Erythrocyte phenotyping is a very important test in the adoption of prophylactic measures to reduce transfusion reactions/alloimmunizations in polytransfused patients. The blood group Diego, in its current, form has 22 antigens, of which 4 are immunogenic, being Diª/Dib and Wra/Wrb, while the others are less expressive. The antigen Diª is of low incidence among whites and blacks, however, it is common in the South American indigenous and Asian Mongolian populations. It is also considered a system of clinical importance for its immunogenicity.
MethodThe present study aimed to carry out a retrospective and descriptive survey of the frequency of the Diª antigen in the blood donor population at the HEMOPA Foundation Coordinating Blood Center from 12/2018 to 1/2000. The data obtained were from the HEMOPA Foundation SBS Progress and SBS WEB Systems databases.
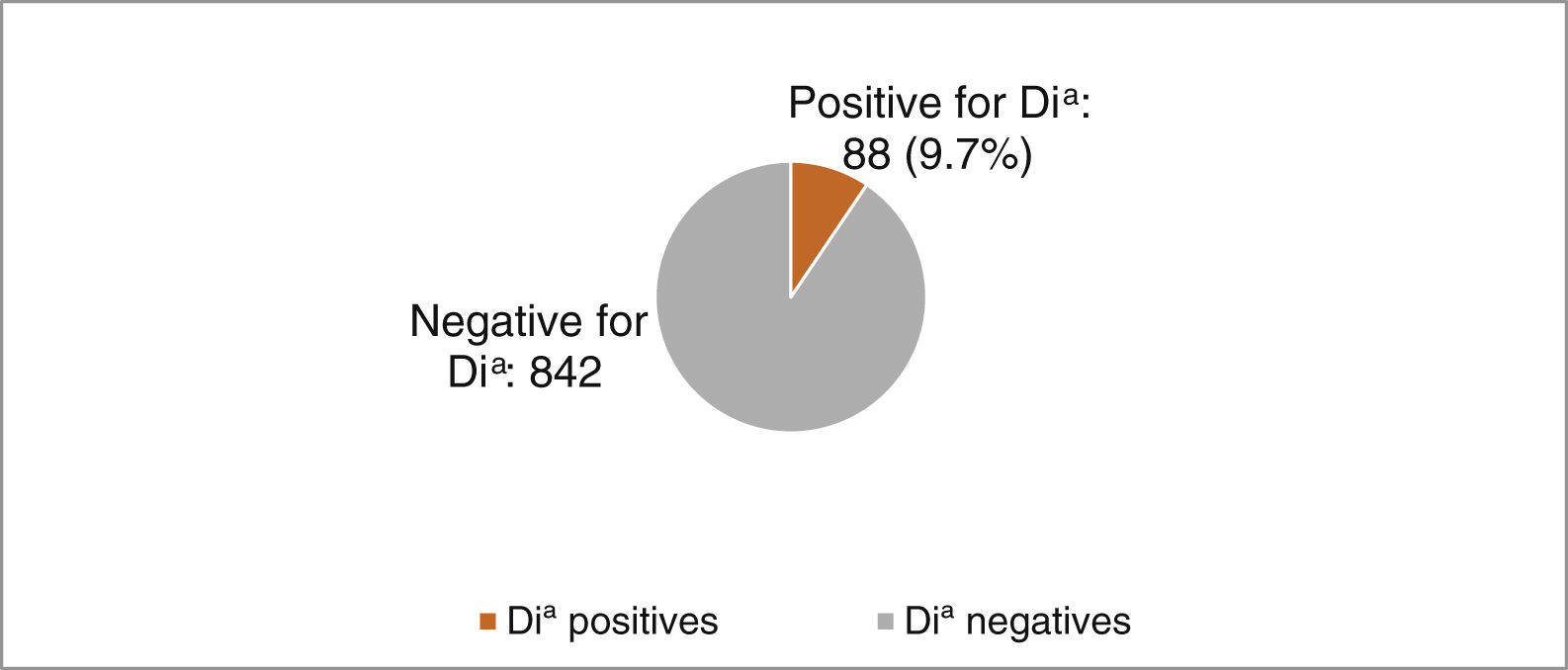
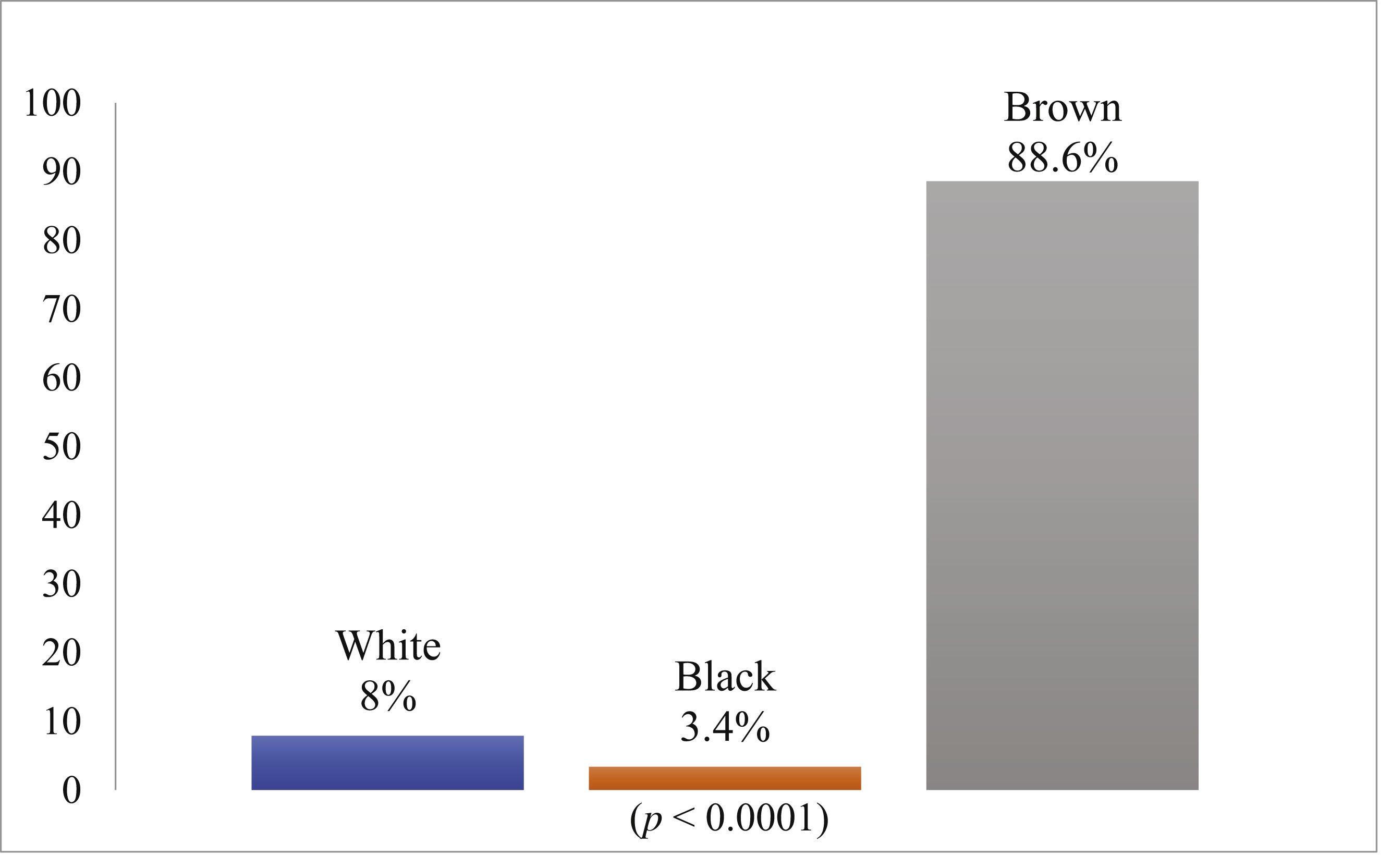
ResultsDuring this period, 941,744 blood bags were collected and, of these, 930 bags were phenotyped for the Diª antigen, of which 842 were negative and 88 (9.7%) positive. The research showed that, among the positive donors for the antigen Diª, 88.6% were brown, 3.4%, black and 8%, white. In the statistical analysis, the frequency observed was higher in browns.
