may appear |
| Spleen | Infiltration of the red pulp | Infiltration of the red pulp | Infiltration of the white pulp |
| Bone marrow | Dry tap | Easy aspiration | Easy aspiration |
| TRAP | Positive | Negative | Negative |
| Annexin A1 | Positive | Negative | Negative |
| Immunophenotype | CD25+, CD103+, CD11c+, CD19+, CD20+, CD22+, CD79a+, FMC7+, sIg++, Kappa predominance, CD10 variable, CD79b−, CD5−, CD23− | CD25− CD103 variable, CD19+, CD20+, CD22+, CD11c+, IgG+, IgA+, FMC7+ | CD25 variable, CD103, CD19+, CD20+, CD22+, CD79a+, IgM+, IgD+, CD5−, CD10−, CD23−, CD43−, cyclin D1− |
In immunohistochemistry, DBA44 provides strong staining for lymphocytes with cytoplasmic projections in tissues; however, it may also be present in normal B cells.3 Moreover, cells from hairy cell leukemia variant patients rarely show TRAP reactivity (unlike the classic form).1 In the patient of this study, TRAP staining remained indeterminate; hence, it did not help in the diagnosis. The morphology and phenotype confirmed the diagnosis of hairy cell leukemia variant.
When the patient returned to the hospital of the Universidade Federal de Santa Catarina (HU-UFSC) at the end of treatment, the myelogram was hypercellular for his age, but this alteration has no clinical relevance to his condition. The presence of 1.1% of cells with a phenotype similar to that found at diagnosis, as evidenced by immunophenotyping of a bone marrow aspirate, indicates the presence of minimal residual disease (MRD). MRD is present in many patients treated for hairy cell leukemia; however, these patients may have long-term survival. Treatment with Rituximab is used to achieve complete remission, although the response is dependent on how much bone marrow is involved and on the characteristics of the individual.8
ConclusionHairy cell leukemia variant is a chronic lymphoproliferative disorder whose characteristics resemble the classic form and SMZL, making differential diagnosis essential for therapeutic follow-up, as hairy cell leukemia variant has a decreased response to drugs prescribed for the classic form. Immunophenotyping is a key tool for diagnosis, as some markers are different between these neoplasms. Therefore, immunophenotyping, clinical, morphological, and immunohistochemical manifestations must be considered in the differential diagnosis.
Conflicts of interestThe authors declare no conflicts of interest.