ConclusionIn the present investigation, we concluded that our region has a relatively higher frequency of the Diª antigen, when compared to the rest of Brazil, and it occurs more often in browns.
Erythrocyte phenotyping is a very important test in the adoption of prophylactic measures to reduce transfusion/alloimmunization reactions and consists of the identification of antigens present in red blood cells tested with sera that have the respective antibodies and stimulate the formation of alloantibodies, especially in pregnant women and patients who will be subjected to polytransfusion. This technique is used to prevent transfusion reactions and the late emergence of antibodies, allowing for the use of an antigenically compatible blood component, being essential for the confirmation of already formed alloantibodies and facilitating the identification of those that may arise in the future1,2.
The Consolidation Ordinance No. 5/2017 of the Ministry of Health, Art. 121, Annex IV advocates the screening of irregular anti-erythrocyte antibodies in donor blood through methods that make evident the presence of clinically significant antibodies3.
The Diego Blood Group System (The International Society of Blood Transfusion, or ISBT) is a clinically important system that was first described by Miguel Layrisse in Venezuela in 1955, when he and colleagues studied a family of indigenous descent, of which Mrs. Diego, in her first record following the detection of the corresponding antibody in her serum, which caused a hemolytic reaction in her newborn, and named it after her4,5,6.
The Diego system in its current form is composed of 22 antigens distributed in 16 antigenic sites, located in the integral band 3 glycoprotein in the erythrocyte membrane and two closely related antigen pairs, Dia/Dib and Wra/Wrb. Of these, Dib and Wrb are the most frequent, while Dia and Wra have a low incidence. For an individual to have a Diego antigen pair, there is a possibility of three different genotypes, Di (a-b+), Di (a + b+) and Di (a + b-). As it is an irregular blood group, it was initially considered to be a particular family factor, but after further studies its highest incidence was found to be among South American and Asian Indians, especially those of Mongol origin, and came to be seen as a genetic marker for this ethnicity7,1,5.
The replacement of Proline (Dib) with Leucine (Dia) occurs in the SLC4A1 gene (Solute Carrier Family 4/Anion Exchanger 1) at position 854, located on chromosome 17, which transcribes an anion carrier protein and is an integral part of the red cell membrane. This protein helps anchor the membrane to the spectrin skeleton, which makes the erythrocyte stable and flexible, and to biconcave red blood cells, as well as encodes and gives rise to the band 3 protein, expressed on the surface of the erythrocytes8.
The antigens Dia and Dib are significantly involved in cases of hemolytic disease of the newborn (NRD) and most cases are related to pregnancy due to maternal fetus incompatibility, in which both antibodies produced are of the IgG1 and IgG3 class. Anti-Dia antibodies developed in pregnant women are mainly caused by her sensitization at birth, when the fetus Dia antigens reach the mother's circulation, possibly inducing an immune response. They are also involved in post-transfusion reactions in recipients when they receive an incompatible red blood cell transfusion9,10.
The Dia antigen also has as one of its features the possibility of being present as a natural immune response, thus causing an immediate hemolytic reaction11.
The alloimmunization by erythrocyte antigens of the Diego system often goes unnoticed when there are no transfusion reactions or fatal hemolytic diseases in newborns or until they are detected in patients. This leads to questioning what percentage of the population is exposed to these antigens in an unknown way. This is because the routine antigen screening procedure at Blood Banks does not usually include the phenotyped red blood cell reagents10,11.
In the study by Sanguino et al.12 at the Amazonas Hematology and Hemotherapy Foundation (FHEMOAM) in Manaus, a total of 302 non-indigenous donors who were eligible for blood donation were investigated. The result of this study showed a frequency of the Di allele three times higher than that of other Brazilian regions, being considered similar to that of the Asian populations.
Komatsu et al.13 point out in their study that the frequency of the Dia antigen among Mongols may be the same as that among Japanese, which leads to the presumption that these populations possibly derive from a common racial ancestor and that the Di antigen tends to show an ethnic variation across its prevalence, unlike the Dib antigen.
Currently, the Dia antigen polymorphism occurs with a high frequency in Venezuelan Indians, with an estimated 36% of the cases. In the Japanese population, the frequency ranges from 8 to 12% and in the Chinese, from 25 to 32%. In contrast, the Dia antigen remains rare in whites and Africans, as shown in a study in Poland with 9661 donors, of whom only 45 expressed this antigen12.
Brazilians form one of the most diverse populations in the world and research on genetic variability and blood group systems has already been conducted and demonstrated this heterogeneity14.
Migration over time has contributed to a high rate of miscegenation, making the Brazilian population unique in anthropology. There is a large number of data in the country regarding the study of erythrocyte phenotypes in the population, especially those related to the ABO, Rh (D) and related systems. However, knowledge of the frequency of antigens from other blood group systems is essential in the estimation of the amount of compatible blood for patients, with the respective erythrocyte antigens, and in the identification of possible donors with rare phenotypes15.
The correct detection of the blood group in hemotherapy is important, not only for the prevention of further problems in incompatible transfusions, but also to allow for the proper use of blood with lower incidence phenotypes, thus ensuring a safe transfusion16.
This research aimed to conduct a retrospective and descriptive study of the frequency of antigen Diapositive blood donors at the HEMOPA Foundation of Blood Donors in the state capital, Belém, to demonstrate its prevalence in the Brazilian northern region, which may have higher rate due to the Pará offspring, as well as to demonstrate the transfusion risks related to this antigen, making its detection is of great importance in the transfusion practice, as its association with antibody development can render it clinically significant. It is well known that to date there is no research published in the literature on this topic at the HEMOPA Foundation.
MethodsA retrospective study of the Dia antigen erythrocyte phenotyping was performed on samples from healthy volunteer blood donors of both sexes attended to at the Coordinating Hemocenter of the HEMOPA Foundation from 12/2018 until 1/2000 through quantitative analysis by the programs of the databases SBS PROGRESS and SBS WEB.
The inclusion criteria for the phenotyping of donors/grants at the HEMOPA Foundation were: second-donation donor or donor of at least two donations; permanent resident of the metropolitan area of Belém, and; history of negative serology and normal hemoglobin electrophoresis.
The ethnicity/race variables were self-declared by donors at the time of screening and subsequently analyzed qualitatively through individual registration in the same programs mentioned.
The data obtained was tabulated on a spreadsheet of the Microsoft Excel 2010 program for further analysis of the results.
The statistical test used to compare the results was the Chi-square in the Bioestat 5.0 program.
This study was submitted to the HEMOPA Foundation Center for Teaching and Research (NEPES) and the Plataforma Brasil, a national and unified database of research involving human beings for the entire CEP/Conep system, in compliance with Resolution No. 466/2012 of the National Health Council, which deals with guidelines and regulatory standards for research involving human subjects.
The researched data refer to the results of the low frequency antigen phenotyping technique with the ID-Seros-Test for the indirect antiglobulin test (TAI) with the ID-Card “LISS/Coombs”, which is already held at the HEMOPA Foundation and is regulated by the Consolidation Ordinance No. 5/2017, Ministry of Health Annex IV of September 28, 2017.
The manufacturer's specifications read: the ID-Seros Bio-Rad Tests used in the indirect antiglobulin (TAI) test with the ID-Card “LISS/Coombs” are human antisera lyophilized in 0.5 mL vials containing incomplete antibodies available for the antigens Dia and Wra.
According to the manufacturer's instructions for the test, blood samples are initially prepared with a 0.8% red cell suspension in ID-Diluent 2, upon which the laboratory technician should: 1) Dispense 1.0 mL of the ID-Diluent 2 in the suspension tube; 2) Pipette 10–12.5 µL of packed red blood cells or 25 µL whole blood, and; 3) Homogenize.
The red cell suspension can be used immediately.
The ID-Soros Test content should be reconstituted with distilled water and thoroughly mixed. Shelf life after dilution is 8 days at 2–8 °C.
In performing the research, positive and negative samples should be included, according to the quality control standards.
With the red blood cell suspension already prepared and the antiserum diluted, appropriate microtubes should be identified with the donor and antigen name to be identified, then the red blood cell suspension gently resuspended and 50 µL of ID-Serum is pipetted. The test corresponding to the antigen to be screened in the microtube should be performed, after which the ID-Card is incubated for 15 min at 37 °C and finally centrifuged for 10 min before reading the result.
For samples with positive results, agglutinated cells are observed forming a red line on the surface or along the gel. Positive reactions from 1+ to 4+ indicate the presence of the antigen.
In the absence of an antigen-antibody reaction, a compact red cell button will be observed at the bottom of the microtube, which characterizes a negative result.
ResultsDonations were collected at the Foundation HEMOPA from 12/2018 to 1/2000 from the database records of the SBS PROGRESS and SBS WEB programs, which showed 941,744 collected bags in the period. Of these, 930 bags were phenotyped for the Diª antigen, of which 842 were negative and 88, positive (9.7%) (Fig. 1).
The survey showed that, among the positive donors for the antigen Diª, 88.6% were self-declared brown (Amerindians + whites), 3.4%, black and 8%, white. In the statistical analysis, the frequency observed was higher in browns (x 2 = 103.144; p < 0.0001) (Fig. 2).
The research showed that, among the negative donors for the Diª antigen, 77% were self-declared brown, 4%, black and 19%, white. In the statistical analysis of the antigen frequency comparison between positive and negative donors, it was observed that there was no significant difference in relation to self-declared ethnicity/race (Table 1).
DiscussionThere are currently several techniques available for the study of blood groups in hemotherapy services, such as hemagglutination. However, to date, not all of them are used in routine donor blood screening, being applied only in special cases in which there must be an investigation or in small populations. This is mainly due to the high cost and, in some situations, to the complexity of the technique and the non-requirement by the legislation that regulates Brazilian hemotherapy services15.
Blood bank screening routines are not able to detect all the antigens of blood group systems due to the difficulty in antisera specifics. This problem we encounter when we refer to the Dia antigen because prior detection is not simple due to the unavailability of antiserum, as it does not have an accessible cost-benefit, nor short-term validity or sufficient volume for large-scale tests17,18.
In a study conducted by Baleotti Júnior (2002)19, using the techniques of erythrocyte phenotyping, molecular biology and electrophoresis, with 318 individuals, who were divided into four groups, being 93 blood donors, 71 Japanese descendants, 84 African descendants and 70 blood samples from Indians belonging to the Parakanã tribe of the state of Pará and, of these 93 donor samples, only 3 (3.2%) had a homozygous genotype, while 90 (96.8%) were heterozygous. Among the samples of African descendants, no homozygote was found for the Dia antigen and just one heterozygote. In the Japanese, only one was homozygous and 7% were heterozygous. This demonstrated that the frequency of the Dia allele found in the indigenous population (75.7%) was higher than the frequency found in other groups. This frequency among the indigenous people was higher than the last recorded one of 46% in the indigenous Kaigangues in Palmas, Paraná. This research demonstrated a close relationship between the Dia phenotype and indigenous and Asian populations. Balleoti Júnior's (2002)19 comparative analysis between Dia and Dib alleles demonstrates the significant difference among donors, indigenous and other populations of ethnic groups, except Japanese, assuming they have common ancestors, also highlighting the low frequency of the Dia allele in blacks and Japanese, when taken compared to the indigenous population.
According to the data from the demographic census conducted by the IBGE (Brazilian Institute of Geography and Statistics) in 2010, the current indigenous population of Brazil totals 896,900 people, the highest concentration being in the North, with about 342.8 thousand, while in the South, 78.8 thousand. Additionally, according to the census, 36.2% live in urban areas and 63.8%, in rural areas. Of the total, 817.9 thousand were classified in terms of color or race, of whom 78.9 thousand resided in indigenous lands and declared themselves of another color or race, mainly browns, 67.5%, declaring themselves “indigenous” by tradition, customs or ancestors20.
In the present investigation, the frequencies observed among positive donors were different in white groups (8%), browns (88.6%) and blacks (3.4%). In fact, the frequency is higher in browns, which was statistically proven (x2 = 103.114; p < 0.0001). This result contrasts with another investigation performed in the state of Paraná, in the southern region, with 251 blood donors, of which 88% were white, 1%, black and only 4%, brown. Of these, only one was Dia positive, which resembles another investigation performed in Santa Catarina, which presented a similarity in the Diego system polymorphism. This can be justified due to the genetic parity between the two states, the highest concentration of browns considered indigenous being in the North of Brazil, when compared to other regions, especially the South, which presents a low indigenous influence. This population characteristic is similar to that of previous studies that found the highest frequency of the Dia antigen in native South American Indians16,20,21.
In this research, the positive donors found (9.7%) were higher in number than those from other studies done in Tokyo, North China and Chinese Koreans that had a prevalence of 8.78%, 8.53% and 7.87%, respectively (Table 2)13.
Comparative analysis of the frequency of the Dia antigen.
| Author/ Year | Researched group | N Total | Frequency Diª (%) |
|---|---|---|---|
| Baleotti Júnior, 2002 | Blood donor | 93 | 3 (3.2%) homozygous 0 (0%) heterozygous |
| Descendants of Japanese | 71 | 1 (1%) homozygous e 8 (7%) heterozygous | |
| Descendants of Africans | 84 | 0 (0%) homozygous and 1 (1.2%) heterozygous | |
| Indians of the Parakanã Tribe | 70 | 27 (38.5%) homozygous and 26 (37.14%) heterozygous | |
| Zacarias et al., 2016 | Brown | 10 | 1 (1%) homozygous and 10 (3.9%) heterozygous (both undetermined by the author as to ethnicity) |
| White | 221 | ||
| Black | 3 | ||
| Did not declare ethnicity | 17 | ||
| Komatsu et al., 2004 | Tokyo | 5822 | 511 (8.78%) homozygous |
| Northern China | 211 | 18 (8.53%) homozygous | |
| Chinese-Korean | 216 | 17 (7.87%) homozygous | |
| Current research | Brown | 74 | 74 (88.6%) homozygous |
| White | 11 | 11 (8%) homozygous | |
| Black | 3 | 3 (3.4%) homozygous |
Source: Author data (2019).
In addition to the international immigration to Brazil, the emergence of a population hybrid through family crossing can be associated with the great diversity in the country, as it was strongly influenced by the immigration movement, making it ethnically very heterogeneous. These aspects rendered the population of Central Thailand, compared to other populations, highly related to that of Brazil, especially the Southern region of Brazil, as shown in a recent study. The frequency of the Dia antigen between the two countries is also similar (3.32%)8.
As for the relationship between indigenous populations in Brazil, the Dia antigen is currently found more frequently in the Parakanã tribe than in the Kaigangues tribe in Paraná, which presented the highest frequency in the last published investigation19,17.
The self-declared brown donors of this research, who tested negative for the Diª antigen (77%), possibly come from a familial genetic cross between whites and blacks, or there had been a possible change in skin color due to the climatic factors in the northern region that may have influenced the self-declaration of ethnicity/race of these donors.
Serological studies demonstrate that there is no Dia antigen in pure Americans and it is extremely rare in Africans and Europeans, thus demonstrating the miscegenation of our population with the indigenous and Japanese populations19.
According to Delaney et al.22, recent evidence confirms that even blood transfusions, compared by race and/or ethnicity in the population with sickle cell disease, do not protect against allosensitization and that the combination of genotypes can further improve results of polytransfused patients.
In blood banks, the knowledge of the prevalence of blood group antigens is important to meet the transfusion needs of all patients in the population it serves and, therefore, they must be prepared for opportune or low-occurrence cases22. In addition, we suggest the inclusion of the Diego antigen research in the erythrocyte phenotyping panel, as it is not required by the current blood therapeutics legislation.
ConclusionIn the present investigation, we concluded that in our region we have a relatively higher frequency of the Diª antigen, when compared to the rest of Brazil, and it is present in a higher form in self-declared brown donors. Self-declared brown donors who tested negative for the antigen may be from a familial genetic cross between whites and blacks, or there had been a possible change in skin color due to climatic factors in the northern region, which may have influenced the self-declaration of ethnicity/race of these donors.
The data obtained from this research enabled us to better understand the blood donor population of the HEMOPA Foundation, as well as to dimension the frequency of the Dia antigen in the North of Brazil, that we had not yet studied.
Brazilian blood centers should contemplate the regional characteristics of the country because, in addition to the common antigens, some rare or low-frequency ones, such as the Dia, are immunogenic and may be responsible for alloimmunizations and post-transfusion reactions dependent on patient awareness and may result in severe hemolytic response, mainly in polytransfused patients